Abstract
Background
Mastectomy is associated with postoperative nausea and pain. We evaluated whether paravertebral block (PVB) use altered opioid use, antiemetic use, and length of stay in patients undergoing mastectomy.
Methods
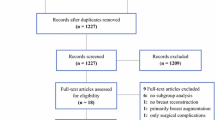
We performed a retrospective cohort analysis of all patients who underwent mastectomy with or without PVB from 2008 to 2010. Patient demographics, operative procedure, intraoperative medications, postoperative opioid and antiemetic use, and length of stay were reviewed. Statistical analysis included univariable and multivariable analysis.
Results
A total of 605 patients were identified, of whom 526 patients were evaluable. A total of 294 patients underwent mastectomy without PVB (132 bilateral), and 232 patients underwent mastectomy with PVB (148 bilateral). Immediate reconstruction was performed in 203 (39 %) patients. Need for any postoperative antiemetic was less frequent in the PVB group (39 vs. 57 %, p < 0.0001). Day of surgery opioid use was lower in the PVB group than the non-PVB group (mean ± SD 40.1 ± 15.2 vs. 47.6 ± 17.7 morphine equivalents, p < 0.0001). Decreased opioid use was seen in unilateral mastectomy without reconstruction and bilateral mastectomy with and without immediate reconstruction. The proportion of patients discharged within 36 h of surgery was significantly higher in the PVB group (55 vs. 42 %, p = 0.0031). On multivariable analysis controlling for year of surgery, patient age and surgeon, PVB use affected antiemetic use and opioid use but not hospital length of stay.
Conclusions
PVB results in decreased opioid use and decreased need for postoperative antiemetic medication in patients undergoing mastectomy. The greatest benefit is seen in patients undergoing bilateral mastectomy with immediate breast reconstruction.
Similar content being viewed by others
References
Vadivelu N, Schreck M, Lopez J, Kodumudi G, Narayan D. Pain after mastectomy and breast reconstruction. Am Surg. 2008;74:285–96.
Voight M, Frohlich CW, Waschke KF, Lenz C, Gobel U, Kerger H. Prophylaxis of postoperative nausea and vomiting in elective breast surgery. J Clin Anesth. 2011;23:461–8.
Ahmed J, Lim M, Khan S, McNaught C, Macfie J. Predictors of length of stay in patients having elective colorectal surgery within an enhanced recovery protocol. Int J Surg. 2010;8:628–32.
Habermann EB, Abbott A, Parsons HM, Virnig BA, Al-Refaie WB, Tuttle TM. Are mastectomy rates really increasing in the United States? J Clin Oncol. 2010;28:3437–41.
Boughey JC, Hieken T, Degnim AC, Jakub JW, Hoskin T. Increase in contralateral prophylactic mastectomy rates is associated with increased use of immediate reconstruction. Paper presented at: 67th Annual Meeting of Society of Surgical Oncology, March 12–15, 2014, Phoenix, AZ.
Yeh CC, Yu JC, Wu CT, Ho ST, Chang TM, Wong CS. Thoracic epidural anesthesia for pain relief and postoperation recovery with modified radical mastectomy. World J Surg. 1999;23:256–60.
Layeeque R, Hochberg J, Siegel E, et al. Botulinum toxin infiltration for pain control after mastectomy and expander reconstruction. Ann Surg. 2004;240:608–13.
Rica MA, Norlia A, Rohaizak M, Naqiyah I. Preemptive ropivacaine local anaesthetic infiltration versus postoperative ropivacaine wound infiltration in mastectomy: postoperative pain and drain outputs. Asian J Surg. 2007;30:34–9.
Grover VK, Matthew PJ, Yaddanapudi S, Sehgal S. A single dose of preoperative gabapentin for pain reduction and requirement of morphine after total mastectomy and axillary dissection: randomized placebo-controlled double-blind trial. J Postgrad Med. 2009;55:257–60.
Boughey JC, Goravanchi F, Parris RN, et al. Improved postoperative pain control using thoracic paravertebral block for breast operations. Breast J. 2009;15:483–8.
Aufforth R, Jain J, Morreale J, Baumgarten R, Falk J, Wesen C. Paravertebral blocks in breast cancer surgery: is there a difference in postoperative pain, nausea, and vomiting? Ann Surg Oncol. 2012;19:548–52.
Bauer M, George JE 3rd, Seif J, Farag E. Recent advances in epidural analgesia. Anesthesiol Res Pract. 2012;2012:309219.
Bhuvaneswari V, Wig J, Mathew PJ, Singh G. Post-operative pain and analgesic requirements after paravertebral block for mastectomy: a randomized controlled trial of different concentrations of bupivacaine and fentanyl. Indian J Anaesth. 2012;56:34–9.
Terheggen MA, Wille F, Borel Rinkes IH, Ionescu TI, Knape JT. Paravertebral blockade for minor breast surgery. Anesth Analg. 2002;94:355–9.
Boughey JC, Goravanchi F, Parris RN. Prospective randomized trial of paravertebral block for patients undergoing breast cancer surgery. Am J Surg. 2009;198:720–5.
Abdallah FW, Morgan PJ, Cil T, et al. Ultrasound-guided multilevel paravertebral blocks and total intravenous anesthesia improve the quality of recovery after ambulatory breast tumor resection. Anesthesiology. 2014;120:703–13.
Chiu M, Bryson GL, Lui A, Watters JM, Taljaard M, Nathan HJ. Reducing persistent postoperative pain and disability 1 year after breast cancer surgery: a randomized, controlled trial comparing thoracic paravertebral block to local anesthetic infiltration. Ann Surg Oncol. 2014;21:795–801.
Coopey SB, Specht MC, Warren L, Smith BL, Winograd JM, Fleischmann K. Use of preoperative paravertebral block decreases length of stay in patients undergoing mastectomy plus immediate reconstruction. Ann Surg Oncol. 2013;20:1282–6.
Niesen A. How I do it: ultrasound-guided thoracic paravertebral block. ASRA News. 2009;14–16. Available at: http://www.asra.com/Newsletters/Nov_09.pdf.
Serlin RC, Mendoza TR, Nakamura Y, Edwards KR, Cleeland CS. When is cancer pain mild, moderate or severe? Grading pain severity by its interference with function. Pain. 1995;61:277–84.
Coveney E, Weltz CR, Greengrass R, et al. Use of paravertebral block anesthesia in the surgical management of breast cancer: experience in 156 cases. Ann Surg. 1998;227:496–501.
Disclosure
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fahy, A.S., Jakub, J.W., Dy, B.M. et al. Paravertebral Blocks in Patients Undergoing Mastectomy with or without Immediate Reconstruction Provides Improved Pain Control and Decreased Postoperative Nausea and Vomiting. Ann Surg Oncol 21, 3284–3289 (2014). https://doi.org/10.1245/s10434-014-3923-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-014-3923-z