Abstract
Background
Anticipated, internal, and enacted stigma are major barriers to tuberculosis (TB) care engagement and directly impact patient well-being. Unfortunately, targeted stigma interventions are lacking. We aimed to co-develop a person-centred stigma intervention with TB-affected community members and health workers in South Africa.
Methods
Using a community-based participatory research approach, we conducted ten group discussions with people diagnosed with TB (past or present), caregivers, and health workers (total n = 87) in Khayelitsha, Cape Town. Group discussions were facilitated by TB survivors. Discussion guides explored experiences and drivers of stigma and used human-centred design principles to co-develop solutions. Recordings were transcribed, coded, thematically analysed, and then further interpreted using the socio-ecological model and behaviour change wheel framework.
Results
Intervention components across socio-ecological levels shared common functions linked to effective behaviour change, namely education, training, enablement, persuasion, modelling, and environmental restructuring. At the individual level, participants recommended counselling to improve TB knowledge and provide ongoing support. TB survivors can guide messaging to nurture stigma resilience by highlighting that TB can affect anyone and is curable, and provide lived experiences of TB to decrease internal and anticipated stigma. At the interpersonal level, support clubs and family-centred counselling were suggested to dispel TB-related myths and foster support. At the institutional level, health worker stigma reduction training informed by TB survivor perspectives was recommended to decrease enacted stigma. Participants discussed how integration of TB/HIV care services may exacerbate TB/HIV intersectional stigma and ideas for restructured service delivery models were suggested. At the community level, participants recommended awareness-raising events led by TB survivors, including TB information in school curricula. At the policy level, solutions focused on reducing the visibility generated by a TB diagnosis and resultant stigma in health facilities and shifting tasks to community health workers.
Conclusions
Decreasing TB stigma requires a multi-level approach. Co-developing a person-centred intervention with affected communities is feasible and generates stigma intervention components that are directed and implementable. Such community-led multi-level intervention components should be prioritised by TB programs, including integrated TB/HIV care services.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Tuberculosis (TB) stigma is a major barrier to ending TB globally [1,2,3,4,5,6,7]. Drivers and facilitators of health-related stigma determine whether stigma “marking” of people or groups occurs [8], such as labelling of people with TB as likely having HIV co-infection in South Africa [9]. Once stigma is applied, it manifests as stigma experiences (lived realities) and practices (beliefs, attitudes, actions) which influence health and social outcomes [8]. Internal, anticipated, and enacted stigma (Table 1) delay TB diagnosis [1, 10,11,12] and compromise treatment adherence and completion [1, 13, 14]. Delayed diagnoses can increase disease severity and transmission, and poor adherence can lead to drug resistance, with impacts on individuals, communities, and health systems. Intersectional stigma (Table 1) can compound effects on health-seeking behaviour and care outcomes, as demonstrated by lower TB treatment adherence in people with TB and HIV co-infection who experience TB stigma [13]. TB stigma is associated with social isolation within families and communities [15], poor communication between health workers and patients [16], discrimination causing job or housing loss, with catastrophic and often long-term financial costs [17, 18], and poor psychological outcomes [15], including a higher likelihood of depression [19].
Despite global calls to address the wide-ranging impacts of TB stigma [21, 22], there are few TB stigma reduction interventions and a dearth of high-quality evidence on the design and implementation of such interventions. Two recent scoping reviews on TB stigma interventions reported major gaps in existing literature, including inconsistent application of stigma definitions, variable non-standardised measurement approaches, and incomplete reporting of intervention design and outcomes [23, 24]. Furthermore, the quality of stigma intervention studies was low, and none measured stigma as a primary outcome [23, 24]. Another review of health-related stigma interventions highlighted that stigma interventions have hitherto focused on a single socio-ecological level (most often that of the individual), which limits their impact given that stigma drivers and experiences are pervasive across levels including individual, interpersonal, institutional, community, and policy [25].
To develop effective TB stigma reduction interventions, participatory approaches that put TB-affected communities at the centre of the research process hold promise. Community-based participatory research (CBPR) involves partnerships with community representatives throughout the research process [26, 27]. This attempts to equalise power between researchers and the researched to promote cultural sensitivity, avoid potential harms, maximize the acceptability and reach of interventions, and advance health equity [28]. We have previously used CBPR in which peer research associates conducted community-based stigma assessments that demonstrated high levels of anticipated, internal, and enacted stigma that manifests across the cascade of care, and identified the lack of quality counselling as a major barrier to care engagement [29].
In intervention development, co-production is used as a strategy for meaningful collaboration with affected groups in all stages of the design process [30, 31]. By involving members of affected communities as co-researchers, co-production utilises locally situated, context-specific knowledge to develop more relevant and impactful interventions [32]. Addressing TB stigma requires an understanding of how stigma is experienced by people with TB, within their families, wider communities, and health systems. Co-production actively involves these stakeholders as partners, to understand their perspectives and work collaboratively to develop solutions [33]. Co-production may utilise human-centred design (HCD), a problem-solving approach that puts the needs of people (service-users) at the centre of the design process [34]. HCD has been shown to be feasible for intervention co-production with diverse populations in healthcare settings [35,36,37], such as efforts to make TB contact tracing more person-centred in Uganda [38]. Integrating HCD into CBPR studies can increase the likelihood of intervention effectiveness and adoption, expand its reach, and add innovation [39].
The aim of this study was to co-develop a counselling-based TB stigma intervention with people affected by TB and health workers in Cape Town, South Africa. We integrated CPBR and HCD principles to explore experiences of TB stigma in people with TB, their caregivers, and health workers and work collaboratively to co-design stigma intervention components. Preliminary data were presented at The Union Conference 2023 [40].
Methods
Study design and team
We conducted a qualitative study using a series of group discussions to co-develop a counselling-based TB stigma intervention, as part of a community-engaged research study: Use My Voice to EndTB [29]. The entire study — including the qualitative work — was co-led by a collaborative team of researchers, including TB survivors from TB Proof, a TB advocacy non-governmental organisation based in South Africa, and the Desmond Tutu TB Centre, Stellenbosch University.
Study setting and population
This study was conducted in Khayelitsha health sub-district, City of Cape Town Health District, Western Cape Province (WCP), South Africa. The incidence of TB in the City of Cape Town is 462 per 100,000 population [41]. Khayelitsha is a peri-urban, low-resourced township with a mix of formal and densely populated informal housing and represents one of the highest TB incidence areas in the WCP. We liaised with the TB nurse and the community health workers (CHWs) at Luvuyo, a Primary Health Clinic (PHC) serving the partner community, to identify people with experience of the local TB program by either accessing care, supporting persons with TB, or providing TB services. The community-based group consisted of (i) persons with TB (present or past) and (ii) caregivers of children or adults with TB. The facility-based group consisted of (i) TB counsellors, (ii) TB nurses, and (iii) CHWs. Individuals were purposively selected to maximize diversity in terms of age, gender, type of TB, and roles (for health workers).
Data collection processes
Between June 2022 and February 2023, we conducted ten discussions that were between 1 and 2 h in duration (average 90 min) with a total of 87 participants. These included community-based groups (4 sessions with persons with TB and caregivers), health worker groups (2 sessions with counsellors, nurses and CHWs), and subsequently combined community and health worker groups (4 sessions). Group size ranged from 5 to 16 (average 9 participants), with some participants taking part in multiple discussion sessions. Discussions were conducted in a venue next to the PHC or in the PHC staff room. Discussions were co-facilitated by a professional nurse researcher (NV (female)), a community-based researcher (LN (male)), and two TB survivors, who were trained as peer research associates (GM (male), PT (female)) [42], and have specific experience in qualitative research methods. Discussion guides (Additional File 1) were informed by the Health Stigma and Discrimination Framework [8] and pilot-tested by the team, with oversight provided by senior researchers (GH and RRN). The discussion guide was designed to cover: (1) experiences of stigma by domain (internal, anticipated, enacted, and intersectional); (2) identification of drivers of stigma and how they might impact care at different levels of the care cascade using card decks (described in Use of Human-Centred Design sub-section); (3) strategies to reduce stigma at different levels of the care cascade, and 4) potential role of counselling interventions to reduce stigma and key messages that should be delivered. All discussions were audio-recorded, notes were taken by PT and/or NV at all sessions, and summaries of the participants’ responses were written after each session by PT and NV. Discussions were conducted in either the local language isiXhosa and/or English in which all data collectors are bilingually fluent. Community-based group participants received reimbursement for their time and transport (R100 ≈ $5.25). Facility-based group participants did not receive reimbursements since the discussions took place in their work setting, and they were permitted to take time out of their working day to participate, thus no cost was incurred to them. Small snacks were provided to all discussion participants.
Use of human-centred design
HCD uses an iterative, solutions-based approach to problem-solving that starts with the target population’s needs and desires [43]. HCD has three core phases: inspiration, ideation, and implementation [34]. This study focused on the inspiration and ideation phases to identify intervention components for future implementation. In the inspiration phase, the aim is to define the problem and gather information to identify themes for potential solutions. Building on our prior work [29], in six of the ten discussions: four with persons with TB and caregivers, and two with health workers, we sought to understand stigma experiences and drivers, and the perceived need for stigma reduction interventions (inspiration). A card deck with visual images evoking examples of stigma manifesting at different steps of the TB care cascade, developed by TB Proof for a different community-based project, was used as a prompt for discussion. Participants were invited to select cards to stimulate conversation around scenarios and places where stigma occurs (Additional File 2). The ideation phase involves cycles of brainstorming to develop a prototype intervention. The last four of the ten discussions with combinations of persons with TB, caregivers, and health workers, were framed using “How might we…” questions, to explore how action could be taken to reduce TB stigma for specific groups, situations and settings. Such questions sought to elicit participants’ suggestions about intervention components and care delivery strategies that could reduce stigma experiences faced by people with TB (ideation).
Analysis
Discussion audio files were password-encrypted and were transcribed and translated into English by a qualitative researcher fluent in isiXhosa and English, who redacted any potentially identifying information, with iterative review by other research team members (NV, PT, GM). We used a thematic approach to analysis [44]. Specifically, after full immersion in the data from reading and discussing all the transcripts iteratively, two researchers (RRN and SEH) developed a coding scheme inductively with input from NV and GH (Additional File 3). This was applied systematically to the data using NVivo 1.7.1 (Lumivero, Colorado, USA), with alterations discussed between the researchers as new codes were iteratively developed. This was complemented by a deductive approach, using the socio-ecological model as a framework [45] to analyse our data [46]. We follow the Centers for Disease Control and Prevention adaptation of the socio-ecological model, which identifies the following levels within which factors can affect health: (1) individual, (2) interpersonal, (3) institutional, (4) community, and (5) policy [47]. Within each level, we considered how reported stigma experiences mapped to potential solutions to address stigma. Improving the design and implementation of interventions that require behaviour change requires an evidence-based approach to identify the core functions of interventions that are most likely to be effective in changing target behaviours [48]. We categorised proposed solutions to reduce stigma according to intervention functions in the behaviour change wheel framework [48], including education, enablement, and environmental restructuring (Table 2). We completed the COnsolidated criteria for REporting Qualitative research (COREQ) checklist (Additional File 4) [49].
Results
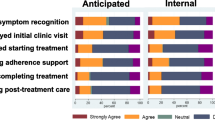
Analyses of the group discussions during the inspiration phase of the HCD approach identified stigma experiences as the central themes, categorised into internal, anticipated, enacted, or intersectional stigma (sub-themes). Analyses of the group discussions during the ideation phase of the HCD approach identified examples of and recommendations for stigma mitigation. Here, we present findings around (1) experiences of TB stigma and (2) proposed intervention components (relating to existing examples or hypothetical recommendations) at each level of the socio-ecological model, grouped according to intervention functions most likely to change target behaviours. Stigma experiences reported by participants and corresponding stigma intervention components proposed to address these are represented graphically in Fig. 1.
Individual level stigma experiences
People with TB reported experiencing internal and anticipated stigma due to fear and lack of knowledge. Some also reported feelings of self-blame, often due to a lack of understanding of how TB is transmitted, and in many cases related to HIV intersectional stigma:
I wonder what I did to deserve this. (community participant).
You have negative thoughts because you don’t have enough information. (community participant)
If you have TB you are HIV positive in the mind of a lot of people and you end up stigmatizing yourself. (community participant)
Individual level stigma intervention components
Education: optimise existing counselling provided to people with TB by health workers
People with TB emphasised gaps in existing counselling delivered by clinic-based health workers. Counselling, if provided, is focused on treatment adherence but does not adequately dispel knowledge gaps and misconceptions that can lead to anticipated and internal stigma, nor does it seek to foster psychosocial well-being. A nurse reflected that counselling should address feelings of shame that people with TB may experience, and that addressing these psychological effects of TB through counselling could also help health workers better understand and care for people with TB:
What I want to hear here at the clinic when I am counselled is that if you have TB, it is not your fault, TB can be found anywhere. (community participant)
Knowledge is power, the moment you know what you are doing you can stand anything. (health worker participant)
They [people with TB] can be counselled not only to understand what TB is but how they are dealing with shame from themselves of having TB […] I think counselling is very important on how I can deal with things that I come across [as a nurse]. (health worker participant)
To support both well-being and retention in care, people with TB emphasised that counselling must be regular and ongoing throughout care, from first contact with health services to post-TB cure:
I think when you are diagnosed with TB you must be given counselling regularly when you come to collect your medication. (community participant)
Enablement and persuasion: create platforms for TB survivor peer support with guided messaging
People with TB suggested insights from TB survivors could foster stigma resilience, support a sense of self-worth and reduce internal and anticipated stigma, particularly related to fears about death related to TB. They discussed the importance of positive messaging to convey that TB is curable, supported by examples of people who have overcome TB, using illustrative stories of survivors.
Explain to them clearly so that he can know that he is not the only one who is infected. There are a lot of people who get infected and there is a good chance to be healed, even though it’s not easy. Then you tell them that you are an example of that. (community participant)
You always hear that so-and-so had TB and passed away but you don’t hear about so-and-so who survived. (community participant)
Interpersonal level stigma experiences
People with TB reported feelings of isolation and instances of anticipated and enacted stigma from friends and family, resulting from fear and a lack of knowledge about TB.
Some of us don’t get support from our families […] they are scared to get infected because they don’t know about TB. (community participant)
I had a child who was infected with TB […] he stayed at home for 3 weeks, his friends didn’t want to play with him because they said he will infect them with TB. (community participant)
Interpersonal level stigma intervention components
Enablement and modelling: TB support groups to share experiences
Patients and health workers proposed TB support groups for patients to share experiences and support one another through treatment. They also suggested TB survivor peer navigators are well-placed to lead support groups: to answer questions, foster a sense of community, and act as role models.
We must meet as a group so that you can talk about how you feel [...] so that I can hear your journey and you can hear mine, so that I can be motivated to move forward. (community participant)
Another thing that has helped it was groups, clubs and support groups. You see even the one who didn’t understand the nurse or the counsellor they understand better when it’s being explained by someone next to them who are having the same experience. (health worker participant)
Education: family-centred counselling to improve knowledge, dispel misconceptions, and generate support
People with TB and caregivers emphasised the need for family-centred counselling. This creates an opportunity to provide support for caregivers and allows them to be educated about TB, dispelling myths and reducing stigma. Caregivers could then be better able to support their loved ones in ways that reduce anticipated and enacted stigma due to fear and a lack of awareness about TB.
I wish they can go even in the households so that everyone can be counselled so they can understand what is happening. (community participant)
Ask the family not to discriminate him/her because it is not the end of the world, he/she will make it. (community participant)
People with TB and caregivers suggested counselling could take place in homes and communities, outside the health facility, facilitated by CHWs. As such, family-centred counselling could facilitate the provision of patient-centred rather than clinic-centred care, by engaging those affected by TB (not limited to the patient) in a space where they may feel a greater sense of comfort and autonomy.
Counselling needs to be patient-centred not clinic-centred […] It’s based at the clinic, I as a patient I do not belong to the clinic, I belong to the community. If they can equip these CHWs and add social workers for the community not for the clinic, the stigma can be reduced because the information goes to the community. (community participant)
Institutional level stigma experiences
Participants reported instances of anticipated and enacted stigma whereby health workers had dehumanized people with TB, for example through the use of stigmatising language such as ‘defaulter’ for those who do not complete treatment.
I am the one who should be advocating for this patient […] but instead it’s me who makes the patient feel less of a human because the patient is infected with TB. (health worker participant)
I said to the doctor there is this name that you use called ‘default’. You do not understand why most TB patients fall under that name; it’s because taking this medication that you give us is not easy. (community participant)
Participants also reported how visibility in institutions such as clinics and schools could lead to anticipated and enacted TB stigma, and how this could deter attendance at these settings and thus lead to poor treatment adherence and non-completion.
This person was coming to the clinic, he would come and get the medication, but he didn’t want to be seen that he is taking TB medication, which made him change clinic and went to town, and that also made him be lost to follow up. (health worker participant)
Institutional level stigma intervention components
Training: health worker TB stigma training by TB survivors
People with TB proposed training for health workers, led by TB survivors, to improve their understanding of the experiences of people with TB and HIV/TB co-infection and avoid stigmatising language and practices. Health workers reflected on the need to better understand their patients’ lived experiences to foster empathy and compassion.
It is a must to listen […] we [health workers] think we know [TB/HIV] but we will never fully know besides what is written in the books. (health worker participant)
I want […] a relationship where there is humanity and support. (health worker participant)
Environmental restructuring: restructure service delivery models to decrease stigma and improve patient-centred TB care
People with TB and caregivers recommended restructured service delivery models to decrease anticipated and enacted stigma. This includes home-based care, particularly during the first few weeks of treatment, when people with TB are particularly vulnerable and struggle to remain engaged when feeling unwell. Specific suggestions for children with TB included after-school clinic appointments and the involvement of school nurses with TB care or to dispel stigma.
Patients could be met halfway and be given medication at home, because we are not all brave enough in these first two weeks. (community participant)
Children should be allowed to come after school [for TB care visits] to prevent questions as to why he didn’t come to school… Each school should also have school nurses to counter issues [that arise due to TB stigma]. (community participant)
Participants also highlighted the importance of individualised care, with service delivery models tailored to the patients’ needs.
Doctors see their patients and they know that they are not the same… if they could see during that first week that you are having difficulties, how about you get your medication at home for the whole journey? The doctors should look at the situation of the person because we might all be affected with TB but every situation is different. (community participant)
Community level stigma experiences
People with TB reported instances of anticipated and enacted stigma in the community, relating to experiences and fears of being gossiped about, labelled and ostracised.
To come here at [clinic] for me it was like it’s double the 32km; the way I was struggling and having difficulties made me attract the prying eyes. (community participant)
Participants mentioned that stigma in the community is mostly due to fear of contagion and lack of knowledge of TB, including gaps in understanding about how effective treatment decreases TB transmission risk or that TB and HIV do not always co-exist.
In the community most people fear that, if you are infected with TB, the moment you pass by, you are going to infect them. (community participant)
There are children who judged him at school, saying that he is going to infect us with TB. (community participant)
Community level stigma intervention components
Education and enablement: increase community awareness and knowledge through community educational forums, school curricula, and CHW outreach
People with TB and caregivers proposed solutions to increase awareness of TB in the community and thus reduce anticipated and enacted stigma. They highlighted the success of previous community events or imbizos to raise awareness of TB and HIV, with components such as theatre plays and football matches. They proposed such events should involve TB survivors who can act as role models, encouraging people with symptoms or risk to seek care and those with TB to disclose their diagnosis.
They brought a big truck to come and educate the community about TB and HIV, there were diverse people, young and old. (community participant)
When they put on these plays, they should be played by people who have experience […] for example someone will see [person with TB] whom they know and used to be sick in front of them. They will then think: I know this person and she is a strong woman so […] if she can stand up why can’t I do the same. (community participant)
People with TB and health workers also proposed incorporating TB into the school curriculum, along with wider outreach by CHWs.
TB is an airborne disease and everyone breathes the same air, if these children can be well educated […] to understand exactly what TB is and how does it infect you and to know that it is curable and how it is cured. (health worker participant)
When they do that door-to-door [education], they can reach everyone, and they are able to talk to my family properly about TB. (community participant)
Policy level factors
Environmental restructuring: consideration of how policies impact stigma and how restructured care delivery models including health worker task shifting may help
While policy-level components were not explicitly discussed as part of our group discussions, people with TB and health workers identified various issues that can perpetuate stigma in health facilities that would need to be addressed through policy change. They suggested reimagining clinic infrastructure to include removal of specific cards, folders, and/or uniforms that could identify care provision to TB patients, and universal mask-use in clinics.
If we can make it a golden rule that when you come to the health facility everyone must wear a mask because for only them [people with TB] to be asked to wear a mask it’s discriminating, because even someone who didn’t know you will know when seeing you wearing a mask that you are infected with TB and not everyone is comfortable with that being known. (community participant)
I am scared to be seen putting my card in that box, people already know that I have TB. (community participant)
Health workers mentioned high workloads and limited resources, both in terms of personnel and space, impacting time spent with patients, which has direct implications for the provision of quality counselling for people with TB.
You have about 50 patients that you have to see in 8 hours. (health worker participant)
The system has to hire more staff so that there is not only one nurse, the system must hire more counsellors or navigators, as people who will be mediators between the staff and the patient, so we understand where the biggest challenge is. (health worker participant)
Health workers also saw the value of home-based counselling with CHW outreach, although they acknowledged the possibility of households being marked by stigma depending on how this is done.
It would be nice for counselling to be done at home because others are comfortable in their space instead of being told that they should come to the clinic but it mustn’t be too formal where someone will be shocked to see CHWs coming to talk about TB but so that everyone who is at home can know about it. (community participant)
Discussion
To decrease TB stigma, action is required at multiple levels. Group discussions with people with TB, caregivers, and health workers revealed how stigma is experienced across the socio-ecological model. Guided by HCD principles, participants identified potential intervention components at each level. Intervention components across different levels were categorised into common functions from the behaviour change wheel framework [48], namely education, training, enablement, persuasion, modelling, and environmental restructuring, which can facilitate the efficient design of effective interventions. At the individual level, proposed improvements to existing counselling to address internal, anticipated, and intersectional stigma included involving TB survivors to help curate guided messaging. At the interpersonal level, participants suggested TB support groups and family-centred counselling could address anticipated and enacted stigma by dispelling myths around TB and fostering support. At the institutional level, participants recommended health worker stigma training informed by TB survivors and restructured service delivery models including home-based care. At the community level, approaches to improve knowledge and reduce misinformation included awareness-raising events led by TB survivors. At the policy level, solutions focused on reducing the visibility generated by a TB diagnosis and resultant stigma in facilities and shifting tasks to CHWs.
Existing interventions — all in the pilot stage — include some but not all of the intervention components proposed by our participants. Prior studies have focused on the individual and interpersonal levels, including TB support groups or clubs [50,51,52], home visits [52, 53], and education for patients/caregivers [54]. TB support groups/clubs have been predominantly facilitated by health workers, such as psychiatrists, nurses, and CHWs [50,51,52]. However, our study participants highlight the potential benefit of involving TB survivors in leading such groups, as well as creating platforms for TB survivors to support people with TB, and optimising existing counselling by health workers with guided messaging around TB that is informed by real-life experiences. Studies involving TB patients’ families provide models for how family-centred counselling could be carried out via home visits [52, 53] and educational tools such as videos [54], which our partner advocacy organisation TB Proof has also used to decrease TB stigma [55, 56]. At the institutional level, health worker training interventions including participatory workshops and visual messaging may reduce TB stigma amongst health workers [57,58,59]. Examples of community-volunteer led education in the form of health talks in community spaces [60] align with strategies proposed by our participants including engagements through school curricula and strengthening CHW outreach.
Proposed novel institutional and policy level interventions include restructuring care delivery models to become more patient-centred, such as differentiated service delivery (DSD) models for HIV [61] or home-based care delivery [62], with the aims of people with TB being less visible in clinics, and health worker task shifting to facilitate provision of stigma-informed care. Such interventions require organisational-level change, creating challenges for implementation, which is perhaps why no existing TB stigma reduction interventions have used such approaches. In contrast, psychological support provided through nurse-led home-based care for people with HIV/AIDS improved stigma scores [63]. Other structural changes to reduce stigma in healthcare settings employed in HIV and mental health services [64] include pharmacists in Ghana designing service delivery changes related to where people with HIV collect their medications [65]. Examples of lay health workers delivering psychological interventions [66] provide insights for counselling-based stigma interventions delivered by CHWs and/or TB survivors [67]. While existing studies and practices utilising lay health workers or disease survivors often rely on volunteerism [68], we emphasise that multi-level interventions that seek to increase equity must recognise contributions of CHWs or TB survivors by formalising their role through payment and provision of appropriate training and support.
Notably, existing TB stigma reduction interventions are typically targeted at one or possibly two levels. This highlights a tension whereby, given limited resources, trade-offs are made between interventions at different levels of the socio-ecological model. Our participants also identified this friction, with strategies targeting individuals (individuals experience stigma, therefore interventions should seek to foster resilience) often pitted against those targeting the wider family, clinic or, community (interventions should either change attitudes or reduce visibility to prevent stigma from occurring at all). For example, when trying to address hesitation about TB disclosure, some participants argued for structural changes to reduce visibility (removing identifying features in clinics such as cards/uniforms, facilitating home-based care), and others advocated that people with TB should be empowered to freely disclose their TB status (counselling and education to foster resilience). While single-level interventions may seem more feasible from a funding or policy perspective, a synergistic multi-level approach [69] that seeks to foster individual resilience amongst people with TB while strengthening institutional and/or community efforts to address stigma is more likely to be effective.
The impact of intersectional TB-HIV stigma across all levels of the socio-ecological model, also identified in other studies [9, 70], was often emphasised by participants. The move towards greater TB-HIV care integration is aligned with the aims of DSD for HIV treatment [61, 71]. While studies indicate the effectiveness of DSD for TB-HIV when considering indicators such as treatment success [72], our findings — in line with other studies [73] — suggest this could exacerbate intersectional TB-HIV stigma. This has implications for calls to integrate TB with other care services such as diabetes [74, 75] or mental health [76,77,78], highlighting the need to evaluate the risk of such service delivery models inadvertently exacerbating TB stigma. Other tensions related to optimal service delivery provision included the challenges of one-size-fits-all programmatic approaches. While some patients may appreciate support such as home medication delivery and ongoing counselling throughout treatment, others may find this unhelpful and even condescending. There is a desire for individualised care, tailored to the needs of each person with TB and fostered through empathetic relationships with health workers. Yet resource constraints common in high TB incidence settings were apparent in our data, with health workers reporting how high workloads impact their ability to deliver high-quality care. Most literature on individualised care focuses on treatment of chronic conditions in high-income countries [79], with proposals for tailored TB care largely limited to individualised treatment duration [80, 81]. Implementation research can identify how best to target and deliver individualised care for TB, for example through risk factor screening to identify vulnerable individuals [82].
Limitations of the study include conducting discussions at only one clinic in Khayelitsha, Cape Town, which reduces generalisability of the findings, due to structural and cultural differences between settings and communities [83]. Nonetheless, this in-depth focus on a single community is the most appropriate for co-design projects, to form a long-term iterative collaboration with affected groups in a specific community and design an intervention tailored to their specific needs [84]. Although the use of peer research associates raises the possibility that their lived experience may influence discussions, their involvement improved rapport with participants, understanding of local references, and contextualisation of their narratives [42]. We thus sought to analyse findings reflexively, bearing in mind the positionality of facilitators and researchers [85]. Key strengths include the use of HCD and CBPR. Using CBPR, we included survivors, caregivers, and health workers in separate and combined groups, we were able to identify differing views and points of synergy. Using HCD enabled us to translate stigma experiences and service provision gaps into actionable intervention components.
Conclusions
Decreasing TB stigma requires a multi-level approach. Co-developing a person-centred intervention with affected communities is feasible and can generate directed, tailored stigma intervention components. By mapping actionable intervention components proposed by participants at each socio-ecological level to intervention functions, including education, training, enablement, persuasion, modelling, and environmental restructuring, we can maximize the likelihood of effecting behaviour change. TB survivors can play a critical role as peer research associates to both inform stigma intervention design and to help galvanise policy change to decrease factors driving stigma.
Availability of data and materials
Data is provided within the manuscript and we have now uploaded a data sharing file which is publicly available through the Harvard Dataverse: Nathavitharana, Ruvandhi, 2024, "UseMyVoice to EndTB stigma intervention co-development focus group discussion data", https://doi.org/10.7910/DVN/1LNKYU, Harvard Dataverse, V1, which we have also cited in the Methods.
References
Courtwright A, Turner AN. Tuberculosis and stigmatization: pathways and interventions. Public Health Rep. 2010;125(4_suppl):34–42.
Daftary A, Mitchell EMH, Reid MJA, Fekadu E, Goosby E. To end TB, first-ever high-level meeting on tuberculosis must address stigma. Am J Trop Med Hyg. 2018;99(5):1114–6.
Xu M, Markström U, Lyu J, Xu L. Survey on tuberculosis patients in rural areas in China: tracing the role of stigma in psychological distress. Int J Environ Res Public Health. 2017;14(10):1171.
Cremers AL, Janssen S, Huson MAM, Bikene G, Bélard S, Gerrets RPM, et al. Perceptions, health care seeking behaviour and implementation of a tuberculosis control programme in Lambaréné. Gabon Public Health Action. 2013;3(4):328–32.
Teo AKJ, Singh SR, Prem K, Hsu LY, Yi S. Duration and determinants of delayed tuberculosis diagnosis and treatment in high-burden countries: a mixed-methods systematic review and meta-analysis. Respir Res. 2021;22(1):251.
Craig GM, Daftary A, Engel N, O’Driscoll S, Ioannaki A. Tuberculosis stigma as a social determinant of health: a systematic mapping review of research in low incidence countries. Int J Infect Dis. 2017;56:90–100.
Chen X, Du L, Wu R, Xu J, Ji H, Zhang Y, et al. Tuberculosis-related stigma and its determinants in Dalian, Northeast China: a cross-sectional study. BMC Public Health. 2021;21(1):6.
Stangl AL, Earnshaw VA, Logie CH, van Brakel W, Simbayi CL, Barré I, et al. The health stigma and discrimination framework: a global, crosscutting framework to inform research, intervention development, and policy on health-related stigmas. BMC Med. 2019;17(1):31.
Daftary A. HIV and tuberculosis: the construction and management of double stigma. Soc Sci Med. 2012;74(10):1512–9.
Paramasivam S, Thomas B, Chandran P, Thayyil J, George B, Sivakumar C. Diagnostic delay and associated factors among patients with pulmonary tuberculosis in Kerala. J Family Med Prim Care. 2017;6(3):643.
Chakrabartty A, Basu P, Ali KM, Sarkar AK, Ghosh D. Tuberculosis related stigma and its effect on the delay for sputum examination under the revised national tuberculosis control program in India. Indian J Tuberc. 2018;65(2):145–51.
Kurspahić-Mujčić A, Hasanović A, Sivić S. Tuberculosis related stigma and delay in seeking care after the onset of symptoms associated with tuberculosis. Med Glas (Zenica). 2013;10(2):272–7.
Kipp AM, Pungrassami P, Stewart PW, Chongsuvivatwong V, Strauss RP, Van Rie A. Study of tuberculosis and AIDS stigma as barriers to tuberculosis treatment adherence using validated stigma scales. Int J Tuberc Lung Dis. 2011;15(11):1540–6.
Kolte IV, Pereira L, Benites A, De Sousa IMC, Basta PC. The contribution of stigma to the transmission and treatment of tuberculosis in a hyperendemic indigenous population in Brazil. PLoS One. 2020;15(12):e0243988.
Mbuthia GW, Nyamogoba HDN, Chiang SS, McGarvey ST. Burden of stigma among tuberculosis patients in a pastoralist community in Kenya: a mixed methods study. PLoS One. 2020;15(10):e0240457.
Yin X, Yan S, Tong Y, Peng X, Yang T, Lu Z, et al. Status of tuberculosis-related stigma and associated factors: a cross-sectional study in central China. Tropical Med Int Health. 2018;23(2):199–205.
Ghazy RM, El Saeh HM, Abdulaziz S, Hammouda EA, Elzorkany AM, Khidr H, et al. A systematic review and meta-analysis of the catastrophic costs incurred by tuberculosis patients. Sci Rep. 2022;12(1):558.
Meghji J, Gregorius S, Madan J, Chitimbe F, Thomson R, Rylance J, et al. The long term effect of pulmonary tuberculosis on income and employment in a low income, urban setting. Thorax. 2021;76(4):387–95.
Duko B, Gebeyehu A, Ayano G. Prevalence and correlates of depression and anxiety among patients with tuberculosis at WolaitaSodo University Hospital and Sodo Health Center, WolaitaSodo, South Ethiopia, Cross sectional study. BMC Psychiatry. 2015;15(1):214.
International union against tuberculosis and lung disease. Pyschosocial counselling and treatment adherence support for people with tuberculosis. 2021.
Macintyre K, Bakker MI, Bergson S, Bhavaraju R, Bond V, Chikovore J, et al. Defining the research agenda to measure and reduce tuberculosis stigmas. Int J Tuberc Lung Dis. 2017;21(11):87–96.
Jaramillo E, Sahu S, Van Weezenbeek C. Ending TB-related stigma and discrimination. Int J Tuberc Lung Dis. 2017;21(11):2–3.
Nuttall C, Fuady A, Nuttall H, Dixit K, Mansyur M, Wingfield T. Interventions pathways to reduce tuberculosis-related stigma: a literature review and conceptual framework. Infect Dis Poverty. 2022;11(1):101.
Foster I, Galloway M, Human W, Anthony M, Myburgh H, Vanqa N, et al. Analysing interventions designed to reduce tuberculosis-related stigma: a scoping review. PLOS Global Public Health. 2022;2(10):e0000989.
Heijnders M, Van Der Meij S. The fight against stigma: an overview of stigma-reduction strategies and interventions. Psychol Health Med. 2006;11(3):353–63.
Israel BA, Schulz AJ, Parker EA, Becker AB. Review of community-based research: assessing partnership approaches to improve public health. Annu Rev Public Health. 1998;19:173–202.
Pellecchia M, Mandell DS, Nuske HJ, Azad G, Benjamin Wolk C, Maddox BB, et al. Community-academic partnerships in implementation research. J Community Psychol. 2018;46(7):941–52.
Wallerstein N, Oetzel JG, Sanchez-Youngman S, Boursaw B, Dickson E, Kastelic S, et al. Engage for equity: a long-term study of community-based participatory research and community-engaged research practices and outcomes. Health Educ Behav. 2020;47(3):380–90.
Foster I, Biewer A, Vanqa N, Makanda G, Tisile P, Hayward SE, et al. “This is an illness. No one is supposed to be treated badly”: community-based stigma assessments in South Africa to inform tuberculosis stigma intervention design. BMC Global and Public Health. 2024;2(1):41.
Hawkins J, Madden K, Fletcher A, Midgley L, Grant A, Cox G, et al. Development of a framework for the co-production and prototyping of public health interventions. BMC Public Health. 2017;17(1):689.
Filipe A, Renedo A, Marston C. The co-production of what? Knowledge, values, and social relations in health care. PLoS Biol. 2017;15(5):e2001403.
Balazs CL, Morello-Frosch R. The three Rs: how community-based participatory research strengthens the rigor, relevance, and reach of science. Environ Justice. 2013;6(1):9–16.
Batalden M, Batalden P, Margolis P, Seid M, Armstrong G, Opipari-Arrigan L, et al. Coproduction of healthcare service. BMJ Qual Saf. 2016;25(7):509.
Fischer M, Safaeinili N, Haverfield MC, Brown-Johnson CG, Zionts D, Zulman DM. Approach to human-centered, evidence-driven adaptive design (AHEAD) for health care interventions: a proposed framework. J Gen Intern Med. 2021;36(4):1041–8.
Altman M, Huang TTK, Breland JY. Design thinking in health care. Prev Chronic Dis. 2018;15:180128.
Bazzano AN, Martin J. Designing public health: synergy and discord. Des J. 2017;20(6):735–54.
Smith PJ, Joseph Davey DL, Schmucker L, Bruns C, Bekker LG, Medina-Marino A, et al. Participatory prototyping of a tailored undetectable equals untransmittable message to increase HIV testing among men in Western Cape. South Africa AIDS Patient Care STDS. 2021;35(11):428–34.
Liu C, Lee JH, Gupta AJ, Tucker A, Larkin C, Turimumahoro P, et al. Cost-effectiveness analysis of human-centred design for global health interventions: a quantitative framework. BMJ Glob Health. 2022;7(3):e007912.
Chen E, Leos C, Kowitt SD, Moracco KE. Enhancing community-based participatory research through human-centered design strategies. Health Promot Pract. 2019;21(1):37–48.
Hayward SE, Vanqa N, Makanda G, Tisile P, Ngwatyu L, Mcinziba A, et al. Addressing TB/HIV intersectional stigma: co‐developing a multi‐level person‐centred stigma reduction intervention with affected communities in South Africa. Abstract LB01–103–15. Paris, France: Oral presentation at the Union World Conference on Lung Health; 2023.
Microbiologically confirmed pulmonary TB-centre for tuberculosis. National Health Laboratory Service M&E Online Dashboards. 2021. Available from: https://mstrweb.nicd.ac.za/Microstrategy/asp/Main.aspx. Accessed 19 Jan 2024.
Kaida A, Carter A, Nicholson V, Lemay J, O’Brien N, Greene S, et al. Hiring, training, and supporting peer research associates: operationalizing community-based research principles within epidemiological studies by, with, and for women living with HIV. Harm Reduct J. 2019;16(1):47.
Hasso Plattner Institute of Design at Stanford University. An introduction to design thinking: Process guide. 2010. Available from: https://web.stanford.edu/~mshanks/MichaelShanks/files/509554.pdf.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
Sallis JF, Owen N, Fisher EB. Ecological models of health behavior. In: Glanz K, Rimer BK, Viswanath K, editors. Health Behaviour and Health Education: Theory, Research, and Practice. 4th ed. San Francisco, CA, USA: Jossey-Bass; 2008. p. 465–485.
Nathavitharana R. UseMyVoice to EndTB stigma intervention co-development focus group discussion data. https://doi.org/10.7910/DVN/1LNKYU. Harvard Dataverse. V1. 2024.
Kilanowski JF. Breadth of the socio-ecological model. J Agromedicine. 2017;22(4):295–7.
Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6(1):42.
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–57.
Acha J, Sweetland A, Guerra D, Chalco K, Castillo H, Palacios E. Psychosocial support groups for patients with multidrug-resistant tuberculosis: five years of experience. Glob Public Health. 2007;2(4):404–17.
Demissie M, Getahun H, Lindtjørn B. Community tuberculosis care through “TB clubs” in rural North Ethiopia. Soc Sci Med. 2003;56(10):2009–18.
Macq J, Solis A, Martinez G, Martiny P. Tackling tuberculosis patients’ internalized social stigma through patient centred care: an intervention study in rural Nicaragua. BMC Public Health. 2008;8(1):154.
Bond V, Floyd S, Fenty J, Schaap A, Godfrey-Faussett P, Claassens M, et al. Secondary analysis of tuberculosis stigma data from a cluster randomised trial in Zambia and South Africa (ZAMSTAR). Int J Tuberc Lung Dis. 2017;21(11):49–59.
Wilson JW, Ramos JG, Castillo F, Castellanos EF, Escalante P. Tuberculosis patient and family education through videography in El Salvador. J Clin Tuberc Other Mycobact Dis. 2016;4:14–20.
TB Proof. TB Proof Community TB Stigma video: YouTube; 2023. Available from: https://www.youtube.com/watch?v=2GwyzFjORbI.
TB Proof. TB Proof Healthcare Worker TB Stigma: YouTube; 2023. Available from: https://www.youtube.com/watch?v=6ctcaYVq46g.
Yassi A, Mabhele S, Wilcox ES, Tsang VWL, Lockhart K. An embodied exercise to address HIV- and tuberculosisrelated stigma of healthcare workers in Southern Africa. J Appl Arts Health. 2019;10(1):73–85.
Siegel J, Yassi A, Rau A, Buxton JA, Wouters E, Engelbrecht MC, et al. Workplace interventions to reduce HIV and TB stigma among health care workers-where do we go from here? Glob Public Health. 2015;10(8):995–1007.
Wu PS, Chou P, Chang NT, Sun WJ, Kuo HS. Assessment of changes in knowledge and stigmatization following tuberculosis training workshops in taiwan. J Formos Med Assoc. 2009;108(5):377–85.
Balogun M, Sekoni A, Meloni ST, Odukoya O, Onajole A, Longe-Peters O, et al. Trained community volunteers improve tuberculosis knowledge and attitudes among adults in a periurban community in southwest Nigeria. Am J Trop Med Hyg. 2015;92(3):625–32.
Roy M, Bolton Moore C, Sikazwe I, Holmes CB. A review of differentiated service delivery for HIV treatment: effectiveness, mechanisms, targeting, and scale. Curr HIV/AIDS Rep. 2019;16(4):324–34.
John JR, Jani H, Peters K, Agho K, Tannous WK. The effectiveness of patient-centred medical home-based models of care versus standard primary care in chronic disease management: a systematic review and meta-analysis of randomised and non-randomised controlled trials. Int J Environ Res Public Health. 2020;17(18):6886.
Wood EM, Zani B, Esterhuizen TM, Young T. Nurse led home-based care for people with HIV/AIDS. BMC Health Serv Res. 2018;18(1):219.
Nyblade L, Stockton MA, Giger K, Bond V, Ekstrand ML, Lean RM, et al. Stigma in health facilities: why it matters and how we can change it. BMC Med. 2019;17(1):25.
Health Policy Plus. Webinar: how to engage with health facilities to reduce HIV-related stigma and move closer to test and treat goals. Washington, DC: Health Policy Plus; 2018. http://www.healthpolicyplus.com/ns/pubs/7187-7333_SDWebinar.pdf.
Shahmalak U, Blakemore A, Waheed MW, Waheed W. The experiences of lay health workers trained in task-shifting psychological interventions: a qualitative systematic review. Int J Ment Heal Syst. 2019;13(1):64.
Ayakaka I, Armstrong-Hough M, Hannaford A, Ggita JM, Turimumahoro P, Katamba A, et al. Perceptions, preferences, and experiences of tuberculosis education and counselling among patients and providers in Kampala, Uganda: a qualitative study. Glob Public Health. 2022;17(11):2911–28.
Budde H, Williams GA, Winkelmann J, Pfirter L, Maier CB. The role of patient navigators in ambulatory care: overview of systematic reviews. BMC Health Serv Res. 2021;21(1):1166.
Heijnders M, Van Der Meij S. The fight against stigma: an overview of stigma-reduction strategies and interventions. Psychol Health Med. 2006;11(3):353–63.
Wouters E, Sommerland N, Masquillier C, Rau A, Engelbrecht M, Van Rensburg AJ, et al. Unpacking the dynamics of double stigma: how the HIV-TB co-epidemic alters TB stigma and its management among healthcare workers. BMC Infect Dis. 2020;20(1):106.
World Health Organization. WHO Guidelines Approved by the Guidelines Review Committee. Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection: recommendations for a public health approach. Geneva: World Health Organization; 2016.
Tran CH, Moore BK, Pathmanathan I, Lungu P, Shah NS, Oboho I, et al. Tuberculosis treatment within differentiated service delivery models in global HIV/TB programming. J Int AIDS Soc. 2021;24 Suppl 6(Suppl 6):e25809.
Daftary A, Padayatchi N. Social constraints to TB/HIV healthcare: accounts from coinfected patients in South Africa. AIDS Care. 2012;24(12):1480–6.
Nyirenda JLZ, Bockey A, Wagner D, Lange B. Effect of tuberculosis (TB) and diabetes mellitus (DM) integrated healthcare on bidirectional screening and treatment outcomes among TB patients and people living with DM in developing countries: a systematic review. Pathog Glob Health. 2023;117(1):36–51.
Riza AL, Pearson F, Ugarte-Gil C, Alisjahbana B, van de Vijver S, Panduru NM, et al. Clinical management of concurrent diabetes and tuberculosis and the implications for patient services. Lancet Diabetes Endocrinol. 2014;2(9):740–53.
Galea JT, Monedero-Recuero I, Sweetland AC. Beyond screening: a call for the routine integration of mental health care with tuberculosis treatment. Public Health Action. 2019;9(1):2.
Sweetland AC, Galea J, Shin SS, Driver C, Dlodlo RA, Karpati A, et al. Integrating tuberculosis and mental health services: global receptivity of national tuberculosis program directors. IJTLD. 2019;23(5):600–5.
Sweetland AC, Jaramillo E, Wainberg ML, Chowdhary N, Oquendo MA, Medina-Marino A, et al. Tuberculosis: an opportunity to integrate mental health services in primary care in low-resource settings. Lancet Psychiatry. 2018;5(12):952–4.
Godfrey M, Young J, Shannon R, Skingley A, Woolley R, Arrojo F, et al. Chapter 4, Person-centred care: meaning and practice. The person, interactions and environment programme to improve care of people with dementia in hospital: a multisite study. Health Services and Delivery Research, No. 6.23. Southampton: NIHR Journals Library; 2018.
Adjobimey M, Behr MA, Menzies D. Individualized treatment duration in tuberculosis treatment: precision versus simplicity. Am J Respir Crit Care Med. 2021;204(9):1013–4.
Dookie N, Padayatchi N, Lessells RJ, Naicker CL, Chotoo S, Naidoo K. Individualized treatment of multidrug-resistant tuberculosis using whole-genome sequencing and expanded drug-susceptibility testing. Clin Infect Dis. 2020;71(11):2981–5.
Washington R, Potty RS, Rajesham A, Seenappa T, Singarajipura A, Swamickan R, et al. Is a differentiated care model needed for patients with TB? A cohort analysis of risk factors contributing to unfavourable outcomes among TB patients in two states in South India. BMC Public Health. 2020;20(1):1158.
Bresenham D, Kipp AM, Medina-Marino A. Quantification and correlates of tuberculosis stigma along the tuberculosis testing and treatment cascades in South Africa: a cross-sectional study. Infect. 2020;9(1):145.
Zamenopoulos T, Alexiou K. Co-design as collaborative research. In: Facer K, Dunleavy K, editors. Connected communities foundation series. Bristol: University of Bristol/AHRC Connected Communities Programme; 2018.
Braun V, Clarke V. Reflecting on reflexive thematic analysis. Qual Res Sport Exerc Health. 2019;11(4):589–97.
Acknowledgements
We express our sincere gratitude to the patients, TB survivors, and family members who participated in this study, and the staff and CHWs at Luvuyo Clinic, Khayelitsha, Western Cape. We also thank Caoimhe Smyth, Ricarda Steele, James Malar, and Viorel Soltan from the Stop TB Partnership for their guidance and support.
Funding
This work was funded by a Stop TB Partnership Challenge Facility for Civil Society Round 10 grant, awarded to TB Proof. RRN is supported by a National Institutes of Health Career Development Award (NIAID K23 AI132648-05) and New Innovator Award (NIAID DP2-AI176896), and an American Society of Tropical Medicine and Hygiene Burroughs Wellcome Fellowship. GH received financial assistance from the European Union (Grant no. DCI-PANAF/2020/420–028), through the African Research Initiative for Scientific Excellence (ARISE), pilot programme. ARISE is implemented by the African Academy of Sciences with support from the European Commission and the African Union Commission. SEH is supported by a UK Medical Research Council PhD studentship (MR/N013638/1). AMM is supported by the US National Institutes of Health (NIAID R01AI150485; NIAID R21AI148852; R34HL170819). The contents of this document are the sole responsibility of the author(s) and can under no circumstances be regarded as reflecting the position of the European Union, the US National Institutes of Health, the African Academy of Sciences, or the African Union Commission.
The funders had no role in the conceptualization, design, data collection, analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
SEH, NV, and RRN analyzed the findings, wrote the main manuscript, and prepared the tables. NV, GM, PT, and LN led data collection. Project supervision was undertaken by IS, MG, LV, GH, and RRN. All authors reviewed and provided critical input on the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Health Research Ethics Committee of Stellenbosch University (N20/10/113), the City of Cape Town Health Directorate, and the Western Cape Department of Health (NHRD ref: WC_Project ID 9804). All participants provided written informed consent. The research conformed to the principles of the Helsinki Declaration.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Hayward, S.E., Vanqa, N., Makanda, G. et al. “As a patient I do not belong to the clinic, I belong to the community”: co-developing multi-level, person-centred tuberculosis stigma interventions in Cape Town, South Africa. BMC Global Public Health 2, 55 (2024). https://doi.org/10.1186/s44263-024-00084-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s44263-024-00084-z