Abstract
Anaplastic lymphoma kinase 1 (ALK-1) is a member of the insulin receptor tyrosine kinase family. ALK-1 was initially found in anaplastic large cell lymphoma (ALCL). ALK mutations have also been implicated in the pathogenesis of non-small cell lung cancer (NSCLC) and other solid tumors. Multiple small molecule inhibitors with activity against ALK and related oncoproteins are under clinical development. Two of them, crizotinib and ceritinib, have been approved by FDA for treatment of locally advanced and metastatic NSCLC. More agents (alectinib, ASP3026, X396) with improved safety, selectivity, and potency are in the pipeline. Dual inhibitors targeting ALK and EGFRm (AP26113), TRK (TSR011), FAK (CEP-37440), or ROS1 (RXDX-101, PF-06463922) are under active clinical development.
Similar content being viewed by others
Introduction
Anaplastic lymphoma kinase 1 (ALK-1) is a member of the insulin receptor tyrosine kinase family (RTK) [1]. Members of this family include α and β type PDGF receptors, EGF receptor, HER2/neu, insulin and IGF-1 receptors which regulate cellular growth and may trigger neoplastic transformation when mutated, translocated, or expressed aberrantly [1-3]. ALK-1 first was found to be associated with the (2; 5)(p23; q35) chromosome translocation in Ki-1 lymphoma or anaplastic large cell lymphoma (ALCL) [4]. The same translocation has also been associated with Hodgkin lymphoma [1]. Multiple mutations involving the ALK gene have since been identified in ALCL. ALK mutations have also been implicated in the pathogenesis of rhabdomyosarcoma [5], inflammatory myofibroblastic pseudo tumor [6], neuroblastoma [7] and non-small cell lung Cancer [8]. In this article, we discussed common ALK mutations and provided a review of ALK-1 Inhibitors that are currently in clinical use or under clinical development.
ALK-1 mutations and oncogenesis
Multiple mutations involving the ALK gene located on 2p23 have been described. The first and prototype of these mutations has been the NPM-ALK mutation caused by translocation (2; 5)(p23; q35) [4,9,10]. This mutation fuses the nucleophosmin (NPM) gene with the ALK gene and was first described in Ki-1 Lymphoma. Ki-1 Lymphoma is a distinct subset of large cell lymphomas that are characterized by CD-30 (Ki-1 antigen) positivity. CD30 is a transmembrane protein which belongs to the nuclear growth factor superfamily and is thought to be involved in ligand binding [4]. NPM encodes for the nucleophosmin protein that is localized to the nucleolus and involved in ribosomal assembly. It is postulated that it provides positive feedback to cell growth [11,12]. The NPM-ALK fusion gene encodes a chimeric receptor tyrosine kinase (RTK) that is de-regulated and constitutionally activated. This leads to activation of phospholipase C-γ (PLC-γ) [8]. Activation of PLC-γ leads to growth factor independent proliferation of lymphocytes. Another mechanism that has been elucidated is the hyperphosphorlyation of p80. Fusion of ALK with NPM leads to hyperphosphorylation of p80 and its constitutional activation. This constitutionally active p80 is localized to the cytoplasm and catalyzes the phosphorylation of SH2 domain-containing transforming protein (SHC), an adaptor protein, and insulin receptor substrate 1 (IRS-1) with downstream effects on RAS and epidermal growth factor receptor (EGFR) pathways [12].
Other mechanisms that have been unearthed mainly occur through the Jun set of proteins [13,14]. Jun (cJun, JunB and JunD) are members of the activated protein 1 (AP-1) transcription factor complex. cJun is regulated by the NPM-ALK tyrosine kinase via pathologic phosphorylation and subsequent activation of cJun N-terminal kinase (JNK), the protein kinase capable of phosphorylating serine residues in the N-terminal of cJun and effecting its subsequent activation [13]. JNK is only physiologically phosphorylated by the mitogen activated protein kinase (MAPK) kinases MKK4 and MKK7. However, in the ALCL cells, JNK is phosphorylated by NPM-ALK which in turn phosphorylates and activates cJun.
Activated cJun causes the transcriptional activation of cell cycle proteins (Cyclin D1, Cyclin D3, Cyclin A and Cyclin E) and the inhibition of tumor suppressors such as p53, p21Cip1 and p16Ink4. This is mediated through the recruitment of cAMP response element binding (CREB) protein (CBP) activator [13]. JunB, another member of the Jun subset of AP–1 complex, is also a positive regulator of cell cycle progression [14]. NPM-ALK also increases JunB expression through the mTOR pathway. mTOR is activated by the phosphoinositol 3- kinase/Akt pathways [14,15].
NPM-ALK has also been shown to act through the signal transducer and activator of transcription (STAT), principally STAT3 and STAT5 [16-19]. STAT3, for example, is constitutionally activated by NPM-ALK phosphorylation and is actively involved in the malignant transformation of NPM-ALK expressing lymphocytes [17]. Activated STAT3 enhances the positive autocrine loop involving IL-6 and the IL-6 receptor (IL6R), which in turn up-regulates the expression of Bcl-xL and survivin, two anti-apoptotic factors [18]. STAT5 activation also is thought to protect cells from apoptosis, likely from activation of anti-apoptotic factors such as A1 (or its human homologue, Bfl-1), Bcl-xL, pim-1 and oncostatin M [16].
Another mechanism for NPM-ALK oncogenesis has been elucidated as occurring through the phosphorylation of p60c-src. p60c-src is a src kinase which plays specific roles in downstream effects of the T-cell receptor and causes hematopoietic growth factor independence specifically of IL-3 and granulocyte-macrophage colony stimulating factor (GM-CSF) [20]. Activated Src kinase can lead to activation of NPM-ALK with downstream effects on PI3K/Akt. The effect of ALK on PLC-γ, Shc, IRS-1 and PI3K has been shown to be mediated through pleiotrophin, the ligand for the ALK receptor [21].
Apart from the NPM-ALK mutation, TPM3-ALK mutation caused by the (1;2)(q25;p23) translocation fused ALK with TPM3 gene located on 1q25 [22-24]. TPM3 encodes a non-muscular tropomyosin protein. Tropomyosins are actin binding proteins that mediate the effect of ionized calcium on actin-myosin interaction in skeletal muscle cells [22]. TPM3 has been shown to be fused with the NTRK1 tropomyosin receptor kinase in ALCL and papillary thyroid cancers [22,25,26]. Another tropomyosin gene, TPM4, has also been found to be fused to the ALK gene in inflammatory myofibroblastic tumors (IMT) and other tumors [24,27-30].
Another ALK mutation from fusion of ALK to the ATIC gene has been described [31,32]. ATIC gene encodes the 5-aminoimidazole-4-carboxamide ribonucleotide formyltransferase/IMP cyclohydrolase (AICARFT/IMPCH) bifunctional enzyme. This enzyme catalyzes the last two steps in the purine synthesis pathway. The fusion gene becomes constitutionally active, leading to pathologic activation of ALK. Additional mutations identified in both solid tumors and hematological malignancies include MSN-ALK, MYH9-ALK, RANBP2–ALK, CARS-ALK, CLTCL-ALK [3,33-44]. Rare mutations have been described in NSCLC, lymphoma, renal cell carcinoma and colon cancer [37,45-58] (Tables 1 and 2).
EML4-ALK fusion gene was initially identified in 2007 in non-small cell lung cancer (NSCLC) [59]. This has facilitated the development of the first ALK inhibitor, crizotinib [60]. This mutation arises from inv(2)(p21p23) which leads to the fusion of echinoderm microtubule-associated protein like-4 (EML4) gene with ALK gene. The fusion protein plays a pivotal role in the malignant transformation of susceptible lung parenchyma [61]. EML4 is a member of the EML protein (EMAP) family and plays an important role in the correct formation of microtubules [62]. The EML4-ALK fusion kinase has an ALK fragment identical to the ALK fragment in NPM-ALK. This intracellular kinase is bound to the amino-terminal coiled-coil domain of EML4 and is thought to be responsible for the transforming activity of the fusion protein [23,63-65].
ALK inhibitors in clinical use
Two small molecule inhibitors, crizotinib and ceritinib, of ALK kinase are in clinical use now, several more are in active clinical development (Table 3).
Crizotinib
Crizotinib (PF-02341066, Xalkori, Pfizer) is an orally active small molecule inhibitor of ALK, c-MET/hepatocyte growth factor receptor (HGFR) kinase and ROS1 receptor tyrosine kinase [66,67]. Since August 2011, crizotinib has been approved for treatment of locally advanced or metastatic NSCLC that are ALK positive [60,68-70].
The maximum dose reached in the phase I dose escalation trials for crizotinib was 250 mg twice daily, which was therefore selected for an expanded cohort of 82 patients with advanced ALK-positive NSCLC [70]. Out of 82 patients, 46 had confirmed partial response (PR) and 1 confirmed complete response (CR) with an impressive overall response (OR) of 57%. The estimated progression free survival (PFS) was 72%. These results were upheld in an updated report in which 87 of 143 patients had an OR of 60.8% (95% CI 52.3-68.9), including 3 CR and 84 PR. Median PFS was 9.7 months (95% CI 7.7-12.8), estimated overall survival at 6 and 12 months was 87.9% (95% CI 81.3-92.3) and 74.8% (66.4-81.5) respectively. Most common drug related adverse events were grade 1 or 2, including visual effects, nausea, vomiting, constipation, diarrhea and peripheral edema. The most common grade 3 and grade 4 adverse events were neutropenia (n = 9), elevated alanine aminotransferase (n = 6), hypophosphatemia (n = 6), and lymphopenia (n = 6) [68]. PROFILE 1005 was a global, multicenter, open label, single arm phase 2 study evaluating safety and efficacy of crizotinib (250 mg oral bid every 3 weeks) in patients with advanced ALK positive NSCLC who progressed after more than one cycle of chemotherapy [69]. Of the 255 patients evaluated for tumor response, ORR was 53% (95% CI: 46–60) and disease control rate at 12 weeks was 85% (95% CI: 80–89). Median PFS was 8.5 months (95% CI: 6.2-9.9) and median duration of response was 43 weeks (96% CI: 36–50). PROFILE 1007, a phase 3 study comparing crizotinib to standard chemotherapy (premetrexed or docetaxel) was updated in 347 patients previously treated with first line platinum based chemotherapy. The median PFS was 7.7 months in crizotinib group (n = 173) compared to 3.0 in chemotherapy group (n = 174), hazard ratio of crizotinib to chemotherapy was 0.49 (95% CI: 0.37-0.67); p < 0.001). The ORR was 65% (95% CI: 58–72) with crizotinib compared to 20% (95% CI: 14–26) with chemotherapy (p < 0.001) [60]. Currently another phase 3 study, PROFILE 1014, is evaluating crizotinib vs. chemotherapy in patients with advanced ALK positive NSCLC patients as a first line therapy [71]. At the last update in ASCO 2014 annual meeting, 343 pts with untreated advanced non-squamous ALK-positive NSCLC were treated with either crizotinib 250 mg PO BID (n = 172) or PPC (pemetrexed 500 mg/m2 + either cisplatin 75 mg/m2 or carboplatin AUC 5–6; all IV q3w for <=6 cycles; n = 171). The primary endpoint was PFS. After disease progression, crossover to crizotinib was allowed for pts on PPC. Superiority of crizotinib over PPC in prolonging PFS (median 10.9 vs. 7.0 mo; HR: 0.454; 95% CI: 0.346–0.596; P < 0.0001) was reported. Crizotinib showed higher ORR than PPC (74% vs. 45%; P < 0.0001) [71].
Unfortunately majority of patients invariably develop resistance to crizotinib during the first year [60,68]. Mechanism of acquired resistance to crizotinib can be classified into three well-recognized categories. These are the development of new ALK domain mutations; amplification of the EML4-ALK gene and activation of alternating pathways that bypass the ALK pathway. Two secondary mutations, L1196M and C1156Y, within the kinase domain of EML4-ALK in tumor cells were reported in a patient during the relapse phase of treatment with an ALK inhibitor. These developed independently in subclones of the tumor cells and conferred marked resistance to two different ALK inhibitors [46]. L1196M gatekeeper mutation results from substitution of leucine by methionine at position 1196 of the ALK kinase domain. This mutation alters the ATP-binding site of ALK and interferes with the binding of inhibitor. C1156Y mutation in the ALK domain involves substitution of a cysteine by tyrosine at position 1156. Several other mutations of ALK kinase domain have been reported so far, G1269A, L1152R, G1202R, 1151Tins and S1206Y [72-76]. The second well established mechanism of crizotinib resistance is the amplification of EML4-ALK fusion gene through two methods, more copies per cell and more cells displaying the rearrangement pattern [72,73]. The third category of acquired resistance to ALK agents represents the activation of alternating signaling pathways bypassing ALK. The EML4-ALK fusion protein is one of the client proteins for heat shock protein 90 (Hsp90), which is a molecular chaperone that regulates the correct folding, stability, and function of numerous client proteins. Ganetepib, which is an Hsp90 inhibitor, has been shown to be effective in patients with secondary ALK mutations and in tumor cells with ALK amplification [77]. Hsp90 inhibition has been shown to cause regression of EML4-ALK driven xenograft of lung adenocarcinomas [78]. EGFR up-regulation has also been observed in ALK positive tumor cell lines resistant to crizotinib [72,74]. These mechanisms can occur independently, or simultaneously, suggesting that the combination of both ALK and EGFR inhibitors may represent an effective therapy for this specific subset of NSCLC patients [72,74]. KIT gene amplification has also been identified as a potential bypass signaling pathway in crizotinib resistant patients. This resistance mechanism likely involves support by the cancer stroma since stem cell factor (SCF), the KIT ligand, is produced specifically in the stroma of resistant cancer cells with KIT amplification [72].
Therefore, there is a unmet need for novel ALK inhibitors that can overcome these resistance mechanisms. The development of a range of new ALK inhibitors is underway both in pre-clinical and clinical studies.
Alectinib (CH-5424802, AF-802, RO05424802)
Alectinib, also known as AF-802, CH-5424802 or RO-5424802, is a highly selective, orally bioavailable ALK inhibitor with ten-fold greater potency than crizotinib in kinase assays (IC50, 1.9nM) [79,80]. A carbonitrile derivative, alectinib has potent efficacy against ALK addicted tumors, such as NSCLC expressing EML4-ALK, ALCL expressing NPM-ALK, and ALK amplified neuroblastoma [79]. The compound has also exhibited substantial inhibitory property against mutant ALK enzymes including ALK L1196M, ALK F1174L, and ALK R1275Q [79].
In July 2014, alectinib was granted approval in Japan for the treatment of patients with recurrent/relapsed ALK+ NSCLC [81]. Similarly, the compound has gained Breakthrough Therapy Designation (BTD) by the U.S. FDA in patients with ALK+ NSCLC who had progressed on crizotinib. In an initial phase I dose-escalation portion of the AF-001JP study, treatment of 24 crizotinib-naïve patients with recurrent/relapsed ALK+ NSCLC with alectinib at doses ranging from 20–300 mg twice daily was found to be safe and well tolerated [81]. No DLTs were observed and 300 mg twice daily was chosen as the recommended phase II dose [81]. In the subsequent expanded phase II part of the trial, the agent exhibited clinical activity achieving an ORR of approximately ninety-four percent including 2 CR and 41 PR in 46 patients evaluable for response [81]. The most serious adverse events noted were neutropenia and elevated creatine phosphokinase levels [81]. Similarly, alectinib has demonstrated promising antitumour activity in patients with ALK-rearranged NSCLC resistant to crizotinib, including those with CNS metastases. The phase I/II study conducted by Gadgeel and colleagues showed that alectinib was associated with acceptable toxicity profile in patients who progressed on or were intolerant to crizotinib [82]. No new safety signal emerged; however grade 3 headaches and neutropenia were identified as DLTs in a cohort of patients who received alectinib 900 mg twice a day [82]. The ORR in 44 out of forty-seven patients evaluable for response was 55%, including 1 CR and 23 PR, and sixteen patients had stable disease after a median follow-up of 126 days [82] . Interestingly, a subset analysis of 21 patients with CNS metastases at baseline enrolled in the study showed a disease control rate of approximately 90%. In contrast to the precedent study [81], this recent trial chose alectinib 600 mg twice a day as the recommended dose for subsequent phase 2 studies [82]. Given these favorable results, ALEX, a phase III randomized trial has been initiated to compare alectinib with crizotinib in treatment-naïve ALK-positive advanced NSCLC patients. The study primary endpoint is PFS and the estimated completion date is December 2017 [NCT02075840]. Alectinib was recently reported to be active in crizotinib-resistant NSCLC patients with leptomeningeal metastasis [83].
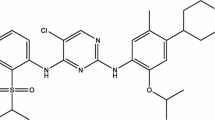
Ceritinib (LDK378)
Ceritinib (LDK378, Celgene) is a potent and selective small molecule tyrosine kinase inhibitor of ALK [84,85]. Ceritinib was shown to be active in NSCLC resistant to crizotinib [86-88]. Preliminary results of a multicenter phase I study of LDK378 were presented at the 48th ASCO annual meeting [89]. Among the 131 patients with advanced malignancies harboring a genetic alteration in ALK, 59 patients were enrolled in the dose escalation phase during which a maximum treatment dose (MTD) of 750 mg was established, and 72 patients in a dose expansion cohort at MTD. In the 123 NSCLC patients, median PFS was 8.6 months (95% CI, 4.3-19.3). In 88 evaluable NSCLC patients who received LDK378 at doses of 400–750 mg daily, the overall response rate (ORR) was 70%. ORR was 73% in a subset of 64 patients who had developed crizotinib resistance. LDK378 was well tolerated. There was no treatment related death and the most common grade 3/4 adverse effects were elevated ALT (12%), diarrhea (7%) and AST elevation (6%). These were updated in a recent publication [90]. Currently two phase II studies are undergoing, the first (NCT01685060) evaluating LDK378 in ALK activated NSCLC patients previously treated with chemotherapy and crizotinib; and the second (NCT01685138) in ALK activated NSCLC patient’s naïve to crizotinib +/–chemotherapy. A Phase III multicenter, randomized study (NCT01828099) is evaluating LDK378 versus standard chemotherapy in previously untreated adult patients with ALK-positive, stage IIIB or IV, NSCLC. Another phase III study is evaluating the antitumor activity of ceritinib versus chemotherapy in patients previously treated with platinum based chemotherapy and crizotinib (NCT01828112). Ceritinib has recently been approved for use in NSCLC patients who have progressed on or are intolerant to crizotinib [91].
Novel ALK inhibitors in clinical development
Multiple new ALK inhibitors are being developed, each with its own unique set of characteristics as detailed below.
AP26113
AP26113 is a potent and selective ALK inhibitor [92]. AP26113 induced tumor regression in BaF3 xenograft model expressing EML4-ALK, and EML4-ALK harboring G1269S and L1196M (gatekeeper) mutations. In preclinical studies, AP26113 was shown to be active against all 9 clinically-identified crizotinib-resistant mutants tested [93]. AP26113 is also a potent, reversible inhibitor of activated and T790M-mutant EGFR, yet it does not inhibit the native enzyme [94]. A phase I/II study was initiated (NCT01449461) to evaluate AP26113 as a dual ALK/mutant EGFR inhibitor. As of 14 Jan 2013, 44 patients were enrolled including 37 with NSCLC [94]. In the dose escalation phase (30-300 mg), two dose limiting toxicities were observed, grade 3 ALT elevations at 240 mg and grade 4 dyspnea at 300 mg. The recommended phase II dose was identified as 180 mg. The most common adverse effects were nausea (45%), fatigue (39%), diarrhea (27%). Among 18 evaluable ALK+ patients, four out of 5 patients with CNS lesions showed improvement on follow up imaging, including one patient resistant to crizotinib and ceritinib. Sixteen patients had EGFR mutation (EGFRm). Of 12 patients with EGFRm, one patient responded at 120 mg (duration 21 weeks, ongoing) and 6 patients had stable disease (2 ongoing, duration 7 and 31 weeks, respectively). In a later update, 114 pts were enrolled: 65 in phase 1 (30–300 mg) and 49 in phase 2 (180 mg) [93]. There were 106 pts with NSCLC. The most common treatment-emergent AEs (20%) were similar to the previous report. Early onset of pulmonary symptoms (dyspnea with hypoxia and/or findings on imaging) were observed in 6/45 (13%) pts at 180 mg QD. These symptoms needed urgent intervention. The respiratory symptoms were not observed at 90 mg QD (n = 8) or in the lead-in dose cohort (n = 19; initiated at 90 mg QD, escalated to 180 mg QD after 1 wk). Therefore, further enrollment with this dose escalation scheme, and an additional cohort of 90 mg QD without escalation were being added. Among 38 evaluable ALK+ NSCLC pts who had prior crizotinib, 24 (63%) reported response, including one CR. Six of 10 pts enrolled with untreated or progressing brain metastases showed response in brain, including 4 with complete resolution; 2 stable disease, 2 progressed; AP26113 has promising anti-tumor activity in pts with crizotinib-resistant ALK+ NSCLC, including pts with brain metastases. A randomized phase 2 trial of AP26113 comparing 90 mg QD vs. 90 mg QD escalating to 180 mg QD in crizotinib-resistant ALK+ NSCLC was planned.
ASP3026
ASP3026 is an oral, selective, potent, ATP competitive small molecule inhibitor of ALK with an IC50 of 3.5nM for ALK [95,96]. A phase I dose escalation trial was initiated to evaluate the safety and clinical activity of ASP3026 in patients with advanced malignancies (excluding leukemia) (NCT01284192). Thirty patients were enrolled in the dose escalation (25–800 mg) part of the study. The most common AEs were constipation, vomiting, nausea and abdominal pain. Grade 3 rash and ALT/AST elevation were dose-limiting. The MTD was established as 525 mg QD with a promising safety and pharmacokinetic (PK) profile in patients with advanced malignancies [95]. Patients (pts) with advanced solid tumors were treated with ASP3026 under fasting conditions without interruption in 3 + 3 dose escalation, “fast follower” phase I trial [97]. The cohorts received ASP3026 from 25 to 800 mg once daily (QD). At the last report for 2014 ASCO annual meeting, 33 patients were enrolled in the dose escalation phase, including 3 ALK+ pts, The phase Ib expansion cohort enrolled another 13 ALK+ pts [total pts N = 46; median (range) age = 61 (19–77) years]. Nausea /vomiting, rash and ALT/AST elevation were dose limiting toxicities. The MTD was 525 mg daily which became the recommended phase 2 dose (RP2D). The most common AEs were fatigue, and GI toxicities. Of 15 pts with ALK+ NSCLC who failed prior crizotinib, 7 (44%) had a PR and 8 had stable disease. The “fast follower” design allowed enrollment of ALK+ pts who achieved PR before the MTD of 525 mg QD was identified. Clinical activity was seen in the phase I trial in ALK+ NSCLC pts who failed crizotinib (NCT01401504).
ALK inhibitors in early phase development
X-376 and X-396 are novel, potent and specific ALK inhibitors with an aminopyridazine-based structure shared by crizotinib. X-396 had a 10 fold higher potency as compared to crizotinib across various cancer cell lines [98]. In addition, X-396 seems to be active against ALK mutants resistant to crizotinib. It has also been shown to penetrate blood–brain barrier.
TSR-011 is a dual ALK/TRK inhibitor developed by Tesaro, Inc., Waltham, MA, USA. It is currently recruiting in a phase I/IIa trial (NCT02048488) [99]; Preliminary results showed a dose range of 30–480 mg, with the DLTs to be dysaesthesia and QTc prolongation. PK modeling has identified 60 mg to have minimal peak exposure with sustained trough concentrations above IC50 required for ALK inhibition. Three of 5 patients with ALK+ NSCLC have achieved PR.
CEP-37440 is a dual ALK/FAK inhibitor currently under investigation in a phase I trial (NCT01922752). Focal adhesion kinase (FAK) is a ubiquitously expressed non-receptor tyrosine kinase implicated in cell adhesion and cell membrane-extracellular matrix interactions. It is thought to be involved in the carcinogenesis of colon cancer and other tumors of epithelial origin [100,101].
NMS-E628 (RXDX-101) is an orally available ALK/ROS-1 Inhibitor. It has been shown to induce complete regression of NSCLC and ALK+ leukemia cells in vitro and in vivo [102]. Currently a phase I/IIa trial studying RXDX-101 (NCT02097810) in locally advanced and metastatic solid tumors is in the recruitment phase.
PF-06463922 is a novel dual inhibitor of ALK/ROS1 with unusual activity against ROS1 kinase. PF-06463922 has IC50 values ranging from 0.1 nM to 1 nM toward ROS kinase inhibition. It was shown to be active across a panel of cell lines harboring ROS1 fusion variants including CD74-ROS1, SLC34A2-ROS1 and Fig-ROS1. This agent was developed to increase CNS availability and widen the spectrum of activity from crizotinib [103]. It has also been shown to overcome the crizotinib resistant CD74-ROS1G2032R mutant. In addition, cyclin D1 was found to be suppressed by this inhibitor in vitro [104]. A phase I/IIa trial (NCT01970865) is currently in the recruitment phase.
Conclusion and future directions
More and more novel agents for targeted therapy of lung cancers are rapidly migrating from bench to bedside [19,89,105-110]. Over the past decade, multiple small molecule inhibitors with activity against ALK and related oncoproteins have been developed [3]. Two of them, crizotinib and ceritinib, have gone on to get FDA approval for clinical use in locally advanced and metastatic NSCLC. More agents with improved safety, selectivity, potency and efficacy profiles are in the pipeline. Dual inhibitors targeting ALK as well as EGFRm, TRK, FAK, or ROS1 are under active clinical development. These agents may have the potential to concur the emerging mutants which become resistant to crizotinib and other agents in refractory and relapsed NSCLC and other solid tumors.
References
Orscheschek K, Merz H, Hell J, Binder T, Bartels H, Feller AC. Large-cell anaplastic lymphoma-specific translocation (t[2;5] [p23;q35]) in Hodgkin’s disease: indication of a common pathogenesis? Lancet. 1995;345(8942):87–90.
Ullrich A, Schlessinger J. Signal transduction by receptors with tyrosine kinase activity. Cell. 1990;61(2):203–12.
Roskoski Jr R. Anaplastic lymphoma kinase (ALK): structure, oncogenic activation, and pharmacological inhibition. Pharmacol Res. 2013;68(1):68–94.
Bullrich F, Morris SW, Hummel M, Pileri S, Stein H, Croce CM. Nucleophosmin (NPM) gene rearrangements in Ki-1-positive lymphomas. Cancer Res. 1994;54(11):2873–7.
Pillay K, Govender D, Chetty R. ALK protein expression in rhabdomyosarcomas. Histopathology. 2002;41(5):461–7.
Cessna MH, Zhou H, Sanger WG, Perkins SL, Tripp S, Pickering D, et al. Expression of ALK1 and p80 in inflammatory myofibroblastic tumor and its mesenchymal mimics: a study of 135 cases. Mod Pathol. 2002;15(9):931–8.
Chen Y, Takita J, Choi YL, Kato M, Ohira M, Sanada M, et al. Oncogenic mutations of ALK kinase in neuroblastoma. Nature. 2008;455(7215):971–4.
Shinmura K, Kageyama S, Tao H, Bunai T, Suzuki M, Kamo T, et al. EML4-ALK fusion transcripts, but no NPM-, TPM3-, CLTC-, ATIC-, or TFG-ALK fusion transcripts, in non-small cell lung carcinomas. Lung Cancer. 2008;61(2):163–9.
Morris SW, Kirstein MN, Valentine MB, Dittmer K, Shapiro DN, Look AT, et al. Fusion of a kinase gene, ALK, to a nucleolar protein gene, NPM, in non-Hodgkin’s lymphoma. Science. 1995;267(5196):316–7.
Onciu M, Behm FG, Downing JR, Shurtleff SA, Raimondi SC, Ma Z, et al. ALK-positive plasmablastic B-cell lymphoma with expression of the NPM-ALK fusion transcript: report of 2 cases. Blood. 2003;102(7):2642–4.
Bai RY, Dieter P, Peschel C, Morris SW, Duyster J. Nucleophosmin-anaplastic lymphoma kinase of large-cell anaplastic lymphoma is a constitutively active tyrosine kinase that utilizes phospholipase C-gamma to mediate its mitogenicity. Mol Cell Biol. 1998;18(12):6951–61.
Fujimoto J, Shiota M, Iwahara T, Seki N, Satoh H, Mori S, et al. Characterization of the transforming activity of p80, a hyperphosphorylated protein in a Ki-1 lymphoma cell line with chromosomal translocation t(2;5). Proc Natl Acad Sci U S A. 1996;93(9):4181–6.
Leventaki V, Drakos E, Medeiros LJ, Lim MS, Elenitoba-Johnson KS, Claret FX, et al. NPM-ALK oncogenic kinase promotes cell-cycle progression through activation of JNK/cJun signaling in anaplastic large-cell lymphoma. Blood. 2007;110(5):1621–30.
Staber PB, Vesely P, Haq N, Ott RG, Funato K, Bambach I, et al. The oncoprotein NPM-ALK of anaplastic large-cell lymphoma induces JUNB transcription via ERK1/2 and JunB translation via mTOR signaling. Blood. 2007;110(9):3374–83.
Bai RY, Ouyang T, Miething C, Morris SW, Peschel C, Duyster J. Nucleophosmin-anaplastic lymphoma kinase associated with anaplastic large-cell lymphoma activates the phosphatidylinositol 3-kinase/Akt antiapoptotic signaling pathway. Blood. 2000;96(13):4319–27.
Nieborowska-Skorska M, Slupianek A, Xue L, Zhang Q, Raghunath PN, Hoser G, et al. Role of signal transducer and activator of transcription 5 in nucleophosmin/ anaplastic lymphoma kinase-mediated malignant transformation of lymphoid cells. Cancer Res. 2001;61(17):6517–23.
Chiarle R, Simmons WJ, Cai H, Dhall G, Zamo A, Raz R, et al. Stat3 is required for ALK-mediated lymphomagenesis and provides a possible therapeutic target. Nat Med. 2005;11(6):623–9.
Zamo A, Chiarle R, Piva R, Howes J, Fan Y, Chilosi M, et al. Anaplastic lymphoma kinase (ALK) activates Stat3 and protects hematopoietic cells from cell death. Oncogene. 2002;21(7):1038–47.
Furqan M, Mukhi N, Lee B, Liu D. Dysregulation of JAK-STAT pathway in hematological malignancies and JAK inhibitors for clinical application. Biomarker Res. 2013;1(1):5.
Cussac D, Greenland C, Roche S, Bai RY, Duyster J, Morris SW, et al. Nucleophosmin-anaplastic lymphoma kinase of anaplastic large-cell lymphoma recruits, activates, and uses pp60c-src to mediate its mitogenicity. Blood. 2004;103(4):1464–71.
Stoica GE, Kuo A, Aigner A, Sunitha I, Souttou B, Malerczyk C, et al. Identification of anaplastic lymphoma kinase as a receptor for the growth factor pleiotrophin. J Biol Chem. 2001;276(20):16772–9.
Lamant L, Dastugue N, Pulford K, Delsol G, Mariame B. A new fusion gene TPM3-ALK in anaplastic large cell lymphoma created by a (1;2)(q25;p23) translocation. Blood. 1999;93(9):3088–95.
Sugawara E, Togashi Y, Kuroda N, Sakata S, Hatano S, Asaka R, et al. Identification of anaplastic lymphoma kinase fusions in renal cancer: large-scale immunohistochemical screening by the intercalated antibody-enhanced polymer method. Cancer. 2012;118(18):4427–36.
Lawrence B, Perez-Atayde A, Hibbard MK, Rubin BP, Dal Cin P, Pinkus JL, et al. TPM3-ALK and TPM4-ALK oncogenes in inflammatory myofibroblastic tumors. Am J Pathol. 2000;157(2):377–84.
Butti MG, Bongarzone I, Ferraresi G, Mondellini P, Borrello MG, Pierotti MA. A sequence analysis of the genomic regions involved in the rearrangements between TPM3 and NTRK1 genes producing TRK oncogenes in papillary thyroid carcinomas. Genomics. 1995;28(1):15–24.
Coulier F, Martin-Zanca D, Ernst M, Barbacid M. Mechanism of activation of the human trk oncogene. Mol Cell Biol. 1989;9(1):15–23.
Du XL, Hu H, Lin DC, Xia SH, Shen XM, Zhang Y, et al. Proteomic profiling of proteins dysregulted in Chinese esophageal squamous cell carcinoma. J Mol Med. 2007;85(8):863–75.
Jazii FR, Najafi Z, Malekzadeh R, Conrads TP, Ziaee AA, Abnet C, et al. Identification of squamous cell carcinoma associated proteins by proteomics and loss of beta tropomyosin expression in esophageal cancer. World J Gastroenterol. 2006;12(44):7104–12.
Mathew P, Morris SW, Kane JR, Shurtleff SA, Pasquini M, Jenkins NA, et al. Localization of the murine homolog of the anaplastic lymphoma kinase (AlK) gene on mouse chromosome 17. Cytogenet Cell Genet. 1995;70(1–2):143–4.
Meech SJ, McGavran L, Odom LF, Liang X, Meltesen L, Gump J, et al. Unusual childhood extramedullary hematologic malignancy with natural killer cell properties that contains tropomyosin 4–anaplastic lymphoma kinase gene fusion. Blood. 2001;98(4):1209–16.
Colleoni GW, Bridge JA, Garicochea B, Liu J, Filippa DA, Ladanyi M. ATIC-ALK: A novel variant ALK gene fusion in anaplastic large cell lymphoma resulting from the recurrent cryptic chromosomal inversion, inv (2)(p23q35). Am J Pathol. 2000;156(3):781–9.
Debiec-Rychter M, Marynen P, Hagemeijer A, Pauwels P. ALK-ATIC fusion in urinary bladder inflammatory myofibroblastic tumor. Genes, Chromosomes Cancer. 2003;38(2):187–90.
Chiarle R, Voena C, Ambrogio C, Piva R, Inghirami G. The anaplastic lymphoma kinase in the pathogenesis of cancer. Nat Rev Cancer. 2008;8(1):11–23.
Cools J, Wlodarska I, Somers R, Mentens N, Pedeutour F, Maes B, et al. Identification of novel fusion partners of ALK, the anaplastic lymphoma kinase, in anaplastic large-cell lymphoma and inflammatory myofibroblastic tumor. Genes, Chromosomes Cancer. 2002;34(4):354–62.
Debelenko LV, Arthur DC, Pack SD, Helman LJ, Schrump DS, Tsokos M. Identification of CARS-ALK fusion in primary and metastatic lesions of an inflammatory myofibroblastic tumor. Lab Invest. 2003;83(9):1255–65.
Huret J, Senon S. ALK (anaplastic lymphoma kinase). Atlas Genet Cytogenet Oncol Haematol. 2003;7(4):217–20.
Lamant L, Gascoyne RD, Duplantier MM, Armstrong F, Raghab A, Chhanabhai M, et al. Non-muscle myosin heavy chain (MYH9): a new partner fused to ALK in anaplastic large cell lymphoma. Genes, Chromosomes Cancer. 2003;37(4):427–32.
Ma Z, Hill DA, Collins MH, Morris SW, Sumegi J, Zhou M, et al. Fusion of ALK to the Ran-binding protein 2 (RANBP2) gene in inflammatory myofibroblastic tumor. Genes, Chromosomes Cancer. 2003;37(1):98–105.
Tort F, Campo E, Pohlman B, Hsi E. Heterogeneity of genomic breakpoints in MSN-ALK translocations in anaplastic large cell lymphoma. Hum Pathol. 2004;35(8):1038–41.
Bridge JA, Kanamori M, Ma Z, Pickering D, Hill DA, Lydiatt W, et al. Fusion of the ALK gene to the clathrin heavy chain gene, CLTC, in inflammatory myofibroblastic tumor. Am J Pathol. 2001;159(2):411–5.
De Paepe P, Baens M, Van Krieken H, Verhasselt B, Stul M, Simons A, et al. ALK activation by the CLTC-ALK fusion is a recurrent event in large B-cell lymphoma. Blood. 2003;102(7):2638–41.
Griffin CA, Hawkins AL, Dvorak C, Henkle C, Ellingham T, Perlman EJ. Recurrent involvement of 2p23 in inflammatory myofibroblastic tumors. Cancer Res. 1999;59(12):2776–80.
Patel AS, Murphy KM, Hawkins AL, Cohen JS, Long PP, Perlman EJ, et al. RANBP2 and CLTC are involved in ALK rearrangements in inflammatory myofibroblastic tumors. Cancer Genet Cytogenet. 2007;176(2):107–14.
Tort F, Pinyol M, Pulford K, Roncador G, Hernandez L, Nayach I, et al. Molecular characterization of a new ALK translocation involving moesin (MSN-ALK) in anaplastic large cell lymphoma. Lab Invest. 2001;81(3):419–26.
Bedwell C, Rowe D, Moulton D, Jones G, Bown N, Bacon CM. Cytogenetically complex SEC31A-ALK fusions are recurrent in ALK-positive large B-cell lymphomas. Haematologica. 2011;96(2):343–6.
Choi YL, Soda M, Yamashita Y, Ueno T, Takashima J, Nakajima T, et al. EML4-ALK mutations in lung cancer that confer resistance to ALK inhibitors. N Engl J Med. 2010;363(18):1734–9.
Debelenko LV, Raimondi SC, Daw N, Shivakumar BR, Huang D, Nelson M, et al. Renal cell carcinoma with novel VCL-ALK fusion: new representative of ALK-associated tumor spectrum. Mod Pathol. 2011;24(3):430–42.
Hernandez L, Bea S, Bellosillo B, Pinyol M, Falini B, Carbone A, et al. Diversity of genomic breakpoints in TFG-ALK translocations in anaplastic large cell lymphomas: identification of a new TFG-ALK (XL) chimeric gene with transforming activity. Am J Pathol. 2002;160(4):1487–94.
Hernández L, Pinyol M, Hernández S, Beà S, Pulford K, Rosenwald A, et al. TRK-fused gene (TFG) is a New partner of ALK in anaplastic large cell lymphoma producing Two structurally DifferentTFG-ALK translocations. Blood. 1999;94(9):3265–8.
Jung Y, Kim P, Jung Y, Keum J, Kim SN, Choi YS, et al. Discovery of ALK-PTPN3 gene fusion from human non-small cell lung carcinoma cell line using next generation RNA sequencing. Genes, Chromosomes Cancer. 2012;51(6):590–7.
Lipson D, Capelletti M, Yelensky R, Otto G, Parker A, Jarosz M, et al. Identification of new ALK and RET gene fusions from colorectal and lung cancer biopsies. Nat Med. 2012;18(3):382–4.
Panagopoulos I, Nilsson T, Domanski HA, Isaksson M, Lindblom P, Mertens F, et al. Fusion of the SEC31L1 and ALK genes in an inflammatory myofibroblastic tumor. Int J Cancer. 2006;118(5):1181–6.
Takeuchi K, Choi YL, Togashi Y, Soda M, Hatano S, Inamura K, et al. KIF5B-ALK, a novel fusion oncokinase identified by an immunohistochemistry-based diagnostic system for ALK-positive lung cancer. Clin Cancer Res. 2009;15(9):3143–9.
Takeuchi K, Soda M, Togashi Y, Ota Y, Sekiguchi Y, Hatano S, et al. Identification of a novel fusion, SQSTM1-ALK, in ALK-positive large B-cell lymphoma. Haematologica. 2011;96(3):464–7.
Togashi Y, Soda M, Sakata S, Sugawara E, Hatano S, Asaka R, et al. KLC1-ALK: a novel fusion in lung cancer identified using a formalin-fixed paraffin-embedded tissue only. PLoS One. 2012;7(2):e31323.
Van Roosbroeck K, Cools J, Dierickx D, Thomas J, Vandenberghe P, Stul M, et al. ALK-positive large B-cell lymphomas with cryptic SEC31A-ALK and NPM1-ALK fusions. Haematologica. 2010;95(3):509–13.
Wong DW, Leung EL, Wong SK, Tin VP, Sihoe AD, Cheng LC, et al. A novel KIF5B-ALK variant in nonsmall cell lung cancer. Cancer. 2011;117(12):2709–18.
Touriol C, Greenland C, Lamant L, Pulford K, Bernard F, Rousset T, et al. Further demonstration of the diversity of chromosomal changes involving 2p23 in ALK-positive lymphoma: 2 cases expressing ALK kinase fused to CLTCL (clathrin chain polypeptide-like). Blood. 2000;95(10):3204–7.
Soda M, Choi YL, Enomoto M, Takada S, Yamashita Y, Ishikawa S, et al. Identification of the transforming EML4-ALK fusion gene in non-small-cell lung cancer. Nature. 2007;448(7153):561–6.
Shaw AT, Kim DW, Nakagawa K, Seto T, Crino L, Ahn MJ, et al. Crizotinib versus chemotherapy in advanced ALK-positive lung cancer. N Engl J Med. 2013;368(25):2385–94.
Mano H. Non-solid oncogenes in solid tumors: EML4-ALK fusion genes in lung cancer. Cancer Sci. 2008;99(12):2349–55.
Inamura K, Takeuchi K, Togashi Y, Nomura K, Ninomiya H, Okui M, et al. EML4-ALK fusion is linked to histological characteristics in a subset of lung cancers. J Thorac Oncol. 2008;3(1):13–7.
Sasaki T, Rodig SJ, Chirieac LR, Janne PA. The biology and treatment of EML4-ALK non-small cell lung cancer. Eur J Cancer. 2010;46(10):1773–80.
Lin E, Li L, Guan Y, Soriano R, Rivers CS, Mohan S, et al. Exon array profiling detects EML4-ALK fusion in breast, colorectal, and non-small cell lung cancers. Mol Cancer Res. 2009;7(9):1466–76.
Rikova K, Guo A, Zeng Q, Possemato A, Yu J, Haack H, et al. Global survey of phosphotyrosine signaling identifies oncogenic kinases in lung cancer. Cell. 2007;131(6):1190–203.
Cui JJ, Tran-Dube M, Shen H, Nambu M, Kung PP, Pairish M, et al. Structure based drug design of crizotinib (PF-02341066), a potent and selective dual inhibitor of mesenchymal-epithelial transition factor (c-MET) kinase and anaplastic lymphoma kinase (ALK). J Med Chem. 2011;54(18):6342–63.
Bergethon K, Shaw AT, Ou SH, Katayama R, Lovly CM, McDonald NT, et al. ROS1 rearrangements define a unique molecular class of lung cancers. J Clin Oncol. 2012;30(8):863–70.
Camidge DR, Bang YJ, Kwak EL, Iafrate AJ, Varella-Garcia M, Fox SB, et al. Activity and safety of crizotinib in patients with ALK-positive non-small-cell lung cancer: updated results from a phase 1 study. Lancet Oncol. 2012;13(10):1011–9.
Kim D-W, Ahn M-J, Shi Y, De Pas TM, Yang P-C, Riely GJ, et al. Results of a global phase II study with crizotinib in advanced ALK-positive non-small cell lung cancer (NSCLC). ASCO Meet Abstr. 2012;30(15):7533.
Kwak EL, Bang YJ, Camidge DR, Shaw AT, Solomon B, Maki RG, et al. Anaplastic lymphoma kinase inhibition in non-small-cell lung cancer. N Engl J Med. 2010;363(18):1693–703.
Mok T, Kim D-W, Wu Y-L, Solomon BJ, Nakagawa K, Mekhail T, et al. First-line crizotinib versus pemetrexed-cisplatin or pemetrexed-carboplatin in patients (pts) with advanced ALK-positive non-squamous non-small cell lung cancer (NSCLC): results of a phase III study (PROFILE 1014). ASCO Meet Abstr. 2014;32(15):8002.
Katayama R, Shaw AT, Khan TM, Mino-Kenudson M, Solomon BJ, Halmos B, et al. Mechanisms of acquired crizotinib resistance in ALK-rearranged lung Cancers. Sci Transl Med. 2012;4(120):120ra117.
Doebele RC, Pilling AB, Aisner DL, Kutateladze TG, Le AT, Weickhardt AJ, et al. Mechanisms of resistance to crizotinib in patients with ALK gene rearranged non-small cell lung cancer. Clin Cancer Res. 2012;18(5):1472–82.
Sasaki T, Koivunen J, Ogino A, Yanagita M, Nikiforow S, Zheng W, et al. A novel ALK secondary mutation and EGFR signaling cause resistance to ALK kinase inhibitors. Cancer Res. 2011;71(18):6051–60.
Huang D, Kim DW, Kotsakis A, Deng S, Lira P, Ho SN, et al. Multiplexed deep sequencing analysis of ALK kinase domain identifies resistance mutations in relapsed patients following crizotinib treatment. Genomics. 2013;102(3):157–62.
Kim S, Kim TM, Kim DW, Go H, Keam B, Lee SH, et al. Heterogeneity of genetic changes associated with acquired crizotinib resistance in ALK-rearranged lung cancer. J Thorac Oncol. 2013;8(4):415–22.
Sang J, Acquaviva J, Friedland JC, Smith DL, Sequeira M, Zhang C, et al. Targeted inhibition of the molecular chaperone Hsp90 overcomes ALK inhibitor resistance in non-small cell lung cancer. Cancer Discov. 2013;3(4):430–43.
Chen Z, Sasaki T, Tan X, Carretero J, Shimamura T, Li D, et al. Inhibition of ALK, PI3K/MEK, and HSP90 in murine lung adenocarcinoma induced by EML4-ALK fusion oncogene. Cancer Res. 2010;70(23):9827–36.
Sakamoto H, Tsukaguchi T, Hiroshima S, Kodama T, Kobayashi T, Fukami TA, et al. CH5424802, a selective ALK inhibitor capable of blocking the resistant gatekeeper mutant. Cancer Cell. 2011;19(5):679–90.
Kinoshita K, Asoh K, Furuichi N, Ito T, Kawada H, Hara S, et al. Design and synthesis of a highly selective, orally active and potent anaplastic lymphoma kinase inhibitor (CH5424802). Bioorg Med Chem. 2012;20(3):1271–80.
Seto T, Kiura K, Nishio M, Nakagawa K, Maemondo M, Inoue A, et al. CH5424802 (RO5424802) for patients with ALK-rearranged advanced non-small-cell lung cancer (AF-001JP study): a single-arm, open-label, phase 1–2 study. Lancet Oncol. 2013;14(7):590–8.
Gadgeel SM, Gandhi L, Riely GJ, Chiappori AA, West HL, Azada MC, et al. Safety and activity of alectinib against systemic disease and brain metastases in patients with crizotinib-resistant ALK-rearranged non-small-cell lung cancer (AF-002JG): results from the dose-finding portion of a phase 1/2 study. Lancet Oncol. 2014;15(10):1119–28.
Gainor JF, Sherman CA, Willoughby K, Logan J, Kennedy E, Brastianos PK, et al. Alectinib salvages CNS metastases in ALK-positive lung cancer patients previously treated with crizotinib and ceritinib. J Thorac Oncol. 2015;10(2):232–6.
Marsilje TH, Pei W, Chen B, Lu W, Uno T, Jin Y, et al. Synthesis, structure-activity relationships, and in vivo efficacy of the novel potent and selective anaplastic lymphoma kinase (ALK) inhibitor 5-chloro-N2-(2-isopropoxy-5-methyl-4-(piperidin-4-yl)phenyl)-N4-(2-(isopropylsulf onyl)phenyl)pyrimidine-2,4-diamine (LDK378) currently in phase 1 and phase 2 clinical trials. J Med Chem. 2013;56(14):5675–90.
Galkin AV, Melnick JS, Kim S, Hood TL, Li N, Li L, et al. Identification of NVP-TAE684, a potent, selective, and efficacious inhibitor of NPM-ALK. Proc Natl Acad Sci U S A. 2007;104(1):270–5.
Friboulet L, Li N, Katayama R, Lee CC, Gainor JF, Crystal AS, et al. The ALK inhibitor ceritinib overcomes crizotinib resistance in non-small cell lung cancer. Cancer discovery. 2014;4(6):662–73.
Rolfo C, Passiglia F, Russo A, Pauwels P. Looking for a new panacea in ALK-rearranged NSCLC: may be Ceritinib? Expert Opin Ther Targets. 2014;18(9):983–5.
Vansteenkiste JF. Ceritinib for treatment of ALK-rearranged advanced non-small-cell lung cancer. Future Oncol. 2014;10(12):1925–39.
Shaw AT, Mehra R, Kim D-W, Felip E, Chow LQM, Camidge DR, et al. Clinical activity of the ALK inhibitor LDK378 in advanced, ALK-positive NSCLC. ASCO Meet Abstr. 2013;31(15):8010.
Shaw AT, Kim DW, Mehra R, Tan DS, Felip E, Chow LQ, et al. Ceritinib in ALK-rearranged non-small-cell lung cancer. N Engl J Med. 2014;370(13):1189–97.
Dhillon S, Clark M. Ceritinib: first global approval. Drugs. 2014;74(11):1285–91.
Zhang S, Wang F, Keats J, Ning Y, Wardwell SD, Moran L, et al. Abstract LB-298: AP26113, a potent ALK inhibitor, overcomes mutations in EML4-ALK that confer resistance to PF-02341066 (PF1066). Cancer Res. 2011;70(8):LB-298.
Gettinger SN, Bazhenova L, Salgia R, Langer CJ, Gold KA, Rosell R, et al. Updated efficacy and safety of the ALK inhibitor AP26113 in patients (pts) with advanced malignancies, including ALK+ non-small cell lung cancer (NSCLC). ASCO Meet Abstr. 2014;32(15):8047.
Camidge DR, Bazhenova L, Salgia R, Weiss GJ, Langer CJ, Shaw AT, et al. First-in-human dose-finding study of the ALK/EGFR inhibitor AP26113 in patients with advanced malignancies: Updated results. ASCO Meet Abstr. 2013;31(15):8031.
Patnaik A, LoRusso P, Ball HA, Bahceci E, Yuen G, Papadopoulos KP, et al. Pharmacokinetics and safety of an oral ALK inhibitor, ASP3026, observed in a phase I dose escalation trial. ASCO Meet Abstr. 2013;31(15):2602.
Kuromitsu S, Mori M, Shimada I, Kondoh Y, Shindoh N, Soga T, et al. Abstract A227: Antitumor activities of ASP3026 against EML4-ALK-dependent tumor models. Mol Cancer Ther. 2011;10(1):A227.
Maitland ML, Ou S-HI, Tolcher AW, LoRusso P, Bahceci E, Ball HA, et al. Safety, activity, and pharmacokinetics of an oral anaplastic lymphoma kinase (ALK) inhibitor, ASP3026, observed in a “fast follower” phase 1 trial design. ASCO Meet Abstr. 2014;32(15):2624.
Lovly CM, Heuckmann JM, De Stanchina E, Chen H, Thomas RK, Liang C, et al. Insights into ALK-driven cancers revealed through development of novel ALK tyrosine kinase inhibitors. Cancer Res. 2011;71(14):4920–31.
Weiss GJ, Sachdev JC, Infante JR, Mita MM, Natale RB, Arkenau H-T, et al. Phase (Ph) 1/2 study of TSR-011, a potent inhibitor of ALK and TRK, including crizotinib-resistant ALK mutations. ASCO Meet Abstr. 2014;32(15):e19005.
Infante JR, Camidge DR, Mileshkin LR, Chen EX, Hicks RJ, Rischin D, et al. Safety, pharmacokinetic, and pharmacodynamic phase I dose-escalation trial of PF-00562271, an inhibitor of focal adhesion kinase, in advanced solid tumors. J Clin Oncol. 2012;30(13):1527–33.
Goody MF, Henry CA. Dynamic interactions between cells and their extracellular matrix mediate embryonic development. Mol Reprod Dev. 2010;77(6):475–88.
Ardini E, Menichincheri M, De Ponti C, Amboldi N, Saccardo MB, Texido G, et al. Abstract A243: Characterization of NMS-E628, a small molecule inhibitor of anaplastic lymphoma kinase with antitumor efficacy in ALK-dependent lymphoma and non-small cell lung cancer models. Mol Cancer Ther. 2009;8(1):A244.
Johnson TW, Richardson PF, Bailey S, Brooun A, Burke BJ, Collins MR, et al. Discovery of (10R)-7-amino-12-fluoro-2,10,16-trimethyl-15-oxo-10,15,16,17-tetrahydro-2H-8,4-(m etheno)pyrazolo[4,3-h][2,5,11]-benzoxadiazacyclotetradecine-3-carbonitrile (PF-06463922), a macrocyclic inhibitor of anaplastic lymphoma kinase (ALK) and c-ros oncogene 1 (ROS1) with preclinical brain exposure and broad-spectrum potency against ALK-resistant mutations. J Med Chem. 2014;57(11):4720–44.
Zou HY, Engstrom LR, Li Q, West Lu M, Tang RW, Wang H, et al. Abstract A277: PF-06463922, a novel ROS1/ALK inhibitor, demonstrates sub-nanomolar potency against oncogenic ROS1 fusions and capable of blocking the resistant ROS1G2032R mutant in preclinical tumor models. Mol Cancer Ther. 2013;12(11 Supplement):A277.
Akinleye A, Avvaru P, Furqan M, Song Y, Liu D. Phosphatidylinositol 3-kinase (PI3K) inhibitors as cancer therapeutics. J Hematol Oncol. 2013;6(1):88.
Akinleye A, Chen Y, Mukhi N, Song Y, Liu D. Ibrutinib and novel BTK inhibitors in clinical development. J Hematol Oncol. 2013;6(1):59.
Akinleye A, Furqan M, Mukhi N, Ravella P, Liu D. MEK and the inhibitors: from bench to bedside. J Hematol Oncol. 2013;6(1):27.
Gerecitano J. SINE (selective inhibitor of nuclear export)-translational science in a new class of anti-cancer agents. J Hematol Oncol. 2014;7(1):67.
Parikh K, Cang S, Sekhri A, Liu D. Selective inhibitors of nuclear export (SINE)-a novel class of anti-cancer agents. J Hematol Oncol. 2014;7(1):78.
Shi L, Chen S, Yang L, Li Y. The role of PD-1 and PD-L1 in T-cell immune suppression in patients with hematological malignancies. J Hematol Oncol. 2013;6(1):74.
Acknowledgment
This study was partly supported by Henan Tumor Hospital, Zhengzhou University, Zhengzhou China.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
DL and CI designed the study and drafted the manuscript. All authors have contributed to data preparation, drafting and revising the manuscripts. All authors have read and approved the final manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Iragavarapu, C., Mustafa, M., Akinleye, A. et al. Novel ALK inhibitors in clinical use and development. J Hematol Oncol 8, 17 (2015). https://doi.org/10.1186/s13045-015-0122-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13045-015-0122-8