Abstract
Background
Phyllodes tumours of the breast are rare fibroepithelial neoplasms with a propensity for recurrence. While surgical excision remains the standard of care, the optimal margin width is an area of active investigation. Recent studies have questioned the necessity for wide, local excision.
Methods
We conducted a retrospective, cohort study of patients with phyllodes tumours treated at our institution between 2003 and 2021. Demographic, histopathological, and recurrence data were captured; malignant phyllodes were excluded. Cox proportional hazard models were used to identify covariates associated with local recurrence.
Results
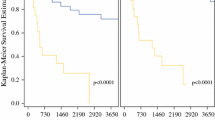
Of 187 patients with phyllodes tumours, 82.9% (n = 155) were classified as benign while 17.1% (n = 32) were borderline. Initial surgical margins were positive in 26.2% (n = 49), < 2 mm in 50.8% (n = 95), and ≥ 2 mm in 23% (n = 43) patients. Among patients with positive margins, 61.2% (n = 30) underwent margin revision. At a median follow-up of 2.9 years, the recurrence rate was 3.7%. On univariate analysis, only a positive margin at the time of initial surgery and not margin width was significantly associated with a higher rate of disease recurrence (hazard ratio [HR] 9.52, 95% confidence interval [CI] 1.85–49.2), as was a size greater than 4 cm on preoperative imaging (HR 10.78, 95% CI 0.97–120.1). Revision of an initially positive margin was not significantly associated with decreased local recurrence (p = 1).
Conclusions
In this large cohort of benign and borderline phyllodes tumours, positive resection margins and not margin width at the initial surgery were associated with a increased recurrence. Individualization of decisions regarding margin reexcision is important.




Similar content being viewed by others
References
Ang MK, Ooi AS, Thike AA, et al. Molecular classification of breast phyllodes tumors: validation of the histologic grading scheme and insights into malignant progression. Breast Cancer Res Treat. 2011;129(2):319–29.
Tan BY, Acs G, Apple SK, et al. Phyllodes tumours of the breast: a consensus review. Histopathology. 2016;68(1):5–21.
Lakhani SREI, Schnitt SJ, et al. World health organization classification of tumours of the breast. Lyon, France: IARC; 2012.
Tan PH, Ellis I, Allison K, et al. The 2019 world health organization classification of tumours of the breast. Histopathology. 2020;77(2):181–5.
Johnson HM, Mohamed A, Hassan MM, Geradts J, Geisel L, Vohra NA, Wong JH. Race-related differences in the clinical presentation and histopathologic features of phyllodes tumor. Am Surg. 2021. https://doi.org/10.1177/00031348211029841.
Choi J, Koo JS. Comparative study of histological features between core needle biopsy and surgical excision in phyllodes tumor. Pathol Int. 2012;62(2):120–6.
Parker SJ, Harries SA. Phyllodes tumours. Postgrad Med J. 2001;77(909):428–35.
Chua CL, Thomas A, Ng BK. Cystosarcoma phyllodes: a review of surgical options. Surgery. 1989;105(2 Pt 1):141–7.
Reinfuss M, Mitus J, Duda K, Stelmach A, Rys J, Smolak K. The treatment and prognosis of patients with phyllodes tumor of the breast: an analysis of 170 cases. Cancer. 1996;77(5):910–6.
Zurrida S, Bartoli C, Galimberti V, et al. Which therapy for unexpected phyllode tumour of the breast? Eur J Cancer. 1992;28(2–3):654–7.
Kapiris I, Nasiri N, A’Hern R, Healy V, Gui GP. Outcome and predictive factors of local recurrence and distant metastases following primary surgical treatment of high-grade malignant phyllodes tumours of the breast. Eur J Surg Oncol. 2001;27(8):723–30.
Moo TA, Alabdulkareem H, Tam A, et al. Association between recurrence and re-excision for close and positive margins versus observation in patients with benign phyllodes tumors. Ann Surg Oncol. 2017;24(10):3088–92.
Ouyang Q, Li S, Tan C, et al. Benign phyllodes tumor of the breast diagnosed after ultrasound-guided vacuum-assisted biopsy: surgical excision or wait-and-watch? Ann Surg Oncol. 2016;23(4):1129–34.
Spitaleri G, Toesca A, Botteri E, et al. Breast phyllodes tumor: a review of literature and a single center retrospective series analysis. Crit Rev Oncol Hematol. 2013;88(2):427–36.
Rosenberger LH, Thomas SM, Nimbkar SN, et al. Contemporary multi-institutional cohort of 550 cases of phyllodes tumors (2007–2017) demonstrates a need for more individualized margin guidelines. J Clin Oncol. 2021;39(3):178–89.
Shaaban M, Barthelmes L. Benign phyllodes tumours of the breast: (Over) treatment of margins: a literature review. Eur J Surg Oncol. 2017;43(7):1186–90.
Genco IS, Purohit V, Hackman K, Ferreira L, Tugertimur B, Hajiyeva S. Benign and borderline phyllodes tumors of the breast: Clinicopathologic analysis of 205 cases with emphasis on the surgical margin status and local recurrence rate. Ann Diagn Pathol. 2021;51:151708.
National Comprehensive Cancer Network. Breast Cancer (Version 8.2021). https://www.nccn.org/professionals/physician_gls/pdf/breast.pdf. Accessed October 16, 2021.
Nair NS, Chitkara G, Hawaldar RW, et al. En bloc excision of phyllodes tumor of the breast: radical approach heralds better outcome. Clin Breast Cancer. 2021;21(3):e228–34.
Toussaint A, Piaget-Rossel R, Stormacq C, Mathevet P, Lepigeon K, Taffe P. Width of margins in phyllodes tumors of the breast: the controversy drags on? A systematic review and meta-analysis. Breast Cancer Res Treat. 2021;185(1):21–37.
Lu Y, Chen Y, Zhu L, et al. Local recurrence of benign, borderline, and malignant phyllodes tumors of the breast: a systematic review and meta-analysis. Ann Surg Oncol. 2019;26(5):1263–75.
Wei Y, Yu Y, Ji Y, et al. Surgical management in phyllodes tumors of the breast: a systematic review and meta-analysis. Gland Surg. 2022;11(3):513–23.
Network NCC. 2018
Rodrigues MF, Truong PT, McKevitt EC, Weir LM, Knowling MA, Wai ES. Phyllodes tumors of the breast: the British columbia cancer agency experience. Cancer Radiother. 2018;22(2):112–9.
Chng TW, Gudi M, Lim SH, Li H, Tan PH. Validation of the Singapore nomogram for outcome prediction in breast phyllodes tumours in a large patient cohort. J Clin Pathol. 2018;71(2):125–8.
Sotheran W, Domjan J, Jeffrey M, Wise MH, Perry PM. Phyllodes tumours of the breast–a retrospective study from 1982–2000 of 50 cases in Portsmouth. Ann R Coll Surg Engl. 2005;87(5):339–44.
Tremblay-LeMay R, Hogue JC, Provencher L, et al. How wide should margins be for phyllodes tumors of the breast? Breast J. 2017;23(3):315–22.
Jang JH, Choi MY, Lee SK, et al. Clinicopathologic risk factors for the local recurrence of phyllodes tumors of the breast. Ann Surg Oncol. 2012;19(8):2612–7.
Koh VCY, Thike AA, Nasir NDM, Yip GWC, Bay BH, Tan PH. Size and heterologous elements predict metastases in malignant phyllodes tumours of the breast. Virchows Arch. 2018;472(4):615–21.
Kim S, Kim JY, Kim DH, Jung WH, Koo JS. Analysis of phyllodes tumor recurrence according to the histologic grade. Breast Cancer Res Treat. 2013;141(3):353–63.
Zhou ZR, Wang CC, Sun XJ, et al. Prognostic factors in breast phyllodes tumors: a nomogram based on a retrospective cohort study of 404 patients. Cancer Med. 2018;7(4):1030–42.
Chen WH, Cheng SP, Tzen CY, et al. Surgical treatment of phyllodes tumors of the breast: retrospective review of 172 cases. J Surg Oncol. 2005;91(3):185–94.
Tan PH, Thike AA, Tan WJ, et al. Predicting clinical behaviour of breast phyllodes tumours: a nomogram based on histological criteria and surgical margins. J Clin Pathol. 2012;65(1):69–76.
Choi JE, Kang SH, Tan PH, Bae YK. Recurrence prediction for breast phyllodes tumours: validation of the Singapore nomogram in Korean women. J Clin Pathol. 2020;75(3):159–63. https://doi.org/10.1136/jclinpath-2020-207093.
Rosenberger LH, Quintana LM, Thomas SM, et al. Limited reporting of histopathologic details in a multi-institutional academic cohort of phyllodes tumors: time for standardization. Ann Surg Oncol. 2021;28(12):7404–9.
Metcalfe LN, Zysk AM, Yemul KS, et al. Beyond the margins-economic costs and complications associated with repeated breast-conserving surgeries. JAMA Surg. 2017;152(11):1084–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
None of the authors has any relevant conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Moldoveanu, D., Iny, E., Theriault, C. et al. Margin Status and Local Recurrence in Phyllodes Tumours of the Breast: A Canadian Series. Ann Surg Oncol 30, 1700–1709 (2023). https://doi.org/10.1245/s10434-022-12894-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-022-12894-2