Abstract
Background
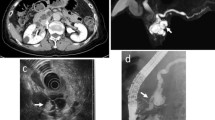
A subset of intraductal papillary mucinous neoplasms (IPMNs) will progress to invasive adenocarcinoma, however identifying invasive from non-invasive disease preoperatively remains challenging. The rate of malignancy in resected IPMNs in the US remains unclear.
Objective
We aimed to determine the rate of malignancy and factors associated with high-risk pathology in resected IPMNs.
Methods
The most recent annual cohort of patients undergoing pancreatectomy included in the American College of Surgeons National Surgical Quality Improvement Program were assessed, and contributions of demographics, preoperative laboratory values, and outcome data to level of IPMN dysplasia were analyzed. The main outcomes were incidence of invasive carcinoma or high-grade dysplasia.
Results
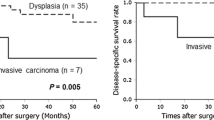
Of 5025 pancreatectomies in 1 year, 478 patients underwent pancreatectomy for IPMN. Invasive carcinoma/high-grade dysplasia was identified in 23% of resected lesions, and there was no difference in patient characteristics or type of resection performed in patients with invasive versus non-invasive pathology. Patients with invasive IPMNs presented significantly more often with high liver function tests, >10% weight loss, clinical jaundice and stent placement, and were more likely to undergo an open operation (p = 0.03). There were no differences in perioperative outcomes. Adjusted logistic regression identified an association between invasive disease and non-soft pancreatic gland texture (odds ratio 0.19, 95% confidence interval 0.05–0.68, p < 0.01).
Conclusions
Approximately 10% of all pancreatectomies in the US are for IPMNs. In these patients, treated after the revised international consensus guidelines, only 23% of IPMNs contained invasive or high-grade histology. Resections carried similar morbidity regardless of pathology. Improved biomarkers are needed to aid in surgical selection.
Similar content being viewed by others
References
Fernández-del Castillo C, Targarona J, Thayer SP, et al. Incidental pancreatic cysts: clinicopathologic characteristics and comparison with symptomatic patients. Arch Surg. 2003;138(4):427–34; discussion 433–4.
Moris M, Bridges MD, Pooley RA, et al. Association between advances in high-resolution cross-section imaging technologies and increase in prevalence of pancreatic cysts from 2005 to 2014. Clin Gastroenterol Hepatol. 2016;14(4):585–93.
Schnelldorfer T, Sarr MG, Nagorney DM, et al. Experience with 208 resections for intraductal papillary mucinous neoplasm of the pancreas. Arch Surg. 2008;143(7):639–46; discussion 646.
Farnell MB. Surgical management of intraductal papillary mucinous neoplasm (IPMN) of the pancreas. J Gastrointest Surg. 2008;12(3):414–6.
Maker AV, Lee LS, Raut CP, et al. Cytology from pancreatic cysts has marginal utility in surgical decision-making. Ann Surg Oncol. 2008;15(11):3187–92.
Suzuki Y, Nakazato T, Yokoyama M, et al. Development and potential utility of a new scoring formula for prediction of malignant intraductal papillary mucinous neoplasm of the pancreas. Pancreas. 2016;45(9):1227–32.
Shin SH, Han DJ, Park KT, et al. Validating a simple scoring system to predict malignancy and invasiveness of intraductal papillary mucinous neoplasms of the pancreas. World J Surg. 2010;34(4):776–83.
Fujino Y, Matsumoto I, Ueda T, et al. Proposed new score predicting malignancy of intraductal papillary mucinous neoplasms of the pancreas. Am J Surg. 2007;194(3):304–7.
Wilson GC, Maithel SK, Bentrem D, et al. Are the current guidelines for the surgical management of intraductal papillary mucinous neoplasms of the pancreas adequate? A multi-institutional study. J Am Coll Surg. 2017;224(4):461–9.
Sahora K, Mino-Kenudson M, Brugge W, et al. Branch duct intraductal papillary mucinous neoplasms: does cyst size change the tip of the scale? A critical analysis of the revised international consensus guidelines in a large single-institutional series. Ann Surg. 2013;258(3):466–75.
Fritz S, Klauss M, Bergmann F, et al. Pancreatic main-duct involvement in branch-duct IPMNs: an underestimated risk. Ann Surg. 2014;260(5):848–55; discussion 855–6.
Reid-Lombardo KM, St Sauver J, Li Z, et al. Incidence, prevalence, and management of intraductal papillary mucinous neoplasm in Olmsted County, Minnesota, 1984–2005: a population study. Pancreas. 2008;37(2):139–44.
Fernández-del Castillo C, Warshaw AL. Cystic tumors of the pancreas. Surg Clin N Am. 1995;75(5):1001–16.
Tanaka M, Chari S, Adsay V, et al. International consensus guidelines for management of intraductal papillary mucinous neoplasms and mucinous cystic neoplasms of the pancreas. Pancreatology. 2006;6(1–2):17–32.
Tanaka M, Fernández-del Castillo C, Adsay V, et al. International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas. Pancreatology. 2012;12(3):183–97.
Fink AS, Campbell DA Jr, Mentzer RM Jr, et al. The National Surgical Quality Improvement Program in non-veterans administration hospitals: initial demonstration of feasibility. Ann Surg. 2002;236(3):344–53; discussion 353-4.
Shimizu Y, Yamaue H, Maguchi H, et al. Predictors of malignancy in intraductal papillary mucinous neoplasm of the pancreas: analysis of 310 pancreatic resection patients at multiple high-volume centers. Pancreas. 2013;42(5):883–8.
Hackert T, Fritz S, Klauss M, et al. Main-duct intraductal papillary mucinous neoplasm: high cancer risk in duct diameter of 5 to 9 mm. Ann Surg. 2015;262(5):875–80; discussion 880–1.
Fan F, Lai EC, Xie F, Yang JM, et al. Intraductal papillary mucinous neoplasms of the pancreas–predictors of malignancy. Hepatogastroenterology. 2010;57(99–100):635–9.
Jang JY, Kim SW, Ahn YJ, et al. Multicenter analysis of clinicopathologic features of intraductal papillary mucinous tumor of the pancreas: is it possible to predict the malignancy before surgery? Ann Surg Oncol. 2005;12(2):124–32.
Kim JR, Jang JY, Kang MJ, et al. Clinical implication of serum carcinoembryonic antigen and carbohydrate antigen 19-9 for the prediction of malignancy in intraductal papillary mucinous neoplasm of pancreas. J Hepatobiliary Pancreat Sci. 2015;22(9):699–707.
Maire F, Voitot H, Aubert A, et al. Intraductal papillary mucinous neoplasms of the pancreas: performance of pancreatic fluid analysis for positive diagnosis and the prediction of malignancy. Am J Gastroenterol. 2008;103(11):2871–7.
Honselmann KC, Patino M, Mino-Kenudson M, et al. Ductal carcinoma arising in a largely unchanged presumed branch-duct IPMN after 10 years of surveillance. Ann Surg. 2017;266(6):e38–40.
Maker AV, Katabi N, Gonen M, et al. Pancreatic cyst fluid and serum mucin levels predict dysplasia in intraductal papillary mucinous neoplasms of the pancreas. Ann Surg Oncol. 2011;18(1):199–206.
Maker AV, Katabi N, Qin LX, et al. Cyst fluid interleukin-1beta (IL1beta) levels predict the risk of carcinoma in intraductal papillary mucinous neoplasms of the pancreas. Clin Cancer Res. 2011;17(6):1502–8.
Maker AV, Carrara S, Jamieson NB, et al. Cyst fluid biomarkers for intraductal papillary mucinous neoplasms of the pancreas: a critical review from the international expert meeting of pancreatic branch-duct-intraductal papillary mucinous neoplasms. J Am Coll Surg. 2015;220(2):243–53.
Tulla KA, Maker AV. Can we better predict the biologic behavior of incidental IPMN? A comprehensive analysis of molecular diagnostics and biomarkers in intraductal papillary mucinous neoplasms of the pancreas. Langenbecks Arch Surg. 2017. https://doi.org/10.1007/s00423-017-1644-z.
Conflicts of interest
Dr. Ajay Maker is supported by an NIH/NCI Grant (K08CA190855). Rym El Khoury, Christopher Kabir, Vijay K. Maker, Mihaela Banulescu, and Margaret Wasserman report no conflicts of interest.
Disclosures
The ACS NSQIP and the hospitals participating in the ACS NSQIP are the source of the data used herein; they have not verified and are not responsible for the statistical validity of the data analysis or the conclusions derived by the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Khoury, R.E., Kabir, C., Maker, V.K. et al. What is the Incidence of Malignancy in Resected Intraductal Papillary Mucinous Neoplasms? An Analysis of Over 100 US Institutions in a Single Year. Ann Surg Oncol 25, 1746–1751 (2018). https://doi.org/10.1245/s10434-018-6425-6
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-018-6425-6