Abstract
Background
Although the current nodal staging system for gallbladder cancer (GBC) was changed based on the number of positive lymph nodes (PLN), it needs to be evaluated in various situations.
Methods
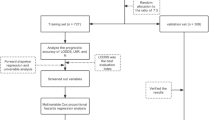
We reviewed the clinical data for 398 patients with resected GBC and compared nodal staging systems based on the number of PLNs, the positive/retrieved LN ratio (LNR), and the log odds of positive LN (LODDS). Prognostic performance was evaluated using the C-index.
Results
Subgroups were formed on the basis of an restricted cubic spline plot as follows: PLN 3 (PLN = 0, 1–2, ≥ 3); PLN 4 (PLN = 0, 1–3, ≥ 4); LNR (LNR = 0, 0–0.269, ≥ 0.27); and LODDS (LODDS < − 0.8, − 0.8–0, ≥ 0). The oncological outcome differed significantly between subgroups in each system. In all patients with GBC, PLN 4 (C-index 0.730) and PLN 3 (C-index 0.734) were the best prognostic discriminators of survival and recurrence, respectively. However, for retrieved LN (RLN) ≥ 6, LODDS was the best discriminator for survival (C-index 0.852).
Conclusion
The nodal staging system based on PLN was the optimal prognostic discriminator in patients with RLN < 6, whereas the LODDS system is adequate for RLN ≥ 6. The following nodal staging system considers applying different systems according to the RLN.


Similar content being viewed by others
References
Chan E, Berlin J (2015) Biliary tract cancers: understudied and poorly understood. J Clin Oncol 33(16):1845–1848. https://doi.org/10.1200/JCO.2014.59.7591
Aloia TA, Jarufe N, Javle M, Maithel SK, Roa JC, Adsay V, Coimbra FJ, Jarnagin WR (2015) Gallbladder cancer: expert consensus statement. HPB (Oxford) 17(8):681–690. https://doi.org/10.1111/hpb.12444
Chen C, Geng Z, Shen H, Song H, Zhao Y, Zhang G, Li W, Ma L, Wang L (2016) Long-term outcomes and prognostic factors in advanced gallbladder cancer: focus on the advanced T stage. PLoS One 11(11):e0166361. https://doi.org/10.1371/journal.pone.0166361
Lee SE, Kim KS, Kim WB, Kim IG, Nah YW, Ryu DH, Park JS, Yoon MH, Cho JY, Hong TH, Hwang DW, Choi DW, Korean Association of H-B, Pancreas S (2014) Practical guidelines for the surgical treatment of gallbladder cancer. J Korean Med Sci 29(10):1333–1340. https://doi.org/10.3346/jkms.2014.29.10.1333
Shindoh J, de Aretxabala X, Aloia TA, Roa JC, Roa I, Zimmitti G, Javle M, Conrad C, Maru DM, Aoki T, Vigano L, Ribero D, Kokudo N, Capussotti L, Vauthey JN (2015) Tumor location is a strong predictor of tumor progression and survival in T2 gallbladder cancer: an international multicenter study. Ann Surg 261(4):733–739. https://doi.org/10.1097/SLA.0000000000000728
Lee W, Jeong CY, Jang JY, Kim YH, Roh YH, Kim KW, Kang SH, Yoon MH, Seo HI, Yun SP, Park JI, Jung BH, Shin DH, Choi YI, Moon HH, Chu CW, Ryu JH, Yang K, Park YM, Hong SC (2017) Do hepatic-sided tumors require more extensive resection than peritoneal-sided tumors in patients with T2 gallbladder cancer? Results of a retrospective multicenter study. Surgery 162:515–524. https://doi.org/10.1016/j.surg.2017.05.004
Chun YS, Pawlik TM, Vauthey JN (2018) 8th edition of the AJCC Cancer staging manual: pancreas and hepatobiliary cancers. Ann Surg Oncol 25(4):845–847. https://doi.org/10.1245/s10434-017-6025-x
Sternby Eilard M, Lundgren L, Cahlin C, Strandell A, Svanberg T, Sandstrom P (2017) Surgical treatment for gallbladder cancer - a systematic literature review. Scand J Gastroenterol 52(5):505–514. https://doi.org/10.1080/00365521.2017.1284895
Amini N, Kim Y, Wilson A, Margonis GA, Ethun CG, Poultsides G, Tran T, Idrees K, Isom CA, Fields RC, Krasnick B, Weber SM, Salem A, Martin RC, Scoggins C, Shen P, Mogal HD, Schmidt C, Beal E, Hatzaras I, Shenoy R, Maithel SK, Pawlik TM (2016) Prognostic implications of lymph node status for patients with gallbladder cancer: a multi-institutional study. Ann Surg Oncol 23(9):3016–3023. https://doi.org/10.1245/s10434-016-5243-y
Birnbaum DJ, Vigano L, Russolillo N, Langella S, Ferrero A, Capussotti L (2015) Lymph node metastases in patients undergoing surgery for a gallbladder cancer. Extension of the lymph node dissection and prognostic value of the lymph node ratio. Ann Surg Oncol 22(3):811–818. https://doi.org/10.1245/s10434-014-4044-4
Kim SH, Chong JU, Lim JH, Choi GH, Kang CM, Choi JS, Lee WJ, Kim KS (2016) Optimal assessment of lymph node status in gallbladder cancer. Eur J Surg Oncol 42(2):205–210. https://doi.org/10.1016/j.ejso.2015.10.013
O’Donnell M, Mente A, Rangarajan S, McQueen MJ, Wang X, Liu L, Yan H, Lee SF, Mony P, Devanath A, Rosengren A, Lopez-Jaramillo P, Diaz R, Avezum A, Lanas F, Yusoff K, Iqbal R, Ilow R, Mohammadifard N, Gulec S, Yusufali AH, Kruger L, Yusuf R, Chifamba J, Kabali C, Dagenais G, Lear SA, Teo K, Yusuf S, Investigators P (2014) Urinary sodium and potassium excretion, mortality, and cardiovascular events. N Engl J Med 371(7):612–623. https://doi.org/10.1056/NEJMoa1311889
Warensjo E, Byberg L, Melhus H, Gedeborg R, Mallmin H, Wolk A, Michaelsson K (2011) Dietary calcium intake and risk of fracture and osteoporosis: prospective longitudinal cohort study. BMJ 342:d1473. https://doi.org/10.1136/bmj.d1473
Lee W, Han HS, Ahn S, Yoon YS, Cho JY, Choi Y (2018) Correlation between resection margin and disease recurrence with a restricted cubic spline model in patients with resected hepatocellular carcinoma. Dig Surg 35(6):520–531. https://doi.org/10.1159/000485805
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213. https://doi.org/10.1097/01.sla.0000133083.54934.ae
Horgan AM, Amir E, Walter T, Knox JJ (2012) Adjuvant therapy in the treatment of biliary tract cancer: a systematic review and meta-analysis. J Clin Oncol 30(16):1934–1940. https://doi.org/10.1200/JCO.2011.40.5381
Chen LJ, Chung KP, Chang YJ, Chang YJ (2015) Ratio and log odds of positive lymph nodes in breast cancer patients with mastectomy. Surg Oncol 24(3):239–247. https://doi.org/10.1016/j.suronc.2015.05.001
Coburn NG, Cleary SP, Tan JC, Law CH (2008) Surgery for gallbladder cancer: a population-based analysis. J Am Coll Surg 207(3):371–382. https://doi.org/10.1016/j.jamcollsurg.2008.02.031
Cai ZQ, Guo P, Si SB, Geng ZM, Chen C, Cong LL (2017) Analysis of prognostic factors for survival after surgery for gallbladder cancer based on a Bayesian network. Sci Rep 7(1):293. https://doi.org/10.1038/s41598-017-00491-3
Cziupka K, Partecke LI, Mirow L, Heidecke CD, Emde C, Hoffmann W, Siewert U, van den Berg N, von Bernstorff W, Stier A (2012) Outcomes and prognostic factors in gallbladder cancer: a single-centre experience. Langenbeck's Arch Surg 397(6):899–907. https://doi.org/10.1007/s00423-012-0950-8
Kokudo N, Makuuchi M, Natori T, Sakamoto Y, Yamamoto J, Seki M, Noie T, Sugawara Y, Imamura H, Asahara S, Ikari T (2003) Strategies for surgical treatment of gallbladder carcinoma based on information available before resection. Arch Surg 138(7):741–750; discussion 750. https://doi.org/10.1001/archsurg.138.7.741
Miyazaki M, Yoshitomi H, Miyakawa S, Uesaka K, Unno M, Endo I, Ota T, Ohtsuka M, Kinoshita H, Shimada K, Shimizu H, Tabata M, Chijiiwa K, Nagino M, Hirano S, Wakai T, Wada K, Isayama H, Okusaka T, Tsuyuguchi T, Fujita N, Furuse J, Yamao K, Murakami K, Yamazaki H, Kijima H, Nakanuma Y, Yoshida M, Takayashiki T, Takada T (2015) Clinical practice guidelines for the management of biliary tract cancers 2015: the 2nd English edition. J Hepatobiliary Pancreat Sci 22(4):249–273. https://doi.org/10.1002/jhbp.233
Benson AB 3rd, D'Angelica MI, Abbott DE, Abrams TA, Alberts SR, Saenz DA, Are C, Brown DB, Chang DT, Covey AM, Hawkins W, Iyer R, Jacob R, Karachristos A, Kelley RK, Kim R, Palta M, Park JO, Sahai V, Schefter T, Schmidt C, Sicklick JK, Singh G, Sohal D, Stein S, Tian GG, Vauthey JN, Venook AP, Zhu AX, Hoffmann KG, Darlow S (2017) NCCN guidelines insights: hepatobiliary cancers, version 1.2017. J Natl Compr Cancer Netw 15(5):563–573
Negi SS, Singh A, Chaudhary A (2011) Lymph nodal involvement as prognostic factor in gallbladder cancer: location, count or ratio? J Gastrointest Surg 15(6):1017–1025. https://doi.org/10.1007/s11605-011-1528-4
Pandey D (2012) Technical description of a regional lymphadenectomy in radical surgery for gallbladder cancer. HPB (Oxford) 14(3):216–219. https://doi.org/10.1111/j.1477-2574.2011.00430.x
Mahul B, Amin SBE, Brookland RK, Jessup JM, Greene FL, Brierley JD, Byrd DR (2017) AJCC cancer staging manual eighth edition.
Lee AJ, Chiang YJ, Lee JE, Conrad C, Chun YS, Aloia TA, Vauthey JN, Tzeng CD (2018) Validation of American joint committee on cancer eighth staging system for gallbladder cancer and its lymphadenectomy guidelines. J Surg Res 230:148–154. https://doi.org/10.1016/j.jss.2018.04.067
Choi BG, Kim CY, Cho SH, Kim HJ, Koh YS, Kim JC, Cho CK, Kim HJ, Hur YH (2013) Impact of lymph node ratio as a valuable prognostic factor in gallbladder carcinoma, focusing on stage IIIB gallbladder carcinoma. J Korean Surg Soc 84(3):168–177. https://doi.org/10.4174/jkss.2013.84.3.168
Ito H, Ito K, D'Angelica M, Gonen M, Klimstra D, Allen P, DeMatteo RP, Fong Y, Blumgart LH, Jarnagin WR (2011) Accurate staging for gallbladder cancer: implications for surgical therapy and pathological assessment. Ann Surg 254(2):320–325. https://doi.org/10.1097/SLA.0b013e31822238d8
Aurello P, Petrucciani N, Nigri GR, La Torre M, Magistri P, Tierno S, D’Angelo F, Ramacciato G (2014) Log odds of positive lymph nodes (LODDS): what are their role in the prognostic assessment of gastric adenocarcinoma? J Gastrointest Surg 18(7):1254–1260. https://doi.org/10.1007/s11605-014-2539-8
Tez M, Altundag K (2017) Log odds of metastatic lymph nodes (LODDS) or negative to positive lymph node ratio? Surgery 162:461. https://doi.org/10.1016/j.surg.2017.01.021
Bagante F, Tran T, Spolverato G, Ruzzenente A, Buttner S, Ethun CG, Groot Koerkamp B, Conci S, Idrees K, Isom CA, Fields RC, Krasnick B, Weber SM, Salem A, Martin RC, Scoggins C, Shen P, Mogal HD, Schmidt C, Beal E, Hatzaras I, Vitiello G, JN IJ, Maithel SK, Poultsides G, Guglielmi A, Pawlik TM (2016) Perihilar cholangiocarcinoma: number of nodes examined and optimal lymph node prognostic scheme. J Am Coll Surg 222(5):750–759 e752. https://doi.org/10.1016/j.jamcollsurg.2016.02.012
Acknowledgments
The authors thank the members of the Busan-Ulsan-Kyeungnam HBP Surgery Study Group of Korea for cooperating in this study and for providing the clinicopathologic information for the patients with gallbladder cancer.
Author information
Authors and Affiliations
Contributions
Study conception and design: Lee, Jeong, YH Kim, Yoon, Hong. Acquisition of data: Lee, KW Kim, Jung, Yang. Analysis and interpretation of data: Lee, Seo, Choi, Ryu, Hong, CS choi, Nah. Drafting of manuscript: Lee, Jeong, JI Park, Chu, Ryu, Shin. Critical revision: Lee, Jeong, Roh, Shin, Hong.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Institutional Research Committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 49 kb)
Rights and permissions
About this article
Cite this article
Lee, W., Jeong, CY., Kim, Y.H. et al. Validation of the prognostic performance in various nodal staging systems for gallbladder cancer: results of a multicenter study. Langenbecks Arch Surg 404, 581–588 (2019). https://doi.org/10.1007/s00423-019-01807-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-019-01807-9