Abstract
To ensure consistency of clinical outcomes, orally inhaled therapies must exhibit consistent delivered dose and aerosol properties at the time of manufacturing, throughout storage, and during various patient-use conditions. Achieving consistency across these scenarios has presented a significant challenge, especially for combination products that contain more than one drug. This study characterized the delivered dose and aerosol properties of glycopyrrolate/formoterol fumarate metered dose inhaler (GFF MDI; Bevespi Aerosphere™). GFF MDI, a fixed-dose combination (FDC) of a long-acting muscarinic antagonist, glycopyrrolate (18 μg, equivalent to glycopyrronium 14.4 μg), and a long-acting β2-agonist, formoterol fumarate (9.6 μg; equivalent to formoterol fumarate dihydrate 10 μg), is formulated using innovative co-suspension delivery technology, which suspends micronized drug crystals with spray-dried phospholipid porous particles in hydrofluoroalkane propellant. In this study, delivered dose uniformity was assessed through the labeled number of doses, and aerosol properties, such as percent fine particle fraction (FPF) and mass median aerodynamic diameter, were determined by cascade impaction. GFF MDI achieved reproducible dose delivery and an FPF greater than 55%, whether formulated and delivered as a monocomponent or dual FDC. The performance of GFF MDI was maintained across various manufacturing batches, under extended storage, and with variations in flow rate. Furthermore, unlike a GFF drug crystal-only suspension, drug delivery remained consistent for GFF MDI when simulated patient-handling errors were applied, such as reduced shake energy and delays between shaking and actuation. These results demonstrate that co-suspension delivery technology overcomes well-known sources of variability in MDI drug delivery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Chronic respiratory disease is a significant cause of morbidity and mortality worldwide. Global prevalence rates for asthma and chronic obstructive pulmonary disease (COPD) alone are estimated to be more than 400 million, with COPD being the fourth worldwide leading cause of death (1). For the treatment of these diseases, drugs are often delivered to the lung using an inhalation delivery device, which include pressurized metered dose inhalers (MDIs), dry powder inhalers (DPI), soft mist inhalers (SMIs), and nebulizers. Each type of inhalation device has its own unique benefits and challenges in terms of formulation requirements and patient usability that should be considered when developing a respiratory drug product. There is also a growing body of evidence showing the nature and extent of user error that inhalation devices are prone to (2–4). Some errors can be addressed by more effective patient education, but advances in inhalation product and device technologies are also needed to improve their usability and ultimately achieve better health outcomes for patients.
Of the available inhalation devices, MDIs are the most widely used worldwide by volume with more than 500 million units estimated to be produced annually (5). MDI formulations can be categorized as solution- or suspension-based depending on whether the drug is in a solution or solid form. For solution-based MDIs, the drug is dissolved and homogeneously dispersed throughout the liquid propellant; however, their broad application is limited by poor drug solubility in propellant. Achieving a solution MDI formulation is particularly challenging when two or more drugs are formulated together because the solubility of both drugs in propellant and excipient selection (e.g. ethanol) needs to be considered, along with the impact on product performance and stability (6,7).
For suspension-based MDIs, micronized drug crystals are suspended in propellant, often aided by suspension-stabilizing excipients (6–9). To ensure that each aerosol spray contains a consistent dose of drug on every actuation, it is critical for the drug, or drugs, in a suspension-based MDI to be physically stable (e.g., no particle growth or irreversible agglomeration) and evenly dispersed throughout the liquid propellant at the time of administration (6). However, the change from chlorofluorocarbon (CFC) to hydrofluoroalkane (HFA) propellants created formulation challenges, with many of the drug microcrystal-based HFA MDIs having poor colloidal stability that results in rapid creaming or sedimentation, which can then lead to dosing variability (8,9).
The difficulties in achieving dosing consistency with suspension MDIs may be exacerbated by errors in patient-handling techniques. Previous studies have shown that compliance with MDI instructions for use, particularly inhalation maneuvers and shaking technique, can be poor among patients (3,10–12). In general, press-and-breathe MDIs require coordination between actuation and inhalation, as well as a relatively low inspiratory flow rate (13). Additionally, for suspension-based MDIs, effective shaking prior to dosing is necessary in order to ensure consistent drug delivery (3,14). Improper inhaler technique during dose administration therefore may result in patients receiving incorrect doses during their treatment period that has the potential to affect clinical outcomes (3).
Pearl Therapeutics Inc. has developed co-suspension delivery technology, an innovative MDI formulation that suspends micronized drug crystals with spray-dried phospholipid excipient porous particles in HFA propellant (8). Co-suspension delivery technology addresses some of the key formulation challenges affecting suspension MDIs that can be applied to drugs, or combinations of drugs, with varying physicochemical properties and across a wide concentration range (8). Additional excipients, such as co-solvents or suspension stabilizers, are no longer needed because the porous particles spontaneously form physically stable and easily dispersible suspensions in HFA propellants, whether co-suspended with micronized drug crystals (8), or when drug is incorporated into the particles (15). Co-suspension delivery technology was used in the development of GFF MDI, a bronchodilator fixed-dose combination (FDC) of glycopyrrolate (GP), a long-acting muscarinic antagonist, at a twice-daily dose of 18 μg (equivalent to 14.4 μg of glycopyrronium), and formoterol fumarate (FF), a long-acting β2-agonist, at a twice-daily dose of 9.6 μg (equivalent to formoterol fumarate dihydrate 10 μg). GFF MDI was approved recently by the US Food and Drug Administration as a long-term maintenance treatment for airflow obstruction in patients with COPD (16).
Here, we aimed to demonstrate that improvements in MDI suspension formulation can be used to overcome variability in dose delivery, particularly those that result from patient-handling errors. To achieve this, a series of in vitro delivered dose and aerodynamic particle size distribution (aPSD) experiments were performed with GFF MDI to evaluate product performance across multiple batches, storage periods, inhalation flow rates, and use conditions. In addition, for those studies evaluating variations in shaking technique and prolonged delays from shake to actuate, a drug crystal-only MDI with the same drug composition and device, but no porous particles, was used to identify the attributes of GFF MDI product reliability that depend on co-suspension delivery technology.
MATERIALS AND METHODS
MDI Formulation
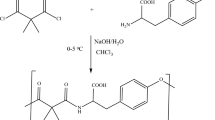
Monocomponent and dual FDC MDIs containing GP and/or FF were prepared by simultaneously suspending the micronized drug particles with spray-dried phospholipid porous particles (“porous particles”; Fig. 1) in HFA-134a propellant. Drug microcrystals were produced by air-jet milling. The manufacturing process for phospholipid porous particles has been described before (17). Briefly, an emulsion feedstock with 1,2-distearoyl-sn-glycero-3-phosphocholine (DSPC) and anhydrous CaCl2 (equivalent to a 2:1 DSPC/CaCl2 molar ratio) was prepared. During the emulsion preparation, DSPC and CaCl2 were dispersed into a vessel containing heated water and perfluorooctyl bromide (perflubron) using a high-shear mixer. The coarse emulsion was then further processed with a high-pressure homogenizer before spray-drying (18). Commercially available pressure filling equipment was used for MDI manufacturing (19). The suspension was filled into 14-mL aluminum canisters (H&T Presspart GmbH & Co. KG, Marsberg, Germany) through 50-μL valves (Bespak, King’s Lynn, UK). For the preparation of the drug crystal-only MDIs tested for comparison, the porous particles were excluded with all other aspects of the preparation process and container closure system remaining the same.
Sample canisters were selected during manufacture for total canister drug content analysis to ensure correct formulation quantities. MDIs were held for a minimum of 1 week prior to aerosol performance testing. All aerosol performance testing was performed with a 0.30-mm spray orifice diameter actuator (Bespak, King’s Lynn, UK).
Aerosol Performance
Aerosol performance was tested using the method described in the United States Pharmacopeia (USP) Chapter ⟨601⟩ and a manual shake maneuver of 15 vertical shakes in 5 s, unless otherwise specified. All aerosol performance collections were performed by manual actuation. Waste actuations between the beginning and end of MDI-labeled actuations were automated (FD-10, Innova Systems, Inc., Moorestown, NJ, USA). A Next Generation Impactor™ (NGI; MSP Corporation, St. Paul, MN, USA) cascade impactor operated at an air flow rate of 30 L/min was used for determination of the aPSD. For these tests, the MDI was attached to the NGI via a Delrin® mouthpiece adapter and USP induction port (USP Throat; MSP Corporation, St. Paul, MN, USA). Additional flow rates of 15 to 90 L/min were analyzed for flow-rate dependency. The volume of inhalation was held constant at 4 L. Sample canisters were seated into actuators with two seating waste actuations and primed with two additional actuations. Two to five actuations, depending on the study, were collected in the NGI with a USP induction port attached. The valve stem, actuator, induction port, NGI collection stages, and micro-orifice collector were rinsed with volumetrically dispensed solvent. The sample solutions were assayed using a drug-specific high-performance liquid chromatography method. The fine particle dose was defined as the mass of particles with an aPSD less than 5.0 μm, an interpolated value. To allow comparisons of inhalers with different dose strengths, the fine particle fraction (FPF) was used. FPF is calculated by normalizing the fine particle dose by the emitted dose (sum of mass deposited on the mouthpiece adapter, throat, stages 1–7, and micro-orifice collector). From the aPSD, a mass median aerodynamic diameter (MMAD) was also obtained, consistent with USP ⟨601⟩.
Delivered dose uniformity through canister life testing was performed using a Dose Uniformity Sampling Apparatus as described by USP ⟨601⟩. Inhalers were seated and primed as described before. Two actuations were collected and assayed at the beginning and throughout product life, depending on the study.
The effect of shaking variation on delivered dose was assessed using three manual shaking maneuvers: (i) a standard control shake (15 shakes in 5 s), (ii) a slow gentle shake (3 shakes in 5 s), and (iii) a single vertical inversion. The delivered dose result following each shaking maneuver was normalized to the result obtained with the standard control shake. The effect of a delay from the time of actuation to the time of dose collection on delivered dose was assessed for delay times of 0, 2, 5, 10, 30, and 60 s for a drug crystal-only MDI and GFF MDI. The delivered dose result for each delay was normalized to the result obtained with no delay. The percent intra-can difference in drug delivery between GP and FF was calculated for each canister. This was done at the delay time of 60 s by subtracting the delivered dose of GP (as a % of the label claim dose) from the delivered dose of FF (as a % of the label claim dose). An overall mean was calculated by dividing the sum of the individual percent intra-can difference values by the total number of samples. The percent intra-can difference was calculated for the drug crystal-only MDI and GFF MDI.
Statistical Analysis
To evaluate in vitro statistical equivalence of the mono and dual FDC MDI suspension (Table I), a two one-sided t test (JMP Statistical Software, SAS, Cary, NC, USA) was performed on the FPF results from the aerodynamic particle size distributions (Fig. 2). A two-sided 90% confidence interval was calculated for the true mean difference between GFF MDI and the corresponding monocomponent MDIs. Statistical equivalence is met if the 90% confidence interval is fully contained within a practical equivalence threshold, θ, of 10% (Table I).
The aerodynamic particle size distribution of a GP and b FF are consistent when formulated and delivered as either a monocomponent (GP MDI or FF MDI) or dual FDC (GFF MDI). N = 5 NGI per product were performed. FDC fixed-dose combination; FF formoterol fumarate; GFF glycopyrrolate/formoterol fumarate; GP glycopyrrolate; MDI metered dose inhaler; MOC micro-orifice collector; NGI Next Generation Impactor. Error bars correspond to ± 1 standard deviation
RESULTS
Performance of Dual FDC MDI Developed Using Co-suspension Delivery Technology
To first demonstrate that combining two drugs into an FDC does not change the aerosol performance of each individual component, the aerosol performance of each drug in GFF MDI was compared with the corresponding monocomponent MDI (GP MDI or FF MDI). The aPSD for GP formulated using co-suspension delivery technology was similar in both the monocomponent formulation and the dual FDC formulation (GP MDI and GFF MDI, respectively; Fig. 2a). The same patterns of consistent aerosol performance between the monocomponent and dual FDC MDIs were upheld for FF (Fig. 2b). Furthermore, the FPF and MMAD of the therapeutic agents remained consistent regardless of whether they were delivered from a mono or dual FDC MDI suspension (Table I). The 90% confidence interval for the mean difference in FPF between the monocomponents and dual FDC MDI was contained within the equivalence threshold of 10% for both drugs (p < 0.0001; Table I). These results show that the aerosol performance of the two drugs, GP and FF, was consistent when formulated with co-suspension delivery technology as either monocomponent MDIs or in a dual FDC MDI.
Batch-to-Batch Consistency and Shelf-Life Stability
To investigate the batch-to-batch consistency and shelf-life stability of GFF MDI, delivered dose uniformity through canister life was tested in three primary stability batches (> 1000 canisters) that were stored up to 24 months at 25°C/60% relative humidity (long-term storage condition per International Council for Harmonization Stability Testing for New Drug Substances Q1A Revision 2). Stability samples were packaged in foil pouches with desiccant during storage. Samples were tested at initial and after storage for 1, 3, 6, 12, 15, 18, 21, and 24 months. The distribution of delivered dose results on stability for both GP and FF are shown in Fig. 3. Throughout the shelf-life of GFF MDI, > 99% of doses were within 75–125% of label claim (LC). Furthermore, the mean delivered doses through 24 months of shelf-life were 100.3 and 100.9% LC for GP and FF, respectively. These results demonstrated that GFF MDI provides a consistent and stable dose, independent of batch, throughout the shelf-life of the product.
Consistent delivered dose of GFF MDI is achieved across multiple MDI batches through 24 months of storage at 25°C/60% RH for both GP (green) and FF (blue). The mean result for both GP and FF was 100.3% and 100.9% of LC from 2040 total data points, respectively. The vertical dashed lines represent ± 25% of LC. N = 1020 delivered dose were collected. FF formoterol fumarate; GFF glycopyrrolate/formoterol fumarate; GP glycopyrrolate; LC label claim; MDI metered dose inhaler; RH relative humidity
Consistent Aerosol Performance Independent of Flow Rate
The inhalation rate and volume for patients with COPD can vary based on the individual, as well as the severity of the disease and resistance of the device used for treatment (13), and failure to inhale at the correct flow rate is one of the most common MDI user errors (20,21). Unlike DPIs, which require a fast and strong inhalation at a flow rate > 30 L/min to move the powder from the device into the airways, MDIs require a slow and deep inhalation with typical peak inspiration flow rates of ≤ 90 L/min (13). To assess the effect of varying flow rate on the aerosol performance of GFF MDI, the FPF and MMAD were determined for continuous in vitro flow rates of 15–90 L/min (Fig. 4). These flow rates were comparable with typical peak inspiratory flow rates of patients with COPD (13) and also produced a range of inhalation volumes since the MDI plume duration is constant regardless of the test flow rate. Moreover, peak inspiratory flow rates < 30 L/min are not common for patients with COPD, particularly using an MDI device (13,22), and therefore 15 L/min in these experiments may be more indicative of a low volume inhalation such as tidal breathing. For GFF MDI, a consistent FPF (< 5 μm) of > 55% was observed for both drugs at flow rates of 30–90 L/min, which ranged from 61–69% FPF. At 15 L/min, an FPF of 48% was still achieved. These FPF results are comparable with, or higher than, other MDIs (23–27). In addition, the measured MMAD results for GFF MDI across the range of flow rates (15–90 L/min) were 3.0–3.2 μm for GP and 2.8–3.1 μm for FF. These results were consistent across flow rates and comparable with the MMAD values observed for the monocomponent and dual FDC MDIs shown in Table I, indicating minimal impact of inhalation flow rate on the GFF MDI in vitro aerosol performance. Overall, these results showed GFF MDI performance is consistent across a broad range of inspiratory flow rates.
The FPF (< 5 μm) of GFF MDI, formulated using the co-suspension delivery technology, is consistent across a broad range of continuous in vitro flow rates. N = 5 NGI were collected per flow rate. FF formoterol fumarate; FPF fine particle fraction; GFF glycopyrrolate/formoterol fumarate; GP glycopyrrolate; MDI metered dose inhaler; NGI Next Generation Impactor
Delivered Dose of GFF MDI Compared with Drug Crystal-Only MDI Without Co-suspension Delivery Technology
To confirm that the consistent performance of GFF MDI is dependent on the co-suspension delivery technology, drug delivery was determined for both GFF MDI and a settling drug crystal-only MDI (no porous particles) for doses at the beginning, middle, and end of the MDI labeled canister actuations. GFF MDI employing co-suspension delivery technology demonstrated consistent delivered dose from the first usable actuation to the last, with all doses within ± 10% of the LC dose for both GP and FF (Fig. 5). For the drug crystal-only MDI, increased variability was observed from beginning to end of product life, with doses ranging from 85 to 150% LC for both drugs.
The delivered dose of GFF MDI from the first to the last labeled actuation compared with a drug crystal-only MDI shows more consistent drug delivery when using the co-suspension delivery technology. N = 30 delivered dose were collected for each product. DT delivery technology; GFF glycopyrrolate/formoterol fumarate; MDI metered dose inhaler
In Vitro Performance with Handling Errors: Variable Shake Technique
A common mistake in patient inhaler technique is the failure to sufficiently shake the MDI prior to taking a dose (3). To evaluate the impact of shake energy on drug delivery consistency, GFF MDI and the drug crystal-only MDI were subjected to one of three different shake energy maneuvers prior to obtaining the delivered dose: (i) a standard shake (15 shakes in 5 s), (ii) a gentle shake (5 shakes in 5 s), and (iii) a single inversion to simulate lifting the device from a rest position.
When the modified shake maneuvers of either a single inversion or gentle shake were applied, GFF MDI delivered a consistent dose, within 25% of the target dose produced by the standard control shake, for all results except one (Fig. 6). By comparison, the drug crystal-only MDI displayed marked variability, particularly for the gentle shake group, with delivered dose results ranging from 40 to 170% of the standard shake. These results demonstrate that the co-suspension delivery technology enables more robust and consistent drug delivery under gentle shaking conditions, which may translate to the GFF MDI being less susceptible to drug delivery variability as a result of patient shaking technique.
GFF MDI formulation with the co-suspension delivery technology shows consistent delivered dose irrespective of shake techniques (relative to a standard control shake). In contrast, a drug crystal-only MDI showed increased variation in drug delivery, particularly when a gentle shake was applied. All results are presented relative to the standard shake delivered dose. N = 10 delivered dose were collected per product and shake type. DT delivery technology; FF formoterol fumarate; GFF glycopyrrolate/formoterol fumarate; GP glycopyrrolate; MDI metered dose inhaler
In Vitro Performance with Handling Errors: Variable Delays from Shake to Actuation
In the ideal patient setting, a dose would be administered as soon as possible following MDI shaking, but these details are typically not provided in patient instructions. In actual use, delays may occur between shaking and actuation, which could result in drug delivery higher or lower than the intended dose, depending on the rate at which a suspension-based MDI settles or creams (14). To evaluate this minor handling error scenario, GFF MDI delivered dose was characterized with delays imparted from shake to actuation of up to 60 s and compared with the drug crystal-only MDI. During the delay, MDIs were held valve down. The results for both MDI formulations were normalized to the mean of the no delay control group. GFF MDI drug delivery remained within 10% of the control for both GP and FF with delays from shake to actuation of up to 60 s (Fig. 7). Comparatively, drug delivery for the drug crystal-only MDIs showed increased variability and divergence from the control, with the delivered dose of GP exceeding 115 and 120% of the control for delays of 10 and 60 s, respectively. Furthermore, the mean percent intra-can difference in drug delivery (% difference GP-FF) was approximately 6% for the drug crystal-only MDI suspension following a 60-s delay from shake to actuate, compared with a mean percent intra-can difference of < 1% for GFF MDI. Taken together, these results provide further evidence that GFF MDI, when formulated with the co-suspension delivery technology, maintains drug delivery consistency when simulated handling errors are applied.
Delay from shake to actuation of up to 60 s does not impact mean delivered dose of GP and FF more than 10% for GFF MDI, which is formulated with the co-suspension delivery technology MDI. In contrast, the drug crystal-only MDI group showed higher variability in drug delivery with delays from shake to actuation. All results are presented relative to the zero delay for each MDI group. N = 10 delivered dose were collected per product and delay time. DT delivery technology; FF formoterol fumarate; GFF glycopyrrolate/formoterol fumarate; GP glycopyrrolate; MDI metered dose inhaler. Error bars represent ± 1 standard deviation
DISCUSSION
Patients with COPD are typically treated with maintenance inhalers containing 30 days of drug treatment, which equates to 30 doses for a once-daily therapy or 60 doses for a twice-daily therapy. These products must be able to deliver the intended dose throughout the device life span. Each inhalation device type, whether MDI, DPI, SMI, or nebulizer, has its own set of formulation and development challenges with regards to achieving dose consistency (28,29), particularly for products that contain more than one drug, where drug delivery must be consistent between the mono and dual formulations (30,31). For suspension-based MDIs, one such challenge is poor physical and kinetic stability, which can result in drug delivery variability from one dose to the next (6,7,9).
In contrast to typical suspension-based MDI formulations, GFF MDI is formulated with co-suspension delivery technology that was designed to overcome challenges in MDI development and drug-delivery consistency. In this formulation, surface polarity of the phospholipid porous particles is similar to the surface polarity of the HFA, which reduces the tendency of porous particles to aggregate. Moreover, since there are a proportionally higher number of excipient particles than drug crystals, the drug crystals spontaneously associate with porous particles and form suspensions in propellant. Since the porous particles are less dense than the propellant, the porous particle/drug crystal ensemble results in a slowly creaming suspension that is easily dispersed with minimal input energy (8). Furthermore, the strong non-specific interaction between the porous particles and the drug crystals is stable in that drug crystals do not sediment when a sufficient amount of porous particles is available, regardless of whether a single drug or multiple drugs are formulated (8,30). As has been demonstrated with GFF MDI, the co-suspension delivery technology is effective at formulating FDC MDI products in which the performance of each individual drug is not impacted by the presence of the other drug or drugs (8).
In addition to addressing formulation challenges with MDI product development, co-suspension delivery technology also showed robust drug delivery under conditions of simulated patient use and handling errors in this study. GFF MDI demonstrated delivery of a consistent FPF for flow rates of 30–90 L/min, which may help to provide reliable dosing to patients with COPD with variable peak inhalation flow rates and volumes. These results are higher than, or comparable with, other MDIs, including an ultrafine solution-based formulation (23–27). The flow rate independence of other MDIs has previously been shown, but across a narrower range of flow rates (24,27,32). One commonly recognized user error with suspension-based MDIs is insufficient shaking prior to taking a dose (3) and, although not typically stated in patient instructions, imparting a delay between shaking and dose administration may also introduce dosing variability (14). For suspension-based MDIs, thorough shaking is often required to re-disperse and uniformly suspend the drug in propellant, as these drug formulations tend to flocculate and subsequently cream or sediment (9). Incorrect shaking or delays between shaking and actuation can result in significant deviations in both in vitro and in vivo drug delivery (14,33,34). GFF MDI with co-suspension delivery technology showed more consistent drug delivery when these simulated handling scenarios were applied in vitro compared with a drug crystal-only MDI. The drug crystal-only MDI used in this comparison had the same manufacturing process and container closure system as GFF MDI, but without any process or formulation optimization that would be expected for marketed MDI therapies. Similar to previous reports with other suspension-based MDIs that tend to settle, the drug crystal-only MDI displayed an increase in drug delivery when time between shaking and actuation was extended (14). Specifically, a recent evaluation of marketed MDI products showed that drug delivery was highly variable when delays from shake to actuation were applied, with delivered dose results exceeding 300% of the target LC dose for a 60-s delay between shake and actuation (14).
CONCLUSION
Co-suspension delivery technology provides a stable, uniform, and easily dispersed MDI suspension formulation when combined with one or multiple types of drug crystals. The formulation attributes of this technology enable pharmaceutical development of therapies that overcome many of the common drug-delivery consistency challenges associated with MDIs, including those that result from handling errors. GFF MDI, an FDC of two bronchodilators formulated using co-suspension delivery technology, displays consistent drug delivery and aerosol performance across a variety of standard test conditions and simulated handling errors. Furthermore, based on this evidence, the GFF MDI performance characteristics associated with co-suspension delivery technology are expected to translate into reliable dosing when used by patients in a real-world setting.
Change history
09 November 2017
This article was originally published Online First without open access. After publication it was discovered that the author had ordered open access during the production process. The incorrect license was assigned to this paper due to a technical error.
References
Ferkol T, Schraufnagel D. The global burden of respiratory disease. Ann Am Thorac Soc. 2014;11(3):404–6.
Chrystyn H, Price D. Not all asthma inhalers are the same: factors to consider when prescribing an inhaler. Prim Care Respir J. 2009;18(4):243–9.
Melani AS, Bonavia M, Cilenti V, Cinti C, Lodi M, Martucci P, et al. Inhaler mishandling remains common in real life and is associated with reduced disease control. Respir Med. 2011;105(6):930–8.
Molimard M, Raherison C, Lignot S, Depont F, Abouelfath A, Moore N. Assessment of handling of inhaler devices in real life: an observational study in 3811 patients in primary care. J Aerosol Med. 2003;16(3):249–54.
McDonald KJ, Martin GP. Transition to CFC-free metered dose inhalers—into the new millennium. Int J Pharm. 2000;201(1):89–107.
Myrdal PB, Sheth P, Stein SW. Advances in metered dose inhaler technology: formulation development. AAPS PharmSciTech. 2014;15(2):434–55.
Smyth HD. The influence of formulation variables on the performance of alternative propellant-driven metered dose inhalers. Adv Drug Deliv Rev. 2003;55(7):807–28.
Vehring R, Lechuga-Ballesteros D, Joshi V, Noga B, Dwivedi SK. Cosuspensions of microcrystals and engineered microparticles for uniform and efficient delivery of respiratory therapeutics from pressurized metered dose inhalers. Langmuir. 2012;28(42):15015–23.
Rogueda P. Novel hydrofluoroalkane suspension formulations for respiratory drug delivery. Expert Opin Drug Deliv. 2005;2(4):625–38.
Molimard M, Colthorpe P. Inhaler devices for chronic obstructive pulmonary disease: insights from patients and healthcare practitioners. J Aerosol Med Pulm Drug Deliv. 2015;28(3):219–28.
Bosnic-Anticevich SZ, Sinha H, So S, Reddel HK. Metered-dose inhaler technique: the effect of two educational interventions delivered in community pharmacy over time. J Asthma. 2010;47(3):251–6.
Crompton GK, Barnes PJ, Broeders M, Corrigan C, Corbetta L, Dekhuijzen R, et al. The need to improve inhalation technique in Europe: a report from the Aerosol Drug Management Improvement Team. Respir Med. 2006;100(9):1479–94.
Al-Showair RA, Tarsin WY, Assi KH, Pearson SB, Chrystyn H. Can all patients with COPD use the correct inhalation flow with all inhalers and does training help? Respir Med. 2007;101(11):2395–401.
Hatley RH, Parker J, Pritchard JN, von Hollen D. Variability in delivered dose from pressurized metered-dose inhaler formulations due to a delay between shake and fire. J Aerosol Med Pulm Drug Deliv. 2017;30(1):71–9.
Dellamary LA, Tarara TE, Smith DJ, Woelk CH, Adractas A, Costello ML, et al. Hollow porous particles in metered dose inhalers. Pharm Res. 2000;17(2):168–74.
AstraZeneca Pharmaceuticals LP. Bevespi Aerosphere Prescribing Information. 2016. http://www.accessdata.fda.gov/drugsatfda_docs/label/2016/208294s000lbl.pdf Accessed 27 May 2017.
Lechuga-Ballesteros D, Vehring R, Dwivedi SK. A new co-suspension MDI platform: scientific foundations of mono, dual and triple combination products. RDD Eur. 2011;1:101–12.
Ivey JW, Vehring R. The use of modeling in spray drying of emulsions and suspensions accelerates formulation and process development. Comput Chem Eng. 2010;34(7):1036–40.
Cummings H, Schultz RD, Speck JH, Joshi V, Lechuga-Ballesteros D, Flynn B, et al. Performance advantages of Pearl co-suspension formulation technology for manufacturing of metered-dose inhalers. RDD Eur. 2011;2:387–90.
Nimmo CJ, Chen DN, Martinusen SM, Ustad TL, Ostrow DN. Assessment of patient acceptance and inhalation technique of a pressurized aerosol inhaler and two breath-actuated devices. Ann Pharmacother. 1993;27(7–8):922–7.
Hesselink AE, Penninx BW, Wijnhoven HA, Kriegsman DM, van Eijk JT. Determinants of an incorrect inhalation technique in patients with asthma or COPD. Scand J Prim Health Care. 2001;19(4):255–60.
Janssens W, VandenBrande P, Hardeman E, De Langhe E, Philps T, Troosters T, et al. Inspiratory flow rates at different levels of resistance in elderly COPD patients. Eur Respir J. 2008;31(1):78–83.
Chambers F, Ludzik A. In vitro drug delivery performance of a new budesonide/formoterol pressurized metered-dose inhaler. J Aerosol Med Pulm Drug Deliv. 2009;22(2):113–20.
Johal B, Howald M, Fischer M, Marshall J, Venthoye G. Fine particle profile of fluticasone propionate/formoterol fumarate versus other combination products: the DIFFUSE Study. Comb Prod Ther. 2013;3(1):39–51.
Hatley RH, von Hollen D, Sandell D, Slator L. In vitro characterization of the OptiChamber Diamond valved holding chamber. J Aerosol Med Pulm Drug Deliv. 2014;27(Suppl 1):S24–36.
Leach CL, Davidson PJ, Boudreau RJ. Improved airway targeting with the CFC-free HFA-beclomethasone metered-dose inhaler compared with CFC-beclomethasone. Eur Respir J. 1998;12(6):1346.
De Maria R, Zagnoni I, Bodria A, Bonelli S, Alberi M, Lewis DA, et al. Foster®: a high-efficiency combination metered dose inhaler with consistent particle size distribution at alternative flow rates. Comb Prod Ther. 2014;4(1):1–5.
Newman SP. Principles of metered-dose inhaler design. Respir Care. 2005;50(9):1177–90.
Telko MJ, Hickey AJ. Dry powder inhaler formulation. Respir Care. 2005;50(9):1209–27.
Lechuga-Ballesteros D, Noga B, Vehring R, Cummings RH, Dwivedi SK. Novel cosuspension metered-dose inhalers for the combination therapy of chronic obstructive pulmonary disease and asthma. Future Med Chem. 2011;3(13):1703–18.
Traini D, Young PM, Rogueda P, Price R. In vitro investigation of drug particulates interactions and aerosol performance of pressurised metered dose inhalers. Pharm Res. 2007;24(1):125–35.
Ross DL, Schultz RK. Effect of inhalation flow rate on the dosing characteristics of dry powder inhaler (DPI) and metered dose inhaler (MDI) products. J Aerosol Med. 1996;9(2):215–26.
Everard ML, Devadason SG, Summers QA, Le Souef PN. Factors affecting total and “respirable” dose delivered by a salbutamol metered dose inhaler. Thorax. 1995;50(7):746–9.
Thorsson L, Edsbacker S. Lung deposition of budesonide from a pressurized metered-dose inhaler attached to a spacer. Eur Respir J. 1998;12(6):1340–5.
Battisti WP, Wager E, Baltzer L, Bridges D, Cairns A, Carswell CI, et al. Good publication practice for communicating company-sponsored medical research: GPP3. Ann Intern Med. 2015;163(6):461–64.
Acknowledgments
The authors would like to thank Sarvajna Dwivedi (Pearl Therapeutics Inc.) for his insight and scientific discussion that contributed to this manuscript. The authors also acknowledge the contributions from individuals within the Pearl Therapeutics Inc. functional areas that enabled this work, including MDI manufacturing (Jake Howland, Brian Foster, and Harris Cummings), Analytical Sciences (Mark Holland, James Jones, Travis Hayes, Ryan Carter, Ashley Stoker, Anne Crawford, Curt Alaspa, Rebecca Holden, Brandon Page, and Shyamala Ivatury), Quality Assurance (Rose Wilson and Shannon Cooley), and Product Development (Grace Li, Penny Tan, Lisa Williams, Aliyah Sheth, and Jill Sherwood), as well as the data reviewers (Joseph Zdanowicz, BJ Bryant, Chetna Purohit, and Wendy Luong).
Funding
This study was supported by Pearl Therapeutics Inc., a member of the AstraZeneca Group. Medical writing support was provided by Thomas Owens, PhD, of Complete Medical Communications, Macclesfield, UK, which was funded by AstraZeneca, Cambridge, UK in accordance with Good Publication Practice (GPP3) guidelines (35).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
All authors are employees of Pearl Therapeutics Inc., a member of the AstraZeneca Group.
Additional information
The original version of this article was revised: The copyright of the article has been changed to The Author(s) 2017 and the article is forthwith distributed under the terms of the Creative Commons Attribution.
A correction to this article is available online at https://doi.org/10.1208/s12249-017-0916-9.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Doty, A., Schroeder, J., Vang, K. et al. Drug Delivery from an Innovative LAMA/LABA Co-suspension Delivery Technology Fixed-Dose Combination MDI: Evidence of Consistency, Robustness, and Reliability. AAPS PharmSciTech 19, 837–844 (2018). https://doi.org/10.1208/s12249-017-0891-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1208/s12249-017-0891-1