Abstract
Background
Positive resection margins are amongst the strongest predictors of cancer-related mortality for adenocarcinoma of the stomach and esophagus. Although intraoperative pathology consultation with frozen section of margins can predict final permanent section pathology, the accuracy of this approach is not known. We sought to determine the diagnostic accuracy of frozen section margin analysis in esophagogastric adenocarcinoma and the impact that it had on surgical therapy.
Methods
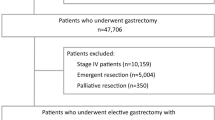
Patients with resection of esophagogastric adenocarcinoma at a single centre from 1998 to 2008 were identified. Clinicopathologic data were collected. Frozen section results were compared to permanent section assessment, and sensitivity, specificity, positive, and negative predictive values were calculated. Patients with positive margins by frozen section were reviewed to assess the impact on surgical decision-making.
Results
Of 220 patients who underwent surgery for adenocarcinoma of the esophagus and stomach (esophagus: 34/220, EGJ: 106/220, stomach 80/220), 56 % had an intraoperative consultation. Of these 122 patients, 66 % underwent frozen section. All errors on frozen section occurred on the interpretation of the proximal margin. The diagnostic accuracy of frozen section at the proximal margin was 93 % with sensitivity = 67 %, specificity = 100 %, positive predictive value = 100 %, and negative predictive value = 91 %. Signet ring cells were present in 83 % of false-negative readings. Surgical management was altered in 10 of the 13 of patients who had a true positive frozen section and 9 of these patients were converted to R0 resections.
Conclusions
Although very specific, negative results on frozen section require greater caution when signet ring cells are present. For esophagogastric adenocarcinoma, frozen section alters management and may increase the rate of complete resection.

Similar content being viewed by others
References
Pohl H, Welch HG. The role of overdiagnosis and reclassification in the marked increase of esophageal adenocarcinoma incidence. J Natl Cancer Inst. 2005;97(2):142–6.
Law S, Arcilla C, Chu KM, Wong J. The significance of histologically infiltrated resection margin after esophagectomy for esophageal cancer. Am J Surg. 1998;176(3):286–90.
Mattioli S, Di Simone MP, Ferruzzi L, D’Ovidio F, Pilotti V, Carella R et al. Surgical therapy for adenocarcinoma of the cardia: modalities of recurrence and extension of resection. Dis Esophagus. 2001;14(2):104–9.
Mariette C, Castel B, Balon JM, Van Seuningen I, Triboulet JP. Extent of oesophageal resection for adenocarcinoma of the oesophagogastric junction. Eur J Surg Oncol. 2003;29(7):588–93.
Ferri LE, Law S, Wong KH, Kwok KF, Wong J. The influence of technical complications on postoperative outcome and survival after esophagectomy. Ann Surg Oncol. 2006;13(4):557–64.
Cunningham D, Allum WH, Stenning SP, Thompson JN, Van de Velde CJ, Nicolson M, et al. Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N Engl J Med. 2006;355(1):11–20.
Barbour AP, Rizk NP, Gonen M, Tang L, Bains MS, Rusch V, et al. Adenocarcinoma of the gastroesophageal junction: influence of esophageal resection margin and operative approach on outcome. Ann Surg. 2007;246(1):1–8.
Casson AG, Darnton SJ, Subramanian S, Hiller L. What is the optimal distal resection margin for esophageal carcinoma? Ann Thorac Surg. 2000;69(1):205–9.
Kuwano H, Masuda N, Kato H, Sugimachi K. The subepithelial extension of esophageal carcinoma for determining the resection margin during esophagectomy: a serial histopathologic investigation. Surgery. 2002;131(1 Suppl):S14–21.
Younes M. Frozen section of the gastrointestinal tract, appendix, and peritoneum. Arch Pathol Lab Med. 2005;129(12):1558–64.
Matsusaka S, Nagareda T, Yamasaki H, Kitayama Y, Okada T, Maeda S. Immunohistochemical evaluation for intraoperative rapid pathological assessment of the gastric margin. World J Surg. 2003;27(6):715–8.
Chan WH, Wong WK, Khin LW, Chan HS, Soo KC. Significance of a positive oesophageal margin in stomach cancer. Aust N Z J Surg. 2000;70(10):700–3.
Papachristou DN, Agnanti N, D’Agostino H, Fortner JG. Histologically positive esophageal margin in the surgical treatment of gastric cancer. Am J Surg. 1980;139(5):711–3.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Spicer, J., Benay, C., Lee, L. et al. Diagnostic Accuracy and Utility of Intraoperative Microscopic Margin Analysis of Gastric and Esophageal Adenocarcinoma. Ann Surg Oncol 21, 2580–2586 (2014). https://doi.org/10.1245/s10434-014-3669-7
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-014-3669-7