Abstract
Purpose
The aim of this study was to investigate the validity of the management strategy for intraductal papillary mucinous neoplasms (IPMNs) advocated by the international consensus guidelines 2012 (ICG2012).
Methods
The medical records of 49 patients who underwent pancreatectomy for IPMN were retrospectively reviewed.
Results
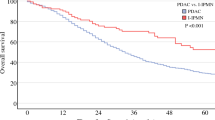
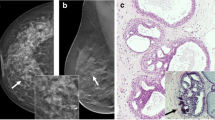
According to preoperative imaging, 10 patients (20 %) had main-duct IPMNs, 20 (41 %) had mixed IPMNs, and 19 (39 %) had branch-duct IPMNs, with malignancy frequencies of 80, 15, and 37 %, respectively. Twenty-seven patients had high-risk stigmata and 21 had worrisome features, with malignancy frequencies of 59 and 10 %, respectively. The sensitivity, specificity, and positive and negative predictive values of high-risk stigmata for malignancy were 88, 65, 59, and 91 %, respectively. Lesions were malignant in 88 % of patients with an enhanced solid component, which was significantly correlated with the prevalence of malignancy (P < 0.01). However, of the 10 patients who underwent pancreatectomy solely due to a main pancreatic dilation of ≥10 mm, 9 (90 %) had benign IPMNs.
Conclusions
Many mixed IPMNs defined according to ICG2012 are benign. Although the management strategy advocated by ICG2012 has been improved relative to the Sendai criteria, the different high-risk stigmata carry unequal weights. Consequently, ICG2012 remains suboptimal for predicting malignant IPMN.


Similar content being viewed by others
References
Furukawa T, Kloppel G, Volkan Adsay N, Albores-Saavedra J, Fukushima N, Hori A, et al. Classification of types of intraductal papillary-mucinous neoplasm of the pancreas: a consensus study. Virchows Arch. 2005;447:794–9.
Maitra A, Fukushima N, Takaori K, Hruban RH. Precursors to invasive pancreatic cancer. Adv Anat Pathol. 2005;12:81–91.
Tanaka M, Chari S, Adsay V, Fernandez-del Castillo C, Falconi M, Shimizu M, et al. International consensus guidelines for management of intraductal papillary mucinous neoplasms and mucinous cystic neoplasms of the pancreas. Pancreatology. 2006;6:17–32.
Tanaka M, Fernandez-del Castillo C, Adsay V, Chari S, Falconi M, Jang JY, et al. International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas. Pancreatology. 2012;12:183–97.
Tamura K, Ohtsuka T, Ideno N, Aso T, Shindo K, Aishima S, et al. Treatment strategy for main duct intraductal papillary mucinous neoplasms of the pancreas based on the assessment of recurrence in the remnant pancreas after resection: a retrospective review. Ann Surg. 2014;259:360–8.
Roch AM, Ceppa EP, DeWitt JM, Al-Haddad MA, House MG, Nakeeb A, et al. International consensus guidelines parameters for the prediction of malignancy in intraductal papillary mucinous neoplasm are not properly weighted and are not cumulative. HPB Oxf. 2014;16:929–35.
Aso T, Ohtsuka T, Matsunaga T, Kimura H, Watanabe Y, Tamura K, et al. “High-risk stigmata” of the 2012 international consensus guidelines correlate with the malignant grade of branch duct intraductal papillary mucinous neoplasms of the pancreas. Pancreas. 2014;43:1239–43.
Adsay NV, Fukushima N, Furukawa T, Hruban RH, Klimstra DS, Koppel G, et al. Intraductal neoplasms of the pancreas. In: Bosman FT, Carneiro F, Hruban RH, Theise ND, editors. WHO classification of tumors of the digestive system. Lyon: IARC Press; 2010. p. 304–13.
Bournet B, Kirzin S, Carrere N, Portier G, Otal P, Selves J, et al. Clinical fate of branch duct and mixed forms of intraductal papillary mucinous neoplasia of the pancreas. J Gastroenterol Hepatol. 2009;24:1211–7.
Nara S, Onaya H, Hiraoka N, Shimada K, Sano T, Sakamoto Y, et al. Preoperative evaluation of invasive and noninvasive intraductal papillary-mucinous neoplasms of the pancreas: clinical, radiological, and pathological analysis of 123 cases. Pancreas. 2009;38:8–16.
Sohn TA, Yeo CJ, Cameron JL, Hruban RH, Fukushima N, Campbell KA, et al. Intraductal papillary mucinous neoplasms of the pancreas: an updated experience. Ann Surg. 2004;239:788–97.
Suzuki Y, Atomi Y, Sugiyama M, Isaji S, Inui K, Kimura W, et al. Cystic neoplasm of the pancreas: a Japanese multiinstitutional study of intraductal papillary mucinous tumor and mucinous cystic tumor. Pancreas. 2004;28:241–6.
Crippa S, Fernandez-del Castillo C, Salvia R, Finkelstein D, Bassi C, Dominguez I, et al. Mucin-producting neoplasms of the pancreas: an analysis of distinguishing clinical and epidemiologic characteristics. Clin Gastroenterol Hepatol. 2010;8:213–9.
Schnelldorfer T, Sarr MG, Nagorney DM, Zhang L, Smyrk TC, Qin R, et al. Experience with 208 resections for intraductal papillary mucinous neoplasm of the pancreas. Arch Surg. 2008;143:639–46.
Pelaez-Luna M, Chari ST, Smyrk TC, Takahashi N, Clain JE, Levy MJ, et al. Do consensus indications for resection in branch-duct intraductal papillary mucinous neoplasm predict malignancy? A study of 147 patients. Am J Gastroenterol. 2007;102:1759–64.
Tang RS, Weinberg B, Dawson DW, Reber R, Hines OJ, Tomlinson JS, et al. Evaluation of the guidelines for management of pancreatic branch-duct intraductal papillary mucinous neoplasm. Clin Gastroenterol Hepatol. 2008;6:815–9.
Nagai K, Doi R, Ito T, Kida A, Koizumi M, Masui T. Single-institution validation of the international consensus guidelines for treatment of branch duct intraductal papillary mucinous neoplasms of the pancreas. J Hepatobiliary Pancreat Surg. 2009;16:353–8.
Cameron JL, Riall TS, Coleman J, Belcher KA. One thousand consecutive pancreaticoduodenectomies. Ann Surg. 2006;244:10–5.
Watanabe Y, Ohtsuka T, Kimura H, Matsunaga T, Tamura K, Ideno N, et al. Braun enteroenterostomy reduces delayed gastric emptying after pylorus-preserving pancreatoduodenectomy: a retrospective review. Am J Surg. 2015;209:369–77.
Kuroki T, Eguchi S. Laparoscopic distal pancreatosplenectomy for pancreatic ductal adenocarcinoma. Surg Today. 2015;45:808–12.
Zhang X, Ma L, Gao X, Bao H, Liu P, Aziz A, et al. Pancreaticogastrostomy versus pancreaticojejunostomy reconstruction after pancraeticoduodenectomy: a meta-analysis of randomized controlled trials. Surg Today. 2015;45:585–94.
Koshita S, Fujita N, Noda Y, Kobayashi G, Ito K, Horaguchi J, et al. Invasive carcinoma derived from “flat type” branch duct intraductal papillary mucinous neoplasms of the pancreas: impact of classification according to the height of mural nodule on endoscopic ultrasonography. J Hepatobiliary Pancreat Sci. 2015;22:301–9.
Kobayashi G, Fujita N, Noda Y, Obana T, Takasawa O. Ultrasonographic findings and natural history of intraductal papillary-mucinous neoplasms of the pancreas. J Med Ultrasonics. 2008;35:85–96.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Rights and permissions
About this article
Cite this article
Watanabe, Y., Nishihara, K., Niina, Y. et al. Validity of the management strategy for intraductal papillary mucinous neoplasm advocated by the international consensus guidelines 2012: a retrospective review. Surg Today 46, 1045–1052 (2016). https://doi.org/10.1007/s00595-015-1292-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-015-1292-2