Abstract
Background
Nodal staging systems (NSS) for pancreatic ductal adenocarcinoma (PDAC) classify patients on the basis of number of metastatic lymph nodes (MLN), metastatic/retrieved lymph node ratio (LNR), and log odds of positive LN (LODDS). The relative prognostic performance of these NSS, however, remains unclear.
Patients and Methods
We identified 2584 patients who underwent surgery for PDAC between 2010 and 2019. Subgroups of each staging system were classified using K-adaptive partitioning method and assessed by comparing time-dependent areas under the curve (AUC) 5 years after surgery.
Results
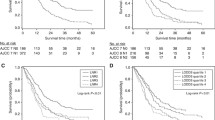
Patients were subgrouped by MLN (0, 1–3, ≥ 4), LNR (0, 0–0.23, > 0.23), and LODDS (< − 3.5, − 3.5 to – 0.970, > − 0.97). All three NSS were independent prognostic factors for overall survival (OS) and recurrence-free survival (RFS). The AUCs for OS were comparable for the MLN (0.622), LNR (0.609), and LODDS (0.596) systems. Subgroup evaluation based on 12 retrieved lymph nodes (RLN), R1 resection, and extent of resection showed that the AUCs of the MLN and LNR NSS were comparable for OS and RFS regardless of the number of RLNs, R1 resection, and extent of resection. By contrast, the AUCs of the LODDS NSS were lower.
Conclusion
The NSS based on the number of MLN is the best prognostic indicator, with prognostic performance comparable to the other NSS and greater convenience for practical use. This NSS was applicable regardless of the numbers of RLN, R1 resection, and extent of resection.

Similar content being viewed by others
References
Kaufmann B, Hartmann D, D’Haese JG, et al. Neoadjuvant treatment for borderline resectable pancreatic ductal adenocarcinoma. Dig Surg. 2018;36:1–7.
Yoo C, Lee SS, Song KB, et al. Neoadjuvant modified FOLFIRINOX followed by postoperative gemcitabine in borderline resectable pancreatic adenocarcinoma: a Phase 2 study for clinical and biomarker analysis. Br J Cancer. 2020;123(3):362–8.
Allen PJ, Kuk D, Castillo CF, et al. Multi-institutional validation study of the American Joint Commission on Cancer changes for T and N staging in patients with pancreatic adenocarcinoma. Ann Surg. 2017;265(1):185–91.
Basturk O, Saka B, Balci S, et al. Substaging of Lymph node status in resected pancreatic ductal adenocarcinoma has strong prognostic correlations: proposal for a revised N classification for TNM staging. Ann Surg Oncol. 2015;22(Suppl 3):S1187-1195.
Amin MB ES, Greene F, Byrd DR, et al. AJCC cancer staging manual, 8th edn. Springer. 2017.
Slidell MB, Chang DC, Cameron JL, et al. Impact of total lymph node count and lymph node ratio on staging and survival after pancreatectomy for pancreatic adenocarcinoma: a large, population-based analysis. Ann Surg Oncol. 2008;15(1):165–74.
Lahat G, Lubezky N, Gerstenhaber F, et al. Number of evaluated lymph nodes and positive lymph nodes, lymph node ratio, and log odds evaluation in early-stage pancreatic ductal adenocarcinoma: numerology or valid indicators of patient outcome? World J Surg Oncol. 2016;14(1):1–8.
Strobel O, Hinz U, Gluth A, et al. Pancreatic adenocarcinoma: number of positive nodes allows to distinguish several N categories. Ann Surg. 2015;261(5):961–9.
You MS, Lee SH, Choi YH, et al. Lymph node ratio as valuable predictor in pancreatic cancer treated with R0 resection and adjuvant treatment. BMC Cancer. 2019;19(1):952.
Morales-Oyarvide V, Rubinson DA, Dunne RF, et al. Lymph node metastases in resected pancreatic ductal adenocarcinoma: predictors of disease recurrence and survival. Br J Cancer. 2017;117(12):1874–82.
Tol JA, Gouma DJ, Bassi C, et al. Definition of a standard lymphadenectomy in surgery for pancreatic ductal adenocarcinoma: a consensus statement by the International Study Group on Pancreatic Surgery (ISGPS). Surgery. 2014;156(3):591–600.
Clavien PA, Barkun J, de Oliveira ML, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250(2):187–96.
Eo SH, Kang HJ, Hong SM, et al. K-adaptive partitioning for survival data, with an application to cancer staging. The Kaps add-on package for R. J Stat Software (in press).
Palumbo A, Avet-Loiseau H, Oliva S, et al. Revised international staging system for multiple myeloma: a report from International Myeloma Working Group. J Clin Oncol. 2015;33(26):2863–9.
Huebner M, Kendrick M, Reid-Lombardo KM, et al. Number of lymph nodes evaluated: prognostic value in pancreatic adenocarcinoma. J Gastrointest Surg. 2012;16(5):920–6.
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69(1):7–34.
Murakami Y, Uemura K, Sudo T, et al. Number of metastatic lymph nodes, but not lymph node ratio, is an independent prognostic factor after resection of pancreatic carcinoma. J Am Coll Surg. 2010;211(2):196–204.
Schwarz RE, Smith DD. Extent of lymph node retrieval and pancreatic cancer survival: information from a large US population database. Ann Surg Oncol. 2006;13(9):1189–200.
Tomlinson JS, Jain S, Bentrem DJ, et al. Accuracy of staging node-negative pancreas cancer: a potential quality measure. Arch Surg. 2007;142(8):767–723.
Jang JY, Kang MJ, Heo JS, et al. A prospective randomized controlled study comparing outcomes of standard resection and extended resection, including dissection of the nerve plexus and various lymph nodes, in patients with pancreatic head cancer. Ann Surg. 2014;259(4):656–64.
Lee W, Jeong CY, Kim YH, et al. Validation of the prognostic performance in various nodal staging systems for gallbladder cancer: results of a multicenter study. Langenbecks Arch Surg. 2019;404(5):581–8.
Valsangkar NP, Bush DM, Michaelson JS, et al. N0/N1, PNL, or LNR? The effect of lymph node number on accurate survival prediction in pancreatic ductal adenocarcinoma. J Gastrointest Surg. 2012;17(2):257–66.
Pawlik TM, Gleisner AL, Cameron JL, et al. Prognostic relevance of lymph node ratio following pancreaticoduodenectomy for pancreatic cancer. Surgery. 2007;141(5):610–8.
Wang J, Hassett JM, Dayton MT, Kulaylat MN. The prognostic superiority of log odds of positive lymph nodes in stage III colon cancer. J Gastrointest Surg. 2008;12(10):1790–6.
Riediger H, Kulemann B, Wittel U, et al. Prognostic role of log odds of lymph nodes after resection of pancreatic head cancer. J Gastrointest Surg. 2016;20(10):1707–15.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
All authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lee, W., Lee, J.B., Hong, S. et al. Predictive Performance of Current Nodal Staging Systems in Various Categories of Pancreatic Cancer. Ann Surg Oncol 29, 390–398 (2022). https://doi.org/10.1245/s10434-021-10641-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-021-10641-7