Abstract
Background
In Ecuador, cervical cancer is the third most common cancer among women and the second most common cause of cancer-related death in women. Although HPV represents a serious public health problem worldwide, the information about its prevalence and genotypes in remote communities of Ecuador is limited. The aim of this study was to determine the distribution of HPV genotypes among ethnic minority women from two remote communities of the northwestern region of Ecuador: Afro-Ecuadorians and Chachis (Amerindian group).
Methods
We included 291 women who responded to a short survey and were screened for HPV by the amplification of the L1 gene and a nested multiplex PCR to detect 14 high risk (HR) genotypes. A survey collected information on ethnicity, age, community access, and sexual and gynecological history. We identified risk factors associated with HPV infection and co-infection using multivariate logistic regression to calculate odds ratio (OR) and Wald 95% confidence intervals (CI).
Results
Overall, HPV prevalence in the study cohort was 56%, and the five most common HR-HPV genotypes were HPV-58, -16, -68, -39, and -43; however, the distribution of HPV genotypes varied according to ethnicity. We identified lineage A (European variant) for HPV-16 and sublineage A2 for HPV-58 in both ethnic groups. Adjusting for ethnicity, age, community access, and number of sexual partners, we found that Afro-Ecuadorian women were less likely to have an HPV infection than Chachi women (OR: 0.49, 95% CI: 0.25, 0.96), and that participants in communities only accessible by river had 64% less chances of an HPV infection when compared to women in communities accessible by road (OR: 0.36, 95% CI: 0.19, 0.71), and women with 2 to 3 sexual partners had 2.47 times the odds of HPV infection than participants with 0–1 partners (OR: 2.47, 95% CI: 1.32, 4.6). Similar associations were observed with prevalence of co-infection.
Conclusions
This study provides baseline knowledge regarding the prevalence and distribution of HPV genotypes in ethnic groups of the northwestern coastal Ecuador and essential information for the implementation of appropriate HPV testing and vaccination program to prevent cervical cancer.
Similar content being viewed by others
Background
Cervical cancer is the fourth most frequently diagnosed cancer and cause of death among women in low- and middle-income countries, with an estimated 604,127 new cases and 341,831 deaths in 2020 [1]. In Ecuador, cervical cancer is the third cause of cancer and the second most common cause of death among young women of ages 15 to 44 [2]. Annually, an estimated of 1534 new cervical cancer cases and 813 cervical cancer deaths occur in the country [3]. The persistent infection with oncogenic genotypes of human papillomavirus (HPV), named high-risk (HR) genotypes, is the most important cause of cervical cancer [2, 4].
The six most common HR-HPV genotypes worldwide are HPV-16, HPV-18, HPV-45, HPV-52, HPV-31, and HPV-58 [5,6,7]. However, the distribution of HPV genotypes and its prevalence vary broadly throughout the world [4, 8]. In many regions, HPV-16 and -18 are the most prevalent oncogenic genotypes, responsible for about 70% of all cervical cancer [8,9,10]. In East Asia, some parts of Europe, Latin America, and Africa, HPV-58, HPV-52, HPV-31, and HPV-45 are among the most common genotypes [5, 7, 10, 11].
HPV genotypes can be further classified into lineages and sublineages (variants). These variants show distinct association with persistence, high viral load, progression to precancer, and cancer, suggesting that each lineage has a distinct evolutionary history [12,13,14]. It has also been suggested that host genetic factors (human leukocyte antigen, HLA, haplotypes) may influence the progression to cancer of some HPV variants [15]. For instance, a study conducted by Mejia et al. [16] in Ecuadorian women showed that HPV-16 from the European lineage was the most common type. The European lineage is considered one of the least carcinogenic.
Women from rural communities in low- and middle-income countries are more vulnerable to develop cervical cancer mainly due to limited access to prevention and treatment. Studies have revealed a disproportionate burden of HPV-related diseases in these populations due to limited access to healthcare, cultural barriers, and socioeconomic disparities [17, 18]. A few studies have estimated HPV prevalence, genotype distribution, and risk factors in rural or indigenous populations in South American countries [19,20,21,22]. Namely, a recent study in the southern highlands of Ecuador concluded that indigenous women had a higher prevalence of HPV infection compared to mestizos (a person of mixed race, especially one having Spanish and indigenous descent) [23]. In Ecuador, recent studies focused on HPV and its clinical manifestations in indigenous populations of the Andean and high Andean region [24, 25] but have not included communities in remote coastal areas. The aim of our study was to determine the main HPV genotypes and oncogenic variants among women from rural communities in the northwestern coastal region of Ecuador and identify risk factors associated with HPV infection in this population.
Methods
Study design and participant selection
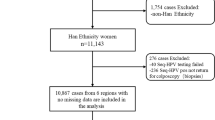
We carried out a cross-sectional observational study in the northwestern coastal region of Ecuador, in canton Eloy Alfaro, Esmeraldas Province, between June 2006 and October 2008. Women aged 14 to 75 years from 20 remote communities participated in the study. According to the 2010 census, this region was mainly inhabited by Afro-Ecuadorians (43.9%; 234,467 people) and Mestizos (44.7%; 238,739), with a smaller proportion of indigenous Amerindians (2.8%; 10,222 Chachi people) and 8.3% other ethnic/racial identities [26, 27].
The sample size was based on previous studies in Ecuador and data from the Ministry of Public Health estimating the prevalence of HPV infection to range between 40 and 80%. To estimate prevalence with 95% confidence and a 5% margin of error, we projected a need for approximately 245 to 360 patients [28].
We employed convenience sampling to recruit female patients who were receiving gynecologist care at Hospital General de Borbón. Participants were also invited by a gynecologist in a medical expedition aimed at accessing remote communities. Eligible participants were women who had not undergone a Pap smear in the previous year or had never undergone one, were not pregnant, were not actively menstruating, and had not undergone a hysterectomy.
Data collection
A trained team member interviewed participants with a short survey regarding sociodemographic and sexual history information. In conjunction with community leaders, we opted to use interviewers to facilitate survey completion among all participants. This allowed us to respect cultural oral traditions from the Chachis and unify data collection strategies across different literacy levels in the communities. Ethnicity was self-reported, and age in years was reported at the time of the survey and divided into four categories for analysis (under 25, 25 to 34, 35 to 44, and 45 +). Additionally, a survey collected data on community access (only road, only by river, both road and river), number of life sexual partners (0, 1, 2 to 3, 4 or more), start of sexual activity (< 15 years, 15–18, > 18), number of pregnancies (1 to 3, 4 to 6, 7 +), any gynecological symptoms reported at the time of the survey (yes/no), and current birth control use (none/any). We decided to omit educational data due to the prevalent lack of education or limited primary education among participants.
Sample collection
We collected a total of 291 samples of ecto- and endocervix using a cytobrush for HPV DNA extraction. We stored the samples in sterile phosphate buffered saline solution (PBS) 1X (37-mM NaCl, 2.7-mM KCl, 4.3-mM Na2HPO4.7H2O, 1.4-mM KH2PO4, pH 7.0) at − 20 °C until molecular analysis. The time elapsed between sample collection and processing was 2 weeks. We conducted DNA extraction at the Instituto de Microbiología of the Universidad San Francisco de Quito.
DNA extraction and HPV genotyping
For DNA extraction, we used a modified cetyl trimethyl ammonium bromide (CTAB) protocol [19]. We released the cervical cells from the cytobrush by agitation and washed twice in 1X PBS solution, pH 7. We lysed the pelleted cells with 700-μl lysis buffer (2% CTAB weigh/vol, 1.4-M NaCl, 20-mM EDTA pH 8, 100-mM Tris–HCl, pH 8) and incubated for 2 h at 65 °C with homogenization each 30 min. We used chloroform:alcohol-isoamyl (24:1) for the extraction of DNA followed by precipitation with 100% ethanol and sodium acetate 3 M (pH 5). Finally, we resuspended the DNA in 50 μl of Tris–EDTA buffer (TE; 10-mM Tris–HCl, pH 8, 0.1-mM EDTA) and stored it at − 20 °C [19]. We determined the quantity and quality of the genomic DNA using a NanoDrop™ 1000 Spectrophotometer (Thermo Scientific) according to the manufacturer’s instructions.
We used the β-actin partial gene as internal control to analyze the quality of template DNA. We amplified a fragment of 290 bp by PCR according to du Breuil et al. [29]. For HPV genotyping, we considered only those samples successfully amplified.
We carried out the detection of HPV by amplification of the L1 gene, as described elsewhere [30], with minor changes. Briefly, we prepared amplification reactions in 20-μl reaction mixture containing a 1X reaction buffer, 1.5-mM MgCl2, 200-μM of each dNTP, 0.25-μM of primers MY09 (5′CGTCCMARRGGAWACTGATC3′) and MY11 (5′GCMCAGGGWCATAAYAATGG3′), 1 U of GoTaq DNA Polymerase (Promega Corporation, Madison), and 20 ng of DNA. The amplification program had an initial denaturation of 94 °C for 3 min, followed by 40 cycles of 1 min each (denaturation at 94 °C, annealing at 55 °C, and elongation at 72 °C). The final extension step was done at 72 °C for 10 min. We analyzed the PCR products on 1.5% agarose gels, visualized by ethidium bromide staining under UV light exposure. We used DNAse-free water as negative control and an HPV-infected sample as positive control.
We performed the HPV genotyping using a nested multiplex PCR described previously by Sotlar et al. [30]. First, we carried out a PCR with a mix of three degenerate consensus primers: GP-E6-3F (5′-GGGWGKKACTGAAATCGGT-3′), GP-E6-5B (5′-CTGAGCTGTCARNTAATTGCTCA-3′), GP-E6-6B (5′-TCCTCTGAGTYGYCTAATTGCTC-3′). We amplified a fragment of 630 bp of the viral E6-E7 oncogenes. We carried out E6/E7 PCR amplification reactions in 20-μl reaction mixture containing 1X PCR buffer, 3-mM MgCl2, 200 μM of each dNTP, 0.25 μM of each primer (E6/E7), 0.7 U GoTaq DNA polymerase (Promega Corporation, Madison), and 200 ng of DNA. PCR conditions consisted of an initial denaturation step at 92 °C for 2 min, then 36 cycles of denaturation at 92 °C for 50 s, annealing at 45 °C for 50 s, and extension at 72 °C for 50 s, followed by a final extension step at 72 °C for 10 min. After that, we carried out a multiplex PCR with four cocktails, each one containing four or five different primers pairs. We used a total of 18 pairs of genotype-specific internal nested PCR primers in a multiplex cocktail for high-risk genotypes: 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, and 68 and low-risk genotypes: 6/11, 42, 43, and 44 [30]. We performed nested PCR amplification reactions in 20-μl reaction mixture containing 1X PCR buffer, 2.5-mM MgCl2, 200 μM of each dNTP, 0.75 μM of each primer, 0.7 U of Taq DNA polymerase (Promega Corporation, Madison), and 2 μl of E6/E7 amplicon. PCR conditions consisted of an initial denaturation step at 94 °C for 4 min, followed by 35 cycles of denaturation at 92 °C for 30 s, annealing at 56 °C for 30 s, and extension at 72 °C for 45 s, followed by a final extension step at 72 °C for 10 min. We analyzed the PCR products on 1.5% agarose gels, visualized by ethidium bromide staining under UV light exposure, and finally photographed. We used a reaction mixture with PCR water as negative control. We delivered results of HPV genotyping to the local healthcare center.
Variant analysis
We chose all mono-infected samples with the most common genotypes (HPV-16 and 58) for variant analyses. We purified the DNA fragments of gene L1 from agarose gels with PureLink Quick Gel Extraction and PCR Purification Combo (Invitrogen, Carlsbad) according to the manufacturer’s instructions. We sequenced the purified samples at Functional Biosciences (https://functionalbio.com/web/) and submitted them to GenBank (Accession numbers MK303335-MK303343). We aligned each gene nucleotide sequence independently with HPV-16 and 58 reference variants from GenBank using MEGA software version X [31]. For phylogenetic analyses, we included other Ecuadorian HPV-16 and 58 L1 gene sequences submitted to GenBank (Accession numbers KP794892-KP794894, KP794914, KP794917, and KP794918) by Mejía et al. [16]. We used representative genomes for HPV-16 (termed A, B) and 58 lineages (termed A, C) and sub-linages (A1-A4/B2 for HPV-16 and A1-A3 for HPV-58) as variant references [13]. Evolutionary history was inferred using the maximum likelihood method and Tamura 3-parameter model [32]. The percentage of trees in which the associated taxa clustered together is shown next to the branches. Initial tree(s) for the heuristic search were obtained automatically by applying neighbor-join and BioNJ algorithms to a matrix of pairwise distances estimated using the maximum composite likelihood (MCL) approach and then selecting the topology with superior log-likelihood value. Evolutionary analyses were conducted in MEGA X [31].
Statistical analyses
We summarized demographic characteristics using frequency tables. Prevalence of HPV infection was coded as positive if the presence of any of the tested genotypes was detected. If a single genotype was detected, the case was deemed a mono-infection, and if more than one genotype was detected, it was deemed a co-infection. We estimated the prevalence of overall HPV infection, co-infection, and by each specific genotype in the general sample, as well as stratified by ethnic group.
To identify risk factors associated with HPV infection and co-infection, we used univariate and multivariate logistic regression to calculate odds ratio (OR) and Wald 95% confidence intervals (CI). All statistical analysis was conducted in Stata 16.1 [33].
Results
A total of 291 women participated in the study, aged 14 to 75 years with a median age of 33 years. Most of them identified as Afro-Ecuadorian (73.5%), and 60.5% lived in communities only accessible by river (Table 1). Most participants (59.5%) reported having 1 life sexual partner, with 24.1% mentioning they had started sexual activity between 15 and 18 years of age, but over 61% had missing information on this variable.
As shown in Table 2, among the 291 women included in the study, 56% were positive for HPV (57% among Afro-Ecuadorian women and 53% among Chachi women). Mono-infections were more common than co-infections in both Afro-Ecuadorian (76%) and Chachi women (79%). Among 163 positive HPV samples, the most common genotype was HPV-58 (37% of all positive samples) followed by HPV-16 (28%) and HPV-68 (13%). Low-risk genotypes 6/11 were present in 20 of the positive samples representing 12% of the HPV cases, but only 4 of these were present as mono-infections; the remaining 16 were present as co-infections with high-risk genotypes. Oncogenic type HPV-18 was only identified in 1% of the positive samples (Table 2).
A total of nine positive samples from mono-infections of HPV-16 (seven) and HPV-58 (two) were used for the amplification and sequencing of the L1 gene. The sequences’ length mean was 351 bp (range 291–422). All nucleotide sequences from HPV-16 amplicons (seven samples) grouped into the European branch (lineage A; Fig. 1), independently of their ethnic origin. The sublineage could not be identified since all sequences grouped into A1 (NC001526) and A4 variants with no characteristic SNPs to differentiate them. Regarding HPV-58, the two sequences (one Chachi sample and one from an Afro-Ecuadorian woman) pooled into the A2 sublineage (Fig. 2); nevertheless, the Afro-Ecuadorian sample showed a SNP in G6641A of gene L1.
Maximum-likelihood tree using nucleotide sequences of L1 genes from HPV-16 mono-infected samples obtained in this study (MK303335-MK303341). Sequences reported here are denoted as Chachi, and Afroec for Afro-Ecuadorian, followed by the initials of the names of the locations. B, Borbon; MP, Mata de Plátano; LLI, Loma Linda I; LLII, Loma Linda II; Z, Zapallo; M, Maldonado; T, Tigüinza. L1 sequences from Mejía et al. [16] (KP794892-KP794894) were included in the analysis. Representative genomes for HPV-16 lineages (termed A, B) and sublineages (termed A1, A2, A3, A4/B2) were used as variant references [13]. Regional variants are indicated as follows: E, European variant; As, East Asian; G, German; Afr, African
Maximum-likelihood tree using nucleotide sequences of L1 genes from HPV-58 mono-infected samples obtained in this study (MK303342 and MK303343). Sequences reported here are denoted as Chachi, and Afroec for Afro-Ecuadorian, followed by the initials of the name of the locations. B, Borbon; SM, San Miguel. L1 sequences from Mejía et al. [16] (KP794914, KP794917, and KP794918) were also included in the analysis. Representative genomes for HPV-58 lineages (termed A, C) and sublineages (termed A1, A2, A3) were used as variant references [13]
Based on univariate (crude) logistic regression, we identified that community access and number of life sexual partners were associated to prevalence of HPV infection, while ethnicity, age, start of sexual activity, and whether symptoms were reported at the time of the survey were not (Table 3). Specifically, women from communities only accessible by river had 51% less chance of HPV infection than women in communities accessible by road (OR: 0.49, 95% CI: 0.28, 0.86). On the other hand, participants with 2 to 3 life partners were 1.83 (95% CI: 1.06, 3.15) times more likely to be HPV positive than participants with 0 or 1 life sexual partners. When we adjusted for ethnicity, age, road access, and number of sexual partners, we found that Afro-Ecuadorian women were less likely to have an HPV infection than Chachi women (OR: 0.49, 95% CI: 0.25, 0.96), and that participants in communities only accessible by river had 64% less chances of an HPV infection when compared to women in communities accessible by road (OR: 0.36, 95% CI: 0.19, 0.71), and women with 2 to 3 sexual partners had 2.47 times the odds of HPV infection than participants with 0–1 partners (OR: 2.47, 95% CI: 1.32, 4.6).
Similarly, univariate (crude) logistic regression models in Table 4 identified number of life sexual partners and age of start of sexual activity as factors associated with co-infection. Specifically, women with 2 to 3 life partners were 2.39 (95% CI: 1.31, 4.36) times more likely to have an HPV co-infection than participants with 0 or 1 life sexual partners. When we adjusted for ethnicity, age, road access, and number of sexual partners, we found that women with 2 to 3 sexual partners had 3.48 times the odds of HPV infection than participants with 0–1 partners (OR: 3.48, 95% CI: 1.72, 7.02), and that women with 4 or more sexual partners had 3.58 times the odds of HPV infection than participants with 0–1 partners (OR: 3.58, 95% CI: 1.15, 11.1).
Discussion
In this study population, we found a period prevalence of HPV infection of 56% (Chachis 53% and Afro-Ecuadorian 57%). This value is comparable with the study conducted by Paez et al. [34], where women with normal and precancerous cervical lesions from rural areas of Ecuador were included. Similar values have also been reported in women from rural communities in other South American countries such as Brazil (53.3%) and Argentina (51.6%) [35, 36]. Surprisingly, HPV-58 was the most common HR-HPV, unlike other studies where HPV-16 is most prevalent [16, 28, 37, 38]. In Ecuador, HPV-58 was reported as the second genotype most frequently associated with cancer [16]. On the other hand, HPV-18 represented only 1% of infections, as in previous reports from Ecuador [23, 37, 38]. The same phenomenon has been described in other South American countries [39,40,41]. HPV-16 (20%) was the most prevalent in Afro-Ecuadorian women whereas HPV-58 (30%) in Chachis women which is consistent with other studies conducted in Ecuador [16, 23]. It is known that the prevalence of HR-HPV genotypes differs from one human population to another [8, 9]. Logistic and sociocultural variables could also be related to the presence of certain HPV types in the studied ethnic groups [22, 42, 43]. Although Chachis and Afro-Ecuadorian women are found in the same region, each group inhabit specific geographic areas that are difficult to access. This isolation may influence the dynamics of the circulation of HPV genotypes as suggested by Batista et al. [44]. In addition, the difference of host genetic background could contribute to the prevalence of a specific HR-HPV genotype. In particular, the HLAs alleles may play an important role in determining which HPV variant will clear or persist and progress to cervical cancer [45, 46].
It is important to highlight the presence of HR-HPV 68 and 39 which were described in lower rates in other Ecuadorian studies [16, 47,48,49]. HPV-68 was found mainly in co-infections, as described by others [16, 50,51,52]. Interestingly, the high HPV-39 prevalence has also been observed in women from Bahía, Brazil [37], and urban women from China [53]. Also, we found a prevalence of HPV-52 (6%) similar to data from East Asia where HPV-52 and -58 are more prevalent compared to worldwide [54, 55]. Most infections with low-risk genotypes (6, 11, and 43) were co-infected with HR-HPV. Something similar has been found in other studies where the prevalence of co-infections is greater than 50% [16, 56]. Therefore, knowledge of the regional prevalence of HPV genotypes is essential for the development of effective vaccination as well as preventative screening strategies against cervical cancer.
All HPV-16 sequences found in this study belonged to the European lineage regardless its ethnical origin which is in accordance with the previously published investigation in Ecuador and other rural populations in Latin America [16, 17, 28, 57, 58]. This lineage tends to be the least carcinogenic and persistent in comparison to the non-European variants, which show increased risk of developing cancerous lesions [12, 13]. All HPV-16 sequences grouped indistinctly into A1 and A4 sublineages. No specific polymorphisms were found in our sequences when compared to the HPV-16 European prototype, and they were similar to previous studies in Ecuadorian mestizo women with HPV-16 positive infection [16]. Both HPV-58 sequences in this study belonged to the A2 sublineage, which is the most common variant around the world [59] and has a lower risk of disease progression than A3 and A1 sublineages [13, 14, 60]. Our findings on HPV-16 and HPV-58 showed no difference between ethnicity, Chachi, Afro-Ecuadorian, and mestizo sequences. One SNP (G6641A, synonymous mutation) was found in one sequence from an Afro-Ecuadorian sample, and it has been previously described [61, 62].
We identified two risk factors that influenced HPV infection in this population: number of life sexual partners and community access by road (vs. river). Several studies have previously reported that higher number of sexual partners increases the risk of HPV infection and co-infections [63, 64]. A study in Mexico with 115,651 participants found that women with 6 or more lifetime sexual partner had twice the prevalence of HR-HPV infection than women with 1–5 partners [65]. In our smaller study of women from remote communities, we also found that having more than one lifetime sexual partner more than doubled the odds of HR-HPV infection after adjusting for other covariates. On the other hand, we found that women living in communities only accessible by river had a third of the odds of HR-HPV infection than women in areas more readily accessible by road. In isolated communities with access only by river, the flow of HPV-infected individuals might be restricted and, therefore, the probability of HPV infection might be lower. Similarly, Eisenberg et al. (2006) [66] evaluated the impact of road construction in this region on the epidemiology of diarrheal diseases. They noted higher infection rates of intestinal pathogens in communities with road access than in remote communities with only river access.
Much less has been discussed on the association between road accessibility and prevalence of HPV in remote communities. Notably, a study of HPV and other sexually transmitted infections in rural communities in Bolivia found no differences in the prevalence of HR-HPV infection between women from large towns, small towns, and villages [22]. Meanwhile, a different study among Amerindians from the Venezuelan Amazon reported an upward trend of the prevalence of any HPV as the urbanicity of communities increased [67]. The study also reported lower HPV diversity among more isolated Amerindians suggesting that geographic barriers may influence the viral genetic pool in communities that are harder to reach.
This study has limitations to note. Interviewer bias may have been introduced because participants did not complete surveys on their own but were assisted by a team member. As was previously mentioned, this was done to accommodate different cultural traditions and literacy levels. To minimize its impact, all team members were well trained in data collection methods and instructed to use a neutral nonjudgmental tone with all participants. We did not provide a specific definition of what a sexual partner or sexual activity entailed, which allowed participants to answer these questions based on their own definitions. For example, some may have had sexual activity including oral sex, but since it did not include penetration, they may not consider that as sexual activity or the other person as a sexual partner [68]. Additionally, this study included participants younger than 30 years of age and as young as 14, which is inconsistent with most current guidelines and may lead to false positive cases [69, 70]. Data for this study was collected before national and international guidelines were developed and when much less was known about the physiopathology of HPV. Currently, some debate still remains about the potential benefits of screening women younger than 30 [71]. Our small sample size may limit generalizability of findings, including populations in northwestern Ecuador. However, this cross-sectional study did not aim to discuss prevalence of HPV across the population of the area but to examine its prevalence in specific minoritized communities of Ecuador who mainly reside in the province of Esmeraldas.
Finally, our study contributes to a better understanding of HPV genotype distribution within Chachis and Afro-Ecuadorian populations that have been underrepresented in HPV research. The identification of HPV-58 as the most prevalent high-risk genotype provides valuable information that can be useful for vaccination strategies and screening programs in these populations.
Conclusions
This study provides a baseline knowledge about the prevalence and distribution of HPV genotypes in the northwestern coastal of Ecuador. Prevalence of HPV in this region was higher compared to previous studies conducted in other regions of Ecuador. The most frequent genotypes were HPV-58, -16, -68, and -39. Studies of HPV prevalence are especially relevant in remote communities where access to health care is very limited. The distribution of the HPV genotypes varied according to the ethnic group. Most results were consistent with previous studies in Ecuador suggesting that geographic location is an important predictor of genotype type. Differences in the frequency of HPV genotypes in Amerindian and Afro populations should be further investigated. Conducting this study in remote populations of northwestern Ecuador represents a pioneering effort aimed at assessing the prevalence of HPV and circulating genotypes, with the goal of combating cervical cancer disparities. Notably, Ecuador lacked a national HPV vaccination plan during the study period, whose implementation began in 2014 using the bivalent vaccine (Cervarix®). However, as this article highlights, the vaccine may offer limited protection among communities where other genotypes circulate. An updated assessment in a post-vaccine era could shed light on the actual efficacy of this strategy among remote communities.
Availability of data and materials
The data and materials produced and examined in this study are not accessible to the public because of confidentiality agreements. Nonetheless, reasonable requests for access will be evaluated individually. Inquiries for access to the confidential data should be sent to the corresponding author at szapata@usfq.edu.ec. Each request will be assessed by the institutional ethics committee to ensure adherence to privacy and confidentiality guidelines.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49. https://doi.org/10.3322/caac.21660.
Bruni L, Albero G, Serrano B, et al. Human papillomavirus and related diseases in Ecuador. ICO/IARC Information Centre on HPV and Cancer (HPV Information Centre). Available from: https://hpvcentre.net/statistics/reports/ECU.pdf. Published, 2021. Accessed 20 Sept. 2022.
World Health Organization. Ecuador. International Agency for Research on Cancer (IARC). GLOBOCAN. Disponible en http://gco.iarc.fr/today/data/factsheets/populations/218-ecuador-fact-sheets.pdf. Published, 2020. Accessed 20 Sept. 2022.
The International Agency for Research on Cancer. Human papillomaviruses: IARC Monographs on the evaluation of carcinogenic risks to humans 100B. Ginebra, Suiza: World Health Organization; 2006. Available from: http://monographs.iarc.fr/ENG/Monographs/vol100B/mono100B-11.pdf. Published, 2012. Accessed 20 Sept. 2022
Bruni L, Diaz M, Castellsagué X, Ferrer E, Bosch FX, de Sanjosé S. Cervical human papillomavirus prevalence in 5 continents: meta-analysis of 1 million women with normal cytological findings. J Infect Dis. 2010;202(12):1789–99. https://doi.org/10.1086/657321.
Ciapponi A, Bardach A, Glujovsky D, Gibbons L, Picconi MA. Type-specific HPV prevalence in cervical cancer and high-grade lesions in Latin America and the Caribbean: systematic review and meta-analysis. Plos One. 2011;6(10):e25493. https://doi.org/10.1371/journal.pone.0025493.
Guan P, Howell-Jones R, Li N, Bruni L, de Sanjosé S, Franceschi S, et al. Human papillomavirus types in 115,789 HPV-positive women: a meta-analysis from cervical infection to cancer. Int J Cancer. 2012;131(10):2349–59. https://doi.org/10.1002/ijc.27485.
Li N, Franceschi S, Howell-Jones R, Snijders PJF, Clifford GM. Human papillomavirus type distribution in 30,848 invasive cervical cancers worldwide: variation by geographical region, histological type and year of publication. Int J Cancer. 2011;128(4):927–35. https://doi.org/10.1002/ijc.25396.
de Sanjose S, Quint WG, Alemany L, Geraets DT, Klaustermeier JE, Lloveras B, et al. Human papillomavirus genotype attribution in invasive cervical cancer: a retrospective cross-sectional worldwide study. Lancet Oncol. 2010;11(11):1048–56. https://doi.org/10.1016/S1470-2045(10)70230-8.
Ogembo RK, Gona PN, Seymour AJ, Park HS-M, Bain PA, Maranda L, et al. Prevalence of human papillomavirus genotypes among African women with normal cervical cytology and neoplasia: a systematic review and meta-analysis. Plos One. 2015;10(4):e0122488. https://doi.org/10.1371/journal.pone.0122488.
Chan PKS, Ho WCS, Chan MCW, Wong MCS, Yeung ACM, Chor JSY, et al. Meta-analysis on prevalence and attribution of human papillomavirus types 52 and 58 in cervical neoplasia worldwide. Plos One. 2014;9(9):e107573. https://doi.org/10.1371/journal.pone.0107573.
Schiffman M, Rodriguez AC, Chen Z, Wacholder S, Herrero R, Hildesheim A, et al. A population-based prospective study of carcinogenic human papillomavirus variant lineages, viral persistence, and cervical neoplasia. Cancer Res. 2010;70(8):3159–69. https://doi.org/10.1158/0008-5472.can-09-4179.
Burk RD, Harari A, Chen Z. Human papillomavirus genome variants. Virology. 2013;445(1–2):232–43. https://doi.org/10.1016/j.virol.2013.07.018.
Chen Z, Ho WCS, Boon SS, Law PTY, Chan MCW, DeSalle R, et al. Ancient evolution and dispersion of human papillomavirus 58 variants. J Virol. 2017;91(21):e01285. https://doi.org/10.1128/jvi.01285-17.
Zehbe I, Tachezy R, Mytilineos J, Voglino G, Mikyskova I, Delius H, et al. Human papillomavirus 16 E6 polymorphisms in cervical lesions from different European populations and their correlation with human leukocyte antigen class II haplotypes. Int J Cancer. 2001;94(5):711–6. https://doi.org/10.1002/ijc.1520.
Mejía L, Muñoz D, Trueba G, Tinoco L, Zapata S. Prevalence of human papillomavirus types in cervical cancerous and precancerous lesions of Ecuadorian women: HPV types on cervical cancer in Ecuadorian women. J Med Virol. 2016;88(1):144–52. https://doi.org/10.1002/jmv.24310.
Nugus P, Désalliers J, Morales J, Graves L, Evans A, Macaulay AC. Localizing global medicine: challenges and opportunities in cervical screening in an indigenous community in Ecuador. Qual Health Res. 2018;28(5):800–12. https://doi.org/10.1177/1049732317742129.
Barrett BW, Paz-Soldan VA, Mendoza-Cervantes D, Sánchez GM, Córdova López JJ, Gravitt PE, et al. Understanding geospatial factors associated with cervical cancer screening uptake in Amazonian Peruvian women. JCO Glob Oncol. 2020;6(6):1237–47. https://doi.org/10.1200/GO.20.00096.
Tonon SA, Picconi MA, Zinovich JB, Nardari W, Mampaey M, Badano I, et al. Human papillomavirus cervical infection in Guarani Indians from the rainforest of Misiones. Argentina Int J Infect Dis. 2004;8(1):13–9. https://doi.org/10.1016/j.ijid.2003.03.001.
Soto-De Leon SC, Camargo M, Sanchez R, Leon S, Urquiza M, Acosta J, et al. Prevalence of infection with high-risk human papillomavirus in women in Colombia. Clin Microbiol Infect. 2009;15(1):100–2. https://doi.org/10.1111/j.1469-0691.2008.02120.x.
Deluca GD, Basiletti J, González JV, Díaz Vásquez N, Lucero RH, Picconi MA. Human papilloma virus risk factors for infection and genotype distribution in aboriginal women from Northern Argentina. Medicina (B Aires). 2012;72(6):461–6.
Patzi-Churqui M, Terrazas-Aranda K, Liljeqvist J-Å, Lindh M, Eriksson K. Prevalence of viral sexually transmitted infections and HPV high-risk genotypes in women in rural communities in the Department of La Paz, Bolivia. BMC Infect Dis. 2020;20(1):204. https://doi.org/10.1186/s12879-020-4931-1.
Ortiz Segarra J, Vega Crespo B, Campoverde Cisneros A, Salazar Torres K, Delgado López D, Ortiz S. Human papillomavirus prevalence and associated factors in indigenous women in Ecuador: a cross-sectional analytical study. Infect Dis Rep. 2023;15(3):267–78. https://doi.org/10.3390/idr15030027.
Carrero Y, Proaño-Pérez E, Vásquez F, et al. Infección por VPH y su correlación clínica en población indígena de la región altoandina del Ecuador. Kasmera. 2018;11:152–8.
Carrión Ordoñez JI, Soto Brito Y, Pupo Antúnez M, Loja Chango R. Infección por Virus del Papiloma Humano y citología cérvico-vaginal en mujeres indígenas del Cañar. Ecuador Bionatura. 2019;4(3):934–8. https://doi.org/10.21931/rb/2019.04.03.10.
Whitten NE. Class, kinship, and power in an Ecuadorian Town: The Negroes of San Lorenzo. Stanford: Stanford University Press; 1965.
Power BI report. Powerbi.com. Available from: https://app.powerbi.com/view?r=eyJrIjoiNWUzMjQwOWMtZjFhOS00NjczLTk0YTItNjcwZmRmY2YxMjkyIiwidCI6ImYxNThhMmU4LWNhZWMtNDQwNi1iMGFiLWY1ZTI1OWJkYTExMiJ9. Accessed 16 Apr 2024.
Tornesello ML, Buonaguro L, Izzo S, Lopez G, Vega X, Maldonado Reyes CF, et al. A pilot study on the distribution of human papillomavirus genotypes and HPV-16 variants in cervical neoplastic lesions from Ecuadorian women. J Med Virol. 2008;80(11):1959–65. https://doi.org/10.1002/jmv.21317.
du Breuil RM, Patel JM, Mendelow BV. Quantitation of beta-actin-specific mRNA transcripts using xeno-competitive PCR. Genome Res. 1993;3(1):57–9. https://doi.org/10.1101/gr.3.1.57.
Sotlar K, Stubner A, Diemer D, Menton S, Menton M, Dietz K, et al. Detection of high-risk human papillomavirus E6 and E7 oncogene transcripts in cervical scrapes by nested RT-polymerase chain reaction: HPV E6 and E7 oncogene transcripts. J Med Virol. 2004;74(1):107–16. https://doi.org/10.1002/jmv.20153.
Kumar S, Stecher G, Li M, Knyaz C, Tamura K. MEGA X: molecular evolutionary genetics analysis across computing platforms. Mol Biol Evol. 2018;35(6):1547–9. https://doi.org/10.1093/molbev/msy096.
Tamura K. Estimation of the number of nucleotide substitutions when there are strong transition-transversion and G+ C-content biases. Mol Biol Evol. 1992;9(4):678–87.
Stata Statistical Software. Release 16. College Station, TX: StataCorp LLC.; 2019.
Paez C, Konno R, Yaegashi N, Matsunaga G, Araujo I, Corral F, et al. Prevalence of HPV DNA in cervical lesions in patients from Ecuador and Japan. Tohoku J Exp Med. 1996;180(3):261–72. https://doi.org/10.1620/tjem.180.261.
Paesi S, Serafini EP, Barea F, Madi SRC, Echeverrigaray S. High prevalence of human papillomavirus type 58 in patients with cervical pre-malignant lesions in southern Brazil. J Med Virol. 2009;81(7):1270–5. https://doi.org/10.1002/jmv.21410.
Venezuela RF, Kiguen AX, Frutos MC, Cuffini CG. Circulation of human papillomavirus (HPV) genotypes in women from Córdoba, Argentina, with squamous intraepithelial lesions. Rev Inst Med Trop Sao Paulo. 2012;54(1):11–6. https://doi.org/10.1590/s0036-46652012000100003.
Dalgo Aguilar P, Loján González C, Córdova Rodríguez A, Acurio Páez K, Arévalo AP, Bobokova J. Prevalence of high-risk genotypes of human papillomavirus: women diagnosed with premalignant and malignant pap smear tests in southern Ecuador. Infect Dis Obstet Gynecol. 2017;2017:8572065. https://doi.org/10.1155/2017/8572065.
Bedoya-Pilozo CH, Medina Magües LG, Espinosa-García M, Sánchez M, Parrales Valdiviezo JV, Molina D, et al. Molecular epidemiology and phylogenetic analysis of human papillomavirus infection in women with cervical lesions and cancer from the coastal region of Ecuador. Rev Argent Microbiol. 2018;50(2):136–46. https://doi.org/10.1016/j.ram.2017.06.004.
Bruno A, Serravalle K, Travassos AG, de Lima BGC. Genotype distribution of human papillomavirus in women from the state of Bahia Brazil. Rev Bras Ginecol Obstet. 2014;36(9):416–22. https://doi.org/10.1590/so100-720320140004995.
Queiroz FA, Rocha DA, Filho RAB, Santos CMB. Detection and genotyping of HPV in women with indeterminate cytology and low-grade squamous intraepithelial lesions. J Bras Patol Med Lab. 2015;51(3):166–72. https://doi.org/10.5935/1676-2444.20150029.
Martins TR, de Oliveira Mendes C, Rosa LR, de Centrone Campos C, Rodrigues CLR, Villa LL, et al. HPV genotype distribution in Brazilian women with and without cervical lesions: correlation to cytological data. Virol J. 2016;13(1):138. https://doi.org/10.1186/s12985-016-0594-3.
Baloch Z, Yuan T, Wang B, Tai W, Feng Y, Liu Y, et al. Ethnic and geographic variations in HPV prevalence and genotype distribution in north-western Yunnan, China: ethnic and geographic variations in HPV prevalence. J Med Virol. 2016;88(3):532–40. https://doi.org/10.1002/jmv.24352.
Mongelos P, Mendoza LP, Rodriguez-Riveros I, Castro A, Gimenez G, Araujo P, et al. Distribution of human papillomavirus (HPV) genotypes and bacterial vaginosis presence in cervical samples from Paraguayan indigenous. Int J Infect Dis. 2015;39:44–9. https://doi.org/10.1016/j.ijid.2015.08.007.
Batista JE, Saddi VA, de Carvalho KPA, Ribeiro AA, Segati KD, Carneiro MADS, et al. Human papillomavirus genotypes 68 and 58 are the most prevalent genotypes in women from quilombo communities in the state of Maranhão Brazil. Int J Infect Dis. 2017;55:51–5. https://doi.org/10.1016/j.ijid.2017.01.001.
Del Río-Ospina L, Camargo M, Soto-De León SC, Sánchez R, Moreno-Pérez DA, Patarroyo ME, et al. Identifying the HLA DRB1-DQB1 molecules and predicting epitopes associated with high-risk HPV infection clearance and redetection. Sci Rep. 2020;10(1):7306. https://doi.org/10.1038/s41598-020-64268-x.
Mora MJ, de Los Ángeles Bayas-Rea R, Mejía L, Cruz C, Guerra S, Calle P, et al. Identification of human leukocyte antigen in precancerous and cancerous cervical lesions from Ecuadorian women. Infect Genet Evol. 2022;105(105365):105365. https://doi.org/10.1016/j.meegid.2022.105365.
Tigre Sinchi PS, Salazar Torres ZK, Espinosa Martin L, Aspiazu Hinostroza KA, Espinosa HM, Cárdena Heredia FR. Human papilloma virus genotypes in type III cervical intraepithelial neoplasia. Cuenca-Ecuador, 2013–2017. Kasmera. 2019;47:95. https://doi.org/10.5281/ZENODO.3521760.
Altamirano GSF, Montenegro W, Silva R. Prevalence and molecular epidemiology of human papillomavirus in Ecuadorian women with cervical cytological abnormalities. J Data Mining Genomics Proteomics. 2015;06(02):2153. https://doi.org/10.4172/2153-0602.1000174.
García Muentes GD, García Rodríguez LK, Burgos Galarraga RI, Almeida Carpio F, Ruiz Cabezas JC. Genotypes distribution of human papillomavirus in cervical samples of Ecuadorian women. Rev Bras Epidemiol. 2016;19(1):160–6. https://doi.org/10.1590/1980-5497201600010014.
Carrillo-García A, Ponce-de-León-Rosales S, Cantú-de-León D, Fragoso-Ontiveros V, Martínez-Ramírez I, Orozco-Colín A, et al. Impact of human papillomavirus coinfections on the risk of high-grade squamous intraepithelial lesion and cervical cancer. Gynecol Oncol. 2014;134(3):534–9. https://doi.org/10.1016/j.ygyno.2014.06.018.
Ramas V, Mirazo S, Bonilla S, Mendoza L, Lago O, Basiletti J, et al. Human papillomavirus genotypes distribution in cervical samples from Uruguayan women. J Med Virol. 2013;85(5):845–51. https://doi.org/10.1002/jmv.23479.
Aguilar-Lemarroy A, Vallejo-Ruiz V, Cortés-Gutiérrez EI, Salgado-Bernabé ME, Ramos-González NP, Ortega-Cervantes L, et al. Human papillomavirus infections in Mexican women with normal cytology, precancerous lesions, and cervical cancer: type-specific prevalence and HPV coinfections: genotyping and coinfection with HPV in Mexican women. J Med Virol. 2015;87(5):871–84. https://doi.org/10.1002/jmv.24099.
Baloch Z, Yuan T, Yindi S, Feng Y, Tai W, Liu Y, et al. Prevalence of genital human papillomavirus among rural and urban populations in southern Yunnan province, China. Braz J Med Biol Res. 2016;49(6):e5254. https://doi.org/10.1590/1414-431X20165254.
Zhao X-L, Hu S-Y, Zhang Q, Dong L, Feng R-M, Han R, et al. High-risk human papillomavirus genotype distribution and attribution to cervical cancer and precancerous lesions in a rural Chinese population. J Gynecol Oncol. 2017;28(4):e30. https://doi.org/10.3802/jgo.2017.28.e30.
Li M, Du X, Lu M, Zhang W, Sun Z, Li L, et al. Prevalence characteristics of single and multiple HPV infections in women with cervical cancer and precancerous lesions in Beijing China. J Med Virol. 2019;91(3):473–81. https://doi.org/10.1002/jmv.25331.
Padilla-Mendoza JR, Gómez-López LA, López-Casamichana M, Azuara-Liceaga EI, Cortés-Malagón EM, López-Cánovas L, et al. Human papillomavirus coinfection in the cervical intraepithelial lesions and cancer of Mexican patients. Biomed Res Int. 2020;2020:4542320. https://doi.org/10.1155/2020/4542320.
Lopera EA, Baena A, Florez V, Montiel J, Duque C, Ramirez T, et al. Unexpected inverse correlation between Native American ancestry and Asian American variants of HPV16 in admixed Colombian cervical cancer cases. Infect Genet Evol. 2014;28:339–48. https://doi.org/10.1016/j.meegid.2014.10.014.
Ortiz-Ortiz J, del Alarcón-Romero LC, Jiménez-López MA, Garzón-Barrientos VH, Calleja-Macías I, Barrera-Saldaña HA, et al. Association of human papillomavirus 16 E6 variants with cervical carcinoma and precursor lesions in women from southern Mexico. Virol J. 2015;12(1):29. https://doi.org/10.1186/s12985-015-0242-3.
Chan PKS, Luk ACS, Park J-S, Smith-McCune KK, Palefsky JM, Konno R, et al. Identification of human papillomavirus type 58 lineages and the distribution worldwide. J Infect Dis. 2011;203(11):1565–73. https://doi.org/10.1093/infdis/jir157.
Chan PKS, Zhang C, Park J-S, Smith-McCune KK, Palefsky JM, Giovannelli L, et al. Geographical distribution and oncogenic risk association of human papillomavirus type 58 E6 and E7 sequence variations. Int J Cancer. 2013;132(11):2528–36. https://doi.org/10.1002/ijc.27932.
Liu J-H, Lu Z-T, Wang G-L, Zhou W-Q, Liu C, Yang L-X, et al. Variations of human papillomavirus type 58 E6, E7, L1 genes and long control region in strains from women with cervical lesions in Liaoning province China. Infect Genet Evol. 2012;12(7):1466–72. https://doi.org/10.1016/j.meegid.2012.05.004.
Chen Z, Jing Y, Wen Q, Ding X, Zhang S, Wang T, et al. L1 and L2 gene polymorphisms in HPV-58 and HPV-33: implications for vaccine design and diagnosis. Virol J. 2016;13(1):167. https://doi.org/10.1186/s12985-016-0629-9.
Johnson AM, Mercer CH, Beddows S, de Silva N, Desai S, Howell-Jones R, et al. Epidemiology of, and behavioural risk factors for, sexually transmitted human papillomavirus infection in men and women in Britain. Sex Transm Infect. 2012;88(3):212–7. https://doi.org/10.1136/sextrans-2011-050306.
Wellings K, Collumbien M, Slaymaker E, Singh S, Hodges Z, Patel D, et al. Sexual behaviour in context: a global perspective. Lancet. 2006;368(9548):1706–28. https://doi.org/10.1016/s0140-6736(06)69479-8.
Torres-Poveda K, Ruiz-Fraga I, Madrid-Marina V, Chavez M, Richardson V. High risk HPV infection prevalence and associated cofactors: a population-based study in female ISSSTE beneficiaries attending the HPV screening and early detection of cervical cancer program. BMC Cancer. 2019;19(1):1205. https://doi.org/10.1186/s12885-019-6388-4.
Eisenberg JNS, Cevallos W, Ponce K, Levy K, Bates SJ, Scott JC, et al. Environmental change and infectious disease: how new roads affect the transmission of diarrheal pathogens in rural Ecuador. Proc Natl Acad Sci USA. 2006;103(51):19460–5. https://doi.org/10.1073/pnas.0609431104.
Vargas-Robles D, Magris M, Morales N, de Koning MNC, Rodríguez I, Nieves T, et al. High rate of infection by only oncogenic human papillomavirus in Amerindians. mSphere. 2018;3(3):00176. https://doi.org/10.1128/msphere.00176-18.
Rodríguez-Arauz G, Mealy M, Smith V, DiPlacido J. Sexual behavior in Costa Rica and the United States. Int J Intercult Relat. 2013;37(1):48–57. https://doi.org/10.1016/j.ijintrel.2012.06.002.
De contenidos T. Preguntas frecuentes sobre el VPH. Paho.org. Available from: https://www3.paho.org/hq/index.php?option=com_docman&view=download&alias=48228-preguntas-frecuentes-sobre-vph&category_slug=preguntas-frecuentes-sobre-enfermedades-prevenibles-por-vacunacion&Itemid=270&lang=es#:~:text=La%20prueba%20del%20VPH%20no,se%20convierten%20en%20pre%2Dc%C3%A1ncer. Cited June 4, 2024
Asccp.org. Available from: https://www.asccp.org/guidelines-history__;!!NN-i7gBg!s6GUginVCAvyCHQILO4YRWZv28DVPdY8YqkYNN5CKiZG4FS_sHvIfu0BaDUC93zqzoErjimDAv-AifUfpouavHpVVlutjmwvhe6B$. Cited June 4, 2024
Garzón-Olivares CD, Grillo-Ardila CF, Amaya-Guio J, Vallejo-Ortega MT, Diaz-Cruz LA, Fernández-Motta C, et al. Tamización primaria con prueba ADN-VPH en mujeres menores de 30 años: evaluación de tecnología sanitaria. Rev Colomb Obstet Ginecol. 2022;73(2):203–22. Available from: https://pubmed.ncbi.nlm.nih.gov/35939411/
Acknowledgements
Special thanks to Dr. Simón Quimi and Dr. Edgar Gualoto from General Hospital of Borbón for helping us with sample collection. We are grateful to Carla Torres for her contributions to this manuscript.
Funding
This study was supported by Internal Grants of Universidad San Francisco de Quito 2008.
Author information
Authors and Affiliations
Contributions
KP and SZ conceptualized and designed the project. KP, AG, and RB were involved in sampling, interviewing the participants, and HPV detection and genotyping. LM, JM, and CA performed the variant and molecular analyses. GB performed the statistical analysis. RB, GB, LM, and SZ analyzed the data and wrote the article. All the authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
All the participants were informed of the aims, procedures, and details of the project before they voluntarily decided to participate and gave their informed consent. Adolescent participants assented to participate, and their legal guardians signed the informed consent forms. Written informed consent was obtained This study was approved by the Human Research Ethics Committee (CEISH), and all the participants signed informed consent. All study activities were conducted in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
de los Ángeles Bayas-Rea, R., Ponce, K., Guenther, A. et al. Prevalence of human papillomavirus genotypes in women of different ethnicity from rural northwestern Ecuador. BMC Global Public Health 2, 46 (2024). https://doi.org/10.1186/s44263-024-00078-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s44263-024-00078-x