Abstract
Objective
This study was designed to evaluate the prognostic value of the preoperative albumin–globulin score (AGS) in the patients with non-small cell lung cancer (NSCLC) after pulmonary lobectomy.
Methods and Results
The optimal cutoff level was 40.00 and 27.05 g/L for Alb and Glb, respectively. Based on this and the previous study, patients with both an hypoalbuminemia (< 40.00 g/L) and an elevated Glb level (≥ 27.05 g/L) were assigned a score of 2, and patients with one or neither were assigned a score of 1 or 0, respectively. We investigated the correlations between the AGS and the clinicopathological characteristics of patients and found that AGS was significantly associated with TNM stage (P = 0.016). Multivariate Cox analyses indicated that the AGS was an independent prognostic indicator for NSCLC for disease-free survival (DFS) (P = 0.001) and overall survival (OS) (P = 0.004). Kaplan–Meier analysis and log-rank test demonstrated that there were significant differences in DFS (P < 0.001) and OS (P < 0.001) among the three AGS groups. Furthermore, our study showed that DFS and OS are significantly different in three groups of patients with different AGS, in both Squamous carcinoma (P < 0.001 for DFS; P < 0.001 for OS) or adenocarcinoma (P = 0.034 for DFS; P = 0.035 for OS). In addition, we enrolled 53 patients as an independent set of cases for the further validation of AGS. Multivariate analyses verified AGS was an independent prognostic factor for NSCLC patients (P = 0.020 for DFS; P = 0.018 for OS).
Conclusions
Preoperative AGS is an independent prognostic factor for patients with operable NSCLC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Lung cancer is the most common cause of cancer death worldwide, and its 5-year survival rates is less than 15%.1 Non-small-cell lung cancer (NSCLC) accounts for more than 80% of lung cancer diagnoses.2 Among all treatment of NSCLC, including surgery, chemotherapy, radiotherapy, targeted therapy, and immunotherapy, the best choice for patients with early-stage disease is still surgery.3,4,5,6 Plenty of indicators were proved to have prognostic value for NSCLC, especially the American Joint Committee on Cancer (AJCC), the Union for International Cancer Control (UICC) tumor-node- metastasis (TNM) staging system.7,8 But it cannot be obtained preoperatively.
Recently, several host-based and inflammation-based indicators have been reported in the literature for patients with NSCLC, such as CRP/Alb ratio, neutrophil to lymphocyte ratio (NLR), and platelet to lymphocyte ratio (PLR).9,10,11,12,13 Malnutrition and systemic inflammatory response were shown to promote tumor progression by destroying immune function, inducing angiogenesis and altering biological features of tumor cells.14,15 Albumin (Alb) and globulin (Glb) are two major components of total proteins in serum human. Serum Alb is commonly used to evaluate the nutritional status and the severity of cancer patients.16 The low level of Alb also is associated with systemic inflammatory response of the host.17 So Alb has been reported to be an independent prognostic factor for NSCLC. The other important serum protein, globulin, plays an important role in immune and inflammation of the host through regulation of inflammatory cytokines.18 Previous studies have shown that albumin to globulin ratio (AGR) is an independent prognostic indicator for several cancers, such as breast cancer and gastric cancer.19,20,21,22 Similarly, a recent study put forward a novel predictor, albumin–globulin score (AGS), which reflects the cumulative effect of both Alb and Glb on esophageal squamous cell carcinoma (ESCC) patients.23 However, there is no report on the relationship between the AGS and the outcome in patients with operable NSCLC.
Methods
Patients
We retrospectively reviewed clinical data for 512 patients who were diagnosed with NSCLC and treated at the First Affiliated Hospital of Xi’an Jiaotong University between 2008 and 2013. The study was approved by the ethics committees at the First Affiliated Hospital of Xi’an Jiaotong University. All patients provided written, informed consent. The inclusion criteria of this study were: (1) pathologically diagnosed NSCLC, (2) surgery included radical resection, (3) preoperative testing included blood tests for liver function 1 week before surgery, and (4) a diagnosis without other malignancies, residual lung cancer or metastatic bronchogenic carcinoma. Patients who met the following criteria were excluded from the study: (1) died in the perioperative period or from non-cancer-related causes, (2) had incomplete medical records, (3) autoimmune disease and (4) severe liver or kidney malfunction. Moreover, the patients neither received neoadjuvant chemoradiation nor took nutritional supplements preoperatively. Based on the inclusion and exclusion criteria, a total of 312 NSCLC patients were analyzed in this study. To further verify the value of AGS, we supplemented a validation group of 53 patients from April 2013 to May 2014.
Clinical Data Collection and Follow-Up
Patient information and laboratory data before surgery were retrieved from the patient records. All parameters were measured within 1 week before surgery to avoid any impacts of surgery, chemotherapy, or radiotherapy. We selected and evaluated the following clinicopathological factors: age, gender, smoking status, pathological type, tumor differentiation, adjuvant chemoradiation, and TNM stage (American Joint Committee on Cancer (AJCC) 7th edition). Smokers were defined as patients who had more than 100 cigarettes in their lifetime. The extent of weight loss and Eastern Cooperative Oncology Group performance status (ECOG-PS) were measured at the time of diagnosis. All patients enrolled in this study had complete blood counts and serum chemistry analysis, including white blood cell count, neutrophil count, lymphocyte count, and platelet count, measurements of Alb, Glb, as well as the serum tumor markers NSE, CEA, and cyfra21-1.
The optimal cutoff value was identified as 40.00 and 27.05 g/L for Alb and Glb using ROC curve analyses, respectively. Based on these cutoff values and the previous study, we defined AGS as follows: patients with both an hypoalbuminemia (< 40.00 g/L) and an elevated Glb level (≥ 27.05 g/L) were assigned an AGS of 2, whereas those with only one of the two abnormalities were assigned an AGS of 1 and those with normal values for both parameters were assigned an AGS of 0. Weight loss was defined as loss of more than 5% pretreatment weight before operation. Other host-related and inflammation-related prognostic indicators used in this study were defined and calculated as follows: NLR was calculated by dividing the absolute neutrophil count by the absolute lymphocyte count, the PLR was defined as the absolute platelet count divided by the absolute lymphocyte count, and the AGR was defined as the ratio of serum Alb to Glb.
All patients were followed up for 3 years; the last date of follow-up was March 31, 2016 or death from any cause (the last date of follow-up in validated group was September 30, 2017). Patients were followed every 3 months for the first 2 years after radical resection and annually thereafter. The postoperative follow-up assessments included routine blood test, liver function, tumor biomarkers, whole body bone scan, computed tomography, and magnetic resonance imaging. The patient will receive a thorough examination when there is any evidence of recurrence and metastasis, including local relapse and distant metastasis, confirmed by computed tomography or magnetic resonance imaging.
Statistical Analysis
Disease-free survival (DFS) was defined as the duration of time between the date of surgery and the date of first recurrence or last follow-up. Data are presented as the mean ± standard deviation (SD). To classify the patients into two groups, the optimal cutoff values of Alb and Glb were determined using ROC curve analyses. The significance of correlations between the preoperative AGS and clinicopathological characteristics was analyzed using the χ2 test and Kruskal–Wallis test. The health status of all patients was provided by the hospital database or telephone interviews. Survival curve was estimated by Kaplan–Meier analysis, and the log-rank test was used to examine the significance of differences in survival distributions between groups. Univariate and multivariate Cox proportional hazards analyses were used to assess the relative effect of the AGS on DFS and OS. Hazard ratio (HR) and 95% confidence interval (95% CI) values were calculated by the Cox proportional hazards model. All statistical analyses were performed using the SPSS 20.0 statistical software (SPSS, Chicago, IL, USA). Generally, P < 0.05 was considered statistically significant for all analyses.
Results
Patients’ Baseline Characteristics
According to the inclusion and exclusion criteria, a total of 312 patients with histologically confirmed as NSCLC were enrolled in this study. In these patients, 223 (71.5%) of them were males and 89(28.5%) were females. The median age was 59 years, with an age range from 18 to 78 years. All patients were able to tolerate surgery, which included adenosquamous carcinoma and large cell carcinoma. There were 174 (55.8%) smokers and 138 (44.2%) nonsmokers. Twenty-nine (9.3%) patients had a loss of more than 5% pretreatment weight. A total of 215 (68.9%) patients were classified into the ECOG-PS group of 0, whereas 95 (30.4%) of them were in the group of 1. The distribution of pathological stages was as follows: stage I, 133 (42.6%); stage II, 99 (31.7%); and stage III, 80 (25.6%; Table 1).
Correlation Between Preoperative AGS and Clinical Pathological Characteristics
The correlation between AGS and the clinicopathological characteristics is shown in Table 2. It was demonstrated that AGS has significant correlation with gender (P = 0.027), histological subtype (P = 0.003), differentiation (P = 0.014), adjuvant chemoradiation (P = 0.013), TNM stage (P = 0.016), neutrophil count (P = 0.035), platelet count (P = 0.001), NLR (P = 0.010), and PLR (P = 0.001).
Survival Analysis with the AGR
The follow-up period ranged from 2 to 91 (median: 41; mean: 39) months. At the end of the last follow-up, 119 of the total patients had died, and the ratio for loss to follow-up was 8.7% (n = 27). Survival analyses were performed in relation to AGS and patient prognosis. Univariate analyses of DFS revealed that gender (P = 0.003), ECOG-PS (P = 0.045), differentiation (P < 0.001), tumor stage (P < 0.001), node stage (P < 0.001), TNM stage (P < 0.001), neutrophil count (P = 0.002), PLR (P = 0.005), NSE (P < 0.001), Alb (P < 0.001), Glb (P = 0.002), AGR (P < 0.001), and AGS (P < 0.001) were significantly associated with DFS. Subsequent multivariate analyses revealed that AGS was an independent prognostic factor for NSCLC patients (P = 0.001); patients with AGS = 0 had better prognosis than patients with AGS = 1 or AGS = 2 (hazard ration [HR]: 1.523; 95% confidence interval [CI]: 1.178–1.969). In addition, differentiation (HR: 3.379; 95% CI 1.566–5.808; P < 0.001) and TNM stage (HR: 2.642; 95% CI 1.631–4.279; P < 0.001) were significant independent predictors of DFS (Table 3).
For OS, multivariate analysis using the 12 clinicopathological characteristics selected by univariate analyses (excluding Alb and Glb) demonstrated that preoperative AGS was significantly associated with OS (HR: 1.513, 95% CI 1.142–2.004, P = 0.004) along with TNM stage (HR: 2.692; 95% CI 1.655–4.379; P < 0.001) and differentiation (HR: 4.692; 95% CI 2.417–9.109; P < 0.001; Table 4).
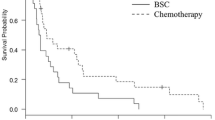
Kaplan–Meier analysis and log-rank test demonstrated that there were significant differences in DFS and OS among three groups of patients with different AGS (P < 0.001 and P < 0.001, respectively). Patients with higher AGS had better prognosis (Fig. 1). Therefore, the preoperative AGS was able to divide the patients into three independent groups. Furthermore, we performed another Kaplan–Meier analysis to evaluate the prognostic value of AGS in NSCLC patients with different histological subtype. We found that DFS and OS are significantly different in three groups of patients with different AGS in both squamous carcinoma (SqCC) (P < 0.001 for DFS; P < 0.001 for OS) and adenocarcinoma (P = 0.034 for DFS; P = 0.035 for OS). However, these differences are more significant in squamous carcinoma patients (Fig. 2). Therefore, the preoperative AGS was able predict the prognosis for patients with NSCLC, especially for squamous carcinoma (SqCC) or adenocarcinoma.
Further Validation in an Independent Set of Cases
The baseline characteristics of the validation group of 53 patients are listed in Table 5. We performed survival analyses to identify the correlation between AGS and patient prognosis. Multivariate analyses verified that AGS was an independent prognostic factor for NSCLC patients (P = 0.020 for DFS; P = 0.018 for OS; Tables 6 and 7).
Kaplan–Meier analysis and log-rank test also validated that there were significant differences in DFS and OS among the three AGS groups (P = 0.003 and P = 0.019, respectively; Fig. 3).
Discussion
It is now widely accepted that systemic inflammation is associated with the poor prognosis in cancer patients. In previous studies, some indicators, such as NLR, PLR, CRP/Alb ratio, and AGR, showed their prognostic value for several tumors.9,10,11,12,13 NLR and PLR are useful prognostic markers for patients with NSCLC. The CRP/Alb ratio is an inflammation-based independent prognostic factor for patients with esophageal squamous cell carcinoma, SCLC, and hepatocellular carcinoma.24,25,26 AGR predicts the outcome of patients with upper tract urothelial carcinoma, esophageal squamous cell carcinoma, or metastatic colorectal cancer.22,23,27 Based on this, a recent study calculated a novel index, AGS, to predict the outcome of patients with esophageal squamous cell carcinoma. They compared the prognostic value of preoperative AGR and AGS in a cohort study of 458 ESCC patients from a statistical point of view and concluded that AGS outperformed AGR as a prognostic factor in ESCC.23 To the best of our knowledge, this is the first study to demonstrate the prognostic significance of preoperative AGS in patients with NSCLC.
Alb, produced by the liver, is a major protein in blood. It is one of the most commonly used markers for assessing patients’ nutritional status.28 In patients with various cancers, low baseline serum Alb predicted shorter survival. When patients are well nourished and their hepatocytes are generating Alb normally, they are more resistant to disease and tumor growth.16,29,30 Thus, Alb levels reflect the ability of the host to fight the tumor to a certain degree. On the other hand, the production of Alb by hepatocytes is suppressed by the activation of proinflammatory cytokines, such as interleukin-1, interleukin-6, and tumor necrosis factor-α. These proinflammatory cytokines can promote tumor development.17,30 Furthermore, albumin acts as a free-radical scavenger, stabilizes cell growth and replication of DNA, and maintains the homeostasis of sex hormones in the body; thereby, it inhibits the development of hormone-related cancer.17,31,32,33 Therefore, albumin can be regarded as a both nutritional and inflammation-related factor.
Glb (total protein-Alb) includes various acute-phase proteins, such as C-reactive protein (CRP), serum amyloid A, complement components, fibrinogen, ceruloplasmin, and immunoglobulins.18,34 A higher level of CRP predicts poor survival in patients with several cancers.35,36 Increased complement 3 and IgA predict poorer prognosis in patients with colorectal cancer.19,20 When these proteins are produced in inflammatory conditions, the level of the globulin increases to reflect systemic inflammation in cancer patients.
Derived from Alb and Glb, AGS could expand the predictive value for prognosis of patients with cancer, comprehensively evaluating both the nutritional condition and systemic inflammation of the host. This was reflected in its prominent value in prognosis of NSCLC patients. By investigating correlations between the AGS and the clinicopathological characteristics of patients, we found that AGS was significantly associated with TNM stage, gender, histological subtype, differentiation, adjuvant chemoradiation, NLR, and PLR. The Kaplan–Meier analysis and log-rank test demonstrated that there were significant differences in DFS and OS among three groups of patients with different AGS. Moreover, our study also showed that AGS remained an independent marker in SqCC or adenocarcinoma. Besides, multivariate Cox analyses indicated that the AGS was an independent prognostic indicator for NSCLC. Furthermore, a validation group for the validation of AGS’s prognostic value proved that there were significant differences in DFS and OS among the three AGS groups.
Conclusions
Preoperative AGS is an independent prognostic factor for patients with operable NSCLC and is able to divide these patients into three independent groups before surgery. Also, higher-risk patients based on the preoperative AGS indicate a poorer prognosis.
This study was limited by the inclusion of a single center, a relatively small number of patients, and its retrospective design. In addition, the biological mechanisms underlying the prognostic roles are yet to be elucidated. Therefore, our results require confirmation by a multicenter, prospective study with a large number of patients and basic research in cell and animal models to provide a better conclusion and integrate with other noninvasive testing of biomarkers into more comprehensive clinical practice.37,38
References
Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F, Jemal A, Yu XQ, He J. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66(2):115.
Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012;62(1):10–29.
Shepherd FA, Rodrigues Pereira J, Ciuleanu T, Tan EH, Hirsh T, Thongprasert S, et al. Erlotinib in previously treated non-small-cell lung cancer. N Engl J Med. 2005;353(2):123–32.
Iragavarapu C, Mustafa M, Akinleye A, Furqan M, Mittal V, Cang S, Liu D. Novel ALK inhibitors in clinical use and development. J Hematol Oncol. 2015;8(1):17.
Wang S, Cang S, Liu D. Third-generation inhibitors targeting EGFR T790M mutation in advanced non-small cell lung cancer. J Hematol Oncol. 2016;9(1):34.
Dholaria B, Hammond W, Shreders A, Lou Y. Emerging therapeutic agents for lung cancer. J Hematol Oncol. 2016;9(1):138.
Bria E, Milella M, Sperduti I, Alessandrini G, Visca P, Corzani F, Giannarelli D, Cerasoli V, Cuppone F, Cecere FL. A novel clinical prognostic score incorporating the number of resected lymph-nodes to predict recurrence and survival in non-small-cell lung cancer. Lung Cancer. 2009;66(3):365–71.
Wang CL, Li Y, Yue DS, Zhang LM, Zhang ZF, Sun BS: Value of the metastatic lymph node ratio for predicting the prognosis of non-small-cell lung cancer patients. World J Surg. 2012;36(2):455-62.
Koh YW, Lee HW: Prognostic impact of C-reactive protein/albumin ratio on the overall survival of patients with advanced nonsmall cell lung cancers receiving palliative chemotherapy. Medicine. 2017;96(19):e6848.
Cedrés S, Torrejon D, Martínez A, Martinez P, Navarro A, Zamora E, Muletmargalef N, Felip E. Neutrophil to lymphocyte ratio (NLR) as an indicator of poor prognosis in stage IV non-small cell lung cancer. Clin Transl Oncol. 2012;14(11):864.
Gu X, Sun S, Gao XS, Xiong W, Qin S, Qi X, Ma M, Li X, Zhou D, Wang W. Prognostic value of platelet to lymphocyte ratio in non-small cell lung cancer: evidence from 3430 patients. Sci Rep. 2016;6:22618.
Zhang H, Xia H, Zhang L, Zhang B, Yue D, Wang C. Clinical significance of preoperative neutrophil–lymphocyte vs platelet–lymphocyte ratio in primary operable patients with non–small cell lung cancer. Am J Surg. 2015;210(3):526–35.
Kim SH, Lee HW, Go SI, Lee SI, Lee GW: Clinical significance of the preoperative platelet count and platelet-to-lymphocyte ratio (PLT-PLR) in patients with surgically resected non-small cell lung cancer. Oncotarget. 2016;7(24):36198.
Mcmillan DC: Systemic inflammation, nutritional status and survival in patients with cancer. Curr Opin Clin Nutr Metab Care. 2009;12(3):223.
Al-Shaiba R, Mcmillan DC, Angerson WJ, Leen E, Mcardle CS, Horgan P. The relationship between hypoalbuminaemia, tumour volume and the systemic inflammatory response in patients with colorectal liver metastases. Br J Cancer. 2004;91(2):205–7.
Barbosa-Silva MC: Subjective and objective nutritional assessment methods: what do they really assess? Curr Opin Clin Nutr Metab Care. 2008;11(3):248–54.
Yildirim M, Yildiz M, Duman E, Goktas S, Kaya V. Prognostic importance of the nutritional status and systemic inflammatory response in non-small cell lung cancer. J Buon. 2013;18(3):728.
Azab B, Kedia S, Shah N, Vonfrolio S, Lu W, Naboush A, Mohammed F, Bloom SW. The value of the pretreatment albumin/globulin ratio in predicting the long-term survival in colorectal cancer. Int J Colorectal Dis. 2013;28(12):1629–36.
Azab BN, Bhatt VR, Vonfrolio S, Bachir R, Rubinshteyn V, Alkaied H, Habeshy A, Patel J, Picon AI, Bloom SW. Value of the pretreatment albumin to globulin ratio in predicting long-term mortality in breast cancer patients. Am J Surg. 2013;206(5):764–70.
Duran AO, Inanc M, Karaca H, Dogan I, Berk V, Bozkurt O, Ozaslan E, Ucar M, Eroglu C, Ozkan M: Albumin-globulin ratio for prediction of long-term mortality in lung adenocarcinoma patients. Asian Pacific J Cancer Prev Apjcp. 2014;15(15):6449–53.
Liu J, Chen S, Geng Q, Liu X, Kong P, Zhan Y, Xu D. Prognostic value of pretreatment albumin-globulin ratio in predicting long-term mortality in gastric cancer patients who underwent D2 resection. Oncotargets Ther. 2017;10:2155.
Bo Z, Wei Y, Zhou LQ, He ZS, Cheng S, He Q, Li J, Liu LB, Cong W, Chen XY. Prognostic significance of preoperative albumin-globulin ratio in patients with upper tract urothelial carcinoma. PLoS One. 2015;10(12):e0144961.
Zhang F, Sun P, Wang Z, Wang D, Wang Y, Zhang D, Wang F, Fu J, Xu R, Li Y. Low preoperative albumin-globulin score predicts favorable survival in esophageal squamous cell carcinoma. Oncotarget. 2016;7(21):30550–60.
Kinoshita A, Onoda H, Imai N, Iwaku A, Oishi M, Tanaka K, Fushiya N, Koike K, Nishino H, Matsushima M. The C-reactive protein/albumin ratio, a novel inflammation-based prognostic score, predicts outcomes in patients with hepatocellular carcinoma. Ann Surg Oncol. 2015;22(3):803–10.
Zhou T, Zhan J, Hong S, Hu Z, Fang W, Qin T, Ma Y, Yang Y, He X, Zhao Y. Ratio of C-reactive protein/albumin is an inflammatory prognostic score for predicting overall survival of patients with small-cell lung cancer. Sci Rep. 2015;5:10481.
Xu XL, Yu HQ, Hu W, Song Q, Mao WM. A novel inflammation-based prognostic score, the c-reactive protein/albumin ratio predicts the prognosis of patients with operable esophageal squamous cell carcinoma. PLoS One. 2015;10(9):e0138657.
Shibutani M, Maeda K, Nagahara H, Ohtani H, Iseki Y, Ikeya T, Sugano K, Hirakawa K. The pretreatment albumin to globulin ratio predicts chemotherapeutic outcomes in patients with unresectable metastatic colorectal cancer. BMC Cancer. 2015;15(1):347.
Mcmillan DC, Watson WS, O’Gorman P, Preston T, Scott HR, Mcardle CS. Albumin concentrations are primarily determined by the body cell mass and the systemic inflammatory response in cancer patients with weight loss. Nutr Cancer. 2001;39(2):210.
Oñate-Ocaña LF, Aiello-Crocifoglio V, Gallardo-Rincón D, Herrera-Goepfert R, Brom-Valladares R, Carrillo JF, Cervera E, Mohar-Betancourt A. Serum albumin as a significant prognostic factor for patients with gastric carcinoma. Ann Surg Oncol. 2007;14(2):381–9.
Chojkier M. Inhibition of albumin synthesis in chronic diseases: molecular mechanisms. J Clin Gastroenterol. 2005;39(2):143–6.
Boonpipattanapong T, Chewatanakornkul S. Preoperative carcinoembryonic antigen and albumin in predicting survival in patients with colon and rectal carcinomas. J Clin Gastroenterol. 2006;40(7):592.
Fearon KC, Falconer JS, Slater C, Mcmillan DC, Ross JA, Preston T. Albumin synthesis rates are not decreased in hypoalbuminemic cachectic cancer patients with an ongoing acute-phase protein response. Ann Surg. 1998;227(2):249–54.
Wang CY, Hsieh MJChiu YC. Higher serum C-reactive protein concentration and hypoalbuminemia are poor prognostic indicators in patients with esophageal cancer undergoing radiotherapy. Radiother Oncol. 2009;92(2):270–5.
Kormelink TG, Powe DG, Kuijpers SA, Abudukelimu A, Fens MHAM, Pieters EHE, Ven KVD, Habashy HO, Ellis IO, Blokhuis BR. Immunoglobulin free light chains are biomarkers of poor prognosis in basal-like breast cancer and are potential targets in tumor-associated inflammation. Oncotarget. 2014;5(10):3159.
Steffens S, Ghazal AA, Steinestel J, Lehmann R, Wegener G, Schnoeller TJ, Cronauer MV, Jentzmik F, Schrader M, Kuczyk MA. High CRP values predict poor survival in patients with penile cancer. BMC Cancer. 2013;13(1):223.
Fenner A. Kidney cancer: Postoperative CRP predicts RCC outcome after nephrectomy. Nat Rev Urol. 2010;7(11):593.
Berz D, Raymond VM, Garst JH, Erlander MG. Noninvasive urine testing of EGFR activating mutation and T790M resistance mutation in non-small cell lung cancer. Exp Hematol Oncol. 2015;5(1):24.
Ma W, Gilligan BM, Yuan J, Li T. Current status and perspectives in translational biomarker research for PD-1/PD-L1 immune checkpoint blockade therapy. J Hematol Oncol. 2016;9(1):47.
Acknowledgment
The present study was supported by the National Natural Science Foundation of China (Approved ID No. 81402506) and the Clinical Research Award of the First Affiliated Hospital of Xi’an Jiaotong University, China (Approved ID No. XJTU1AF-CRF-2017-020).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
All clinical studies were conducted in accordance with the protocol approved by the Ethics Committee of the First Affiliated Hospital of Xi’an Jiaotong University.
Disclosure
The authors declare no conflict of interest.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Li, X., Qin, S., Sun, X. et al. Prognostic Significance of Albumin–Globulin Score in Patients with Operable Non-Small-Cell Lung Cancer. Ann Surg Oncol 25, 3647–3659 (2018). https://doi.org/10.1245/s10434-018-6715-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-018-6715-z