Abstract
Background
Evidence shows that mindfulness-based programs reduce levels of stress, anxiety, and depression. Yet, web-based mindfulness has been less studied, especially among university students. We developed a student-centered web-based mindfulness virtual community (MVC) intervention informed by cognitive-behavioral-therapy constructs. MVC comprised of (1) 12 online video-based modules (psychoeducation and practice), (2) anonymous peer-to-peer discussion forums, and (3) anonymous, group-based, 20-min live video conferences by a trained moderator. While the intervention was found effective in reducing anxiety and depression in a randomized controlled trial (RCT), the impact on students’ quality of life remained to be examined. The reported study examined the impact of 8-week long web-based MVC intervention on the quality of life of undergraduate students compared to those in the control group. Participants were recruited from a large Canadian university into a two-arm RCT (N = 160) and randomly allocated to the web-based MVC intervention (n = 80) or to the control (n = 80) group. Participants completed online survey at baseline (T1) and at 8-week (T2). The outcome of quality of life was measured by 16-item Quality of Life Scale (QOLS). The generalized estimation equation (GEE) method with AR(1) covariance structures was used, adjusting for potential covariates.
Results
At the baseline 159 students completed the survey. Participants (32 males, 125 females, 2 other gender) had a mean age of 22.6 years, 57.2% were born in Canada. Participants in MVC (n = 79) and control (n = 80) groups were similar in sociodemographic characteristics except hours of volunteer work. At T2 that coincided with students’ exam period, QOLS score for the control group declined while MVC group had a slight increase. Between-group analysis for QOLS score-change showed a significantly higher score at T2 for MVC group compared to the control (81.64, SD = 14.63 vs. 72.9, SD = 17.26, P < 0.001). Per adjusted GEE analysis, the higher QOLS score in MVC compared to the control group was statistically significant (\(\upbeta\) = -2.24, P = .03).
Conclusions
Web-based MVC intervention helped the students to have better quality of life, compared to the control group, at 8-week follow-up despite exam stress. Future research with a longer follow-up would advance understanding.
Trial registration
https://doi.org/10.1186/ISRCTN12249616 Registration Date: 21/06/2017.
Similar content being viewed by others
Introduction
With the growing recognition of ubiquitous stress in modern life, several stress reduction techniques have surfaced during the last few decades. Mindfulness-based stress reduction (MBSR) is one such approach that emerged in the West in the 1980s by drawing from Buddhist mindfulness meditation [1]. In this technique the mindfulness refers to non-judgementally paying attention to one’s sensations, thoughts, emotions and the environment, in the present moment, while embracing openness, curiosity and acceptance [2, 3]. Those examining the mechanisms through which mindfulness training impacts the body, report changes in the areas of brain regulating affect and our reaction to stressful impulses, and these then influence breathing, heart rate, and immune functions [2, 4, 5]. Others report reduction in negative thoughts and emotions [6] and increase in positive thoughts and emotions due to the reappraisal of thoughts and emotions learned through mindfulness [7]. In 2017, the authors of Campbell Collaboration systematic review of MBSR noted its growing adoption in clinical samples for people experiencing chronic conditions like pain, anxiety, depression, burnout or cancer, and in non-clinical samples with high levels of stress such as students, healthcare workers, caregivers, and teachers and in the general population [8]. For mental health outcomes, they found an effect size of 0.54 for studies with inactive control groups and an effect size of 0.18 for studies with active control groups. For the quality of life and social function outcomes pooled together, the effect size was 0.44 for studies with inactive controls and 0.17 for studies with active controls [8].
Not surprisingly, there has been an increasing effort by the scientific community to develop and investigate various types of Mindfulness-Based Interventions (MBI) to improve physical and mental health outcomes [9]. In these MBI approaches, mindfulness meditation could be combined with other techniques, such as cognitive behavior therapy (CBT) or act commitment therapy (ACT). Segal et al. are one of earliest scholars who combined CBT principles with mindfulness—Mindfulness Based Cognitive Therapy (MBCT)—with the aim to “change one’s awareness of and relationship to thoughts and emotions” and, hence, reduce the associations between negative automatic thinking and feelings of sadness and unease [10]. More recently, web-based MBIs are being increasingly used for better accessibility, among other reasons, with promising results to promote mental health and wellbeing [11,12,13]. In 2016, a meta-analysis of earlier 15 clinical trials using web-based MBIs was conducted with a focus on mindfulness-based self-regulation (MBSR), MBCT, and ACT interventions [14]. The authors found an effect size of 0.51 for stress reduction and small but significant effects sizes, ranging from 0.29 to 0.22, for anxiety, depression and well-being. However, the impact of web-based MBIs on the quality of life was not examined, which is a significant knowledge gap given growing adoption of web-based MBIs across diverse samples.
World Health Organization defines quality of life as “an individual's perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns” (pg 11) [15]. The evaluation of quality of life is particularly relevant for young adults as they experience many life transitions and in a relatively short period of time. Their new learnings, growing social relationships, and varying expectations from academic institutions and/or workplaces are likely to influence their perceived quality of life. There is growing body of work on students’ quality of life and how it varies with factors like age, gender, socioeconomic status, living away from family, commuting, year of college, exams stress, academic performance, grade point average (GPA), number of hours of classes, everyday life insecurity, mental health problems, burnout, religious coping, and social support from family, friends and significant others [16,17,18,19,20]. However, web-based MBIs with a focus on students and quality of life are just emerging. Addressing this knowledge gap is imperative given that web-based MBIs are better suited to engage students due to technological comfort of Gen Z (or millennials) and their preference for web-based services than in-person services [21]. A handful of studies with students, examining the influence of mindfulness on quality of life, report mixed results. For example, a 2018 survey of Italian students reported significant positive correlations between mindfulness and quality of life [22]. In 2016, a peer-led mindfulness-based program among medical students in New Zealand found some improvement in the quality of life but it was not statistically significant [23]. In 2020, a randomized controlled trial (RCT) in Brazil on teaching mindfulness techniques among medical students did not find significant gains in the quality of life in the intervention group compared to the control group [24]. Indeed, there is a need to advance scholarly understanding on web-based MBIs among students for their impact on the quality of life.
The specific objective of the current study was to test the hypothesis: would the use of a web-based 8-week long mindfulness and CBT informed intervention—Mindfulness Virtual Community (MVC)—improve the quality of life of undergraduate students? The earlier related work reports on the MVC effectiveness in a 4-arm pilot RCT [25] and a 2-arm RCT [26, 27] with main focus on the mental health outcomes.
Methods
In 2018 September–November, we conducted a 2-arm RCT to examine the effectiveness of the MVC web-based intervention for students enrolled in undergraduate programs at a Canadian university in Toronto, Ontario. The intervention’s statistically significant impact on reducing symptoms of anxiety and depression, primary outcome, is reported elsewhere [26, 27]. This paper reports on the intervention’s impact for the quality of life measured by the Quality of Life Scale [28]. The trial was guided by the CONSORT guidelines for non-pharmacological interventions [29] and informed by the reporting guidelines for web-based and online interventions [30]. The research ethics approval was obtained from York University, Canada (Certificate No.: e216-345). All methods were performed in accordance with the relevant ethical guidelines and regulations including the Declarations of Helsinki.
Eligibility and recruitment
The eligibility criteria included being an actively enrolled undergraduate student, 18 years or more in age with English language written/oral fluency and a self-report of high confidence in the study completion. The exclusion criteria were substance abuse or psychotic behavior that respondents perceived as interfering in their routine life during the last month, and were applied once interested students approached the study staff for more details. The recruitment entailed multiple strategies, such as posting study posters in high traffic areas of campus, announcements in classes with permission of professors, and study invitations circulated through electronic mailing list of students’ associations. The incentive of CAD $50 or 2% in course grade (a standard followed at the university) were offered. All participants provided informed written consent and received an information sheet about health and social care programs in the community and on the campus. Participant access to internet and laptop or computers or smartphone was assumed as a non-issue based on focus groups conducted before the trial [31, 32]; these amenities are also available free of cost throughout the campus.
Randomization
The randomization scheme was 1:1 block randomization and generated by an off-site biostatistician. The sequence for allocation of participants was concealed in opaque envelopes which were sequentially numbered and opened by the research assistant (RA) in that order [33]. Once an eligible student provided informed consent, the envelopes were opened by the RA and participant students were then randomized to the MVC or the waitlist control group. These procedures ensured that both RA and participants were blind until the allocation was made. To login the MVC intervention, participants were provided with a unique ID and a temporary password; they changed the password after first login. Participants in both groups completed online questionnaire at the start (T1) and at 8-weeks (T2). Once T2 survey was completed, participants in the waitlist group received access to all of the video-based modules simultaneously, but video conferences and discussion forum were not offered nor were further data collected; hence we refer to this group as control group from here onwards.
Mindfulness Virtual Community (MVC) Intervention
The MVC intervention (Fig. 1) was 8-week long and offered three components: (1) 12 mental health modules in video format; (2) 3 discussion boards for anonymous exchange on depression, anxiety, and stress; and (3) a 20-min live videoconference led by a trained moderator (master’s in psychology) whereby participants remained anonymous while discussing topics covered in the modules.
The Design of Web-based Mindfulness Virtual Community. a First published as “Effectiveness of an 8-week web-based mindfulness virtual community intervention for university students on symptoms of stress, anxiety, and depression: randomized controlled trial,” by El Morr C, Ritvo P, Ahmad F, Moineddin R, Team MVC, 2020, JMIR Mental Health, 7(7):e18595, p. 3. (https://mental.jmir.org/2020/7/e18595/) CC BY 4.0
Each of the video-based modules consisted of two parts: an educational section; and a mindfulness-practice section. Each of these two parts of a module focused on a specific topic (see the 12 topics described below) and were available in female or male voice and high or low resolution (i.e., 8 versions for each module). The topics of modules drew from our earlier work where focus groups were conducted with undergraduate students to develop the intervention through a student-centered approach [31, 32]. One of the team members (PR) with clinical experience developed the module scripts and audio recordings by combining principles from mindfulness and CBT. The selection of images was a collaborative work (PR, CEM, FA). The video-based modules were then tested in a pilot randomized trial and found efficacious [25].
The topics of the final modules were: Overcoming stress, anxiety, and depression; Mindfulness and being a student; Mindfulness for better sleep; Thriving in a fast-changing world; Healthy intimacy; De-stigmatization; No more procrastination; Pain reduction and mindfulness; Healthy body image; Healthier eating; Overcoming trauma; and Relationships with family and friends. On average, the educational videos were 5:14 min long and the mindfulness-practice videos 7:79 min. The modules were released at a regular interval during the 8-week intervention period. Once a module was released, it remained open for the remaining study period. The research staff sent email reminders to the participants before the release of a module and the live videoconference. They were also encouraged to access the opened modules as often as they desired.
The 20-min videoconferences were offered twice each week with three evening sessions each time between 8:00 and 9:30 pm. The moderator role drew from our pilot trial [25]. The moderator led the live discussions and moderated discussion board messages. On weekly basis, the moderator met the team clinician (PR) to discuss and optimize student engagement during videoconference, and submitted written reports.
Our team partnered with the industry partner, ForaHealthyme Inc, for the MVC platform development. The main page of the MVC platform showed only names of the university and the IT partner. The accessibility features of the MVC platform were tailored for the two types of users: students and moderator. Once logged in, the students were able to access video-based modules; posts on discussion board; notify the moderator for problematic posts on the discussion board; book videoconference session through calendar; join videoconference room with default set as “off” for camera and microphone; privately chat with the moderator during live videoconference; and access resource page with information of health and social programs. In addition to all options available to the students, the moderator was able to delete unsuitable messages from the discussion board, add session dates and times for videoconferencing, start a live videoconference (camera was turned on by default), and respond privately to chat messages from the students. For the study period, the intervention content and structure remained unchanged.
Measurement
The quality of life was measured using the 16-item Quality of Life Scale (QOLS) [28]. This scale captures physical/material well-being, relationships with other people, social/civic activities, personal development, recreation, and independence [34]. The study participants rated each item on a 7-point Likert scale with response options of delighted = 7, pleased = 6, mostly satisfied = 5, mixed = 4, mostly dissatisfied = 3, unhappy = 2, and terrible = 1. The total score was calculated by summing the item scores; the score ranges from 16 to 112. Previous studies show that QOLS is a reliable and valid instrument. For example, Burckhardt in 1989 reported the Cronbach alpha of 0.89 for its internal consistency and test–retest scores in the range of 0.76 to 0.84 over 6- to 3-week intervals [35]. Burckhardt has also reported its discriminant validity with higher scores found in painful chronic condition than in more stable chronic conditions [36]. In the current study, the internal consistency score of QOLS was Cronbach alpha of 0.99 at the baseline. The outcomes of depression, anxiety and perceived stress were measured using validated and reliable scales: the 9-item Patient Health Questionnaire or PHQ-9 for depression symptoms [37], 21-item Beck Anxiety Inventory or BAI-21 for anxiety symptoms [38], and 10-item Perceives Stress Scale, or PSS-10 for global stress [39]. The Five Facets Mindfulness Questionnaire Short Form (FFMQ-SF) was used to measure the mindfulness [40]. Information on participants’ sociodemographic characteristics was also collected.
Statistical analysis
The estimation of the sample size was based on the standardized effect size of 0.5 or larger in the primary outcomes of mental health. With the power set at 80% and type I error as 5%, the sample size was estimated as 63 for each group in the 2-arm trial. The attrition rate was estimated as 20% (n = 16) and, thus, we aimed to recruit 80 participants for each group. On completion of data collection, we used descriptive statistics (mean, frequencies) to present a summary of the sample characteristics. The outcome analysis for the QOLS was intention-to-treat (ITT) including data of the entire sample (n = 159) who were randomized at the start of the study. The missing values were imputed using multiple imputation with multivariate regression. To analyze effectiveness of the intervention, we used generalized estimating equation (GEE) method with an AR(1) covariance structure. In Model 1, the effect of intervention at 8-week time (T2) was examined on the dependent variable of QOLS. In Model 2, potential covariates were added to Model 1. The adjusted potential covariates were gender, age, country of birth, first language, ethnicity, relationships, self-rated health, access to private mental health counselling, paid work, unpaid work, and engagement in vigorous physical exercise. For consistency and ease of interpretation, the covariates were same as in previously reported analysis for mental health outcomes. In addition to ITT, we also executed the GEE analyses using the same model but with complete-case approach (n = 147) where missing values were not imputed. We report both ITT and complete-cases analyses. All analyses was conducted using the Stata software [41].
Results
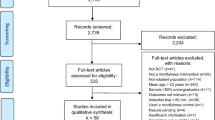
Out of 164 students assessed for eligibility, 4 were excluded and 160 randomized to the intervention (n = 80) or control (n = 80) groups. The recruitment flow and reasons for exclusion are provided in Fig. 2. One student was excluded after randomization as he/she was enrolled in graduate studies. 159 students completed the baseline survey and, thus, are included in the analysis.
Participant characteristics
The characteristics of participants at the baseline are presented in Table 1. There were 125 (78.6%) females and 32 (20.1%) males with overall mean age of 22.6 years (SD 6.1). In the total sample, 91 (57.2%) were born in Canada and 68 (42.8%) outside Canada; the majority (58.5%) reported English as the first language spoken at home. The most common ethnicity was South Asian (27.7%) followed by White (20.1%), Black (14.5%) and Chinese (9.4%). Most of the participants were single (64.1%) and rated their general health as ‘very good’ to ‘excellent’ (42.2%). The baseline score for perceived stress measured by PSS was 22.01 (SD 5.32) while the PHQ-9 score for depression was 9.91 (SD 6.22), and BAI-21 for anxiety was 17.56 (SD 12.17). The baseline score for FFMQ-SF was 72.62 (SD 12.06). The MVC intervention and control groups were similar at the baseline except for mean weekly hours of unpaid work, which was 3.06 h (SD 0.52) for the control group and 1.75 h (SD 0.30) for the intervention group (t = 2.2, df 157, p = 0.03).
Quality of life, socio-demographics and mental health
The baseline score of QOLS was 79.42 (SD 15.95) for the whole sample. On examining its.relationship with the sociodemographic characteristics, significant associations were found for the self-reported health (F = 21.61, p < 0.001), access to mental health services (F = 6.64, p = 0.01), engagement in weekly vigorous exercise (F = 10.81, p = 0.001), and number of hours of voluntary unpaid work (r = 0.15, p = 0.007). The score of QOLS also had a strong negative correlation with PSS stress score (r = -0.37, p < 0.001), anxiety BAI-21 score (r = -0.48, p < 0.001), depression PHQ-9 score (r = -0.56, p < 0.001). The QOLS score has a positive correlation with FFMQ-SF total score at the baseline (r = 0.54, p < 0.001).
Quality of life score changes
Table 2 compares the QOLS mean scores of the control and interventions groups at baselines. (T1) and after 8 weeks (T2). QOLS was normally distributed (Shapiro–Wilk test p = 0.41). There was no statistically significant difference in QOLS scores between the intervention and control groups at baseline (81.33, SD 16.82 vs. 77.53, SD 14.91, p = 0.13). Between-group comparison showed a significantly higher score at T2 for the intervention group compared to the control group (81.64, SD 14.63 vs. 72.9, SD 17.26, p < 0.001); also see Fig. 3. Within-group changes showed significant reduction of QOLS mean score in the control group by 4.63 points (p = 0.005), and a small increase of scores (0.31 points) in the intervention group which was not statistically significant.
Effect of the intervention
Using the GEE, the unadjusted and adjusted effects of the MVC intervention on QOLS scores are shown in Table 3 using the intention to treat and imputation of missing values (n = 159). In the unadjusted model, there were significant score change for time T2 (β = -4.63, p = 0.003), intervention group (β = 8.75, p = 0.001) and interaction between the two (β = -4.94, p = 0.03). The results were similar when the model was adjusted for potential covariates; time T2 (β = -4.63, p = 0.003), intervention group (β = 7.87, p = 0.001) and interaction between the two (β = -4.94, p = 0.03). Of the factors included in the model, only self-rated health showed significant effect (β = -5.73, p < 0.001).
When we ran the same models on the observations having complete data (n = 147) (i.e., without imputing missing values), the results were similar as shown in Table 4 with similar effects and significance levels. The only difference was that in this case, an additional factor (unpaid work), which was close to significance in the previous model (p = 0.06), became statistically significant (β = 0.59, p = 0.04).
Discussion
Given the applicability of the quality of life across various health conditions, we believe the findings of the reported RCT on the students’ quality of life after use of the Mindfulness Virtual Community (MVC) would make meaningful contributions towards development of support programs for students’ global health. This study is especially timely as student challenges have exacerbated with the onset of COVID-19 pandemic [42], calling for new ways to support their overall well-being.
The study findings show partial support for the tested hypothesis. On one side, student participants in the intervention group had a higher quality of life compared to those in the control group at the post-intervention time, and the difference was statistically significant. On the other, the pre- and post-intervention scores were almost the same in the intervention group while the control group had a statistically significant decline. Its notable that the post-intervention measurement coincided with the student preparation time for the midterm exams. In this context, it can be inferred the intervention supported the participant students in maintaining their quality of life despite the exam period stress while those in the control group experienced the usual decline. This possibility is supported by recent research reporting the mediating role of mindfulness nonreactivity facet on the effect of anxiety over exam performance among college students [43] while the quality of life score in our sample at the baseline was negatively correlated with anxiety scores. Another possible reason for not being able to find the pre-post gains in the QOLS score could be our sample of undergraduate students with chronically low quality of life given their multiple challenges at the stage of life transition to adulthood [44, 45]. Participants in the study had a baseline total score of 79.42 for the QOLS scale. This score is lower than the estimation by Burckhardt and Anderson who stated in 2003, after examining the scale use across various published studies, “Average total score for healthy populations is about 90” [46]. A similar low score of 74 was noted in the pilot trial of MVC intervention with 112 undergraduate students from the same university [25]. In another study of 2015 with nursing students in Norway the score was 84 for the QOLS total sum [47]. Therefore, future study with a larger sample of undergraduate students would be needed to assess the MVC impact beyond being protective for the students’ quality of life as found in our study. We have also previously reported the effectiveness of MVC in significantly improving the symptoms of depression and anxiety at the post-intervention measurement [26]. Taken together, the findings show that web-based MVC intervention is effective in supporting both the overall quality of life and mental health of undergraduate students. There are multiple practical implications of these results. For instance, web-based interventions are less costly than face-to-face counselling and overcome access barriers like commute, time and worries about stigma [48, 49] while youth is technologically savvy and find such programs easy to use. Further, existing research shows that students’ calmer view of present improves their task focus, study habits, exam performance, and organization [43, 50,51,52] and some report improvement in students’ working memory after mindfulness programs [53]. Thus, a wide scale adoption of effective web-based MBI like MVC could benefit both the students and the academic institutions through students’ better quality of life, mental health, and academic performance.
The findings of the study also offer insights on a multitude of factors that could potentially support students’ overall quality of life during the university years. For instance, the QOLS score was significantly associated with participants’ engagement in weekly vigorous exercise, consistent with prior research with students [19, 54], and the number of hours in volunteer work. These results emphasize the importance of having effective student-engagement activities, on campus and outside campus, for their better quality of life. The possible underlying mechanism could be the enhancement of self-esteem and confidence [55], which needs further research with university students. A counter argument could be made that those working more hours may have less quality of life due to less spare time. Studies comparing working and non-working students could enhance further understanding. The QOLS score was also positively associated with students’ access to mental health services. In our best knowledge, this association has not been previously reported in QOLS studies with students and signify the need to expand the mental health coverage for students. Although Canada has a government funded universal health care program, the access to mental health counselling is outside the scope of this universal program. Students have limited access to counselling under the student insurance plans. Another notable finding of the current study is the negative association of the QOLS with stress, depression and/or anxiety. Similar results have been reported in other studies with students [18, 19, 47]. These findings emphasize how mental health is a key determinant of one’s overall quality of life. Given the growing rates of depression and anxiety among students [44, 45], programs to support students’ mental health would go a long way by contributing to their overall quality of life. Effective web-based MBIs like MVC offer an important alternative to meet the needs of university students.
The results should be interpreted in light of the study’s strengths and limitations. A strength of the study is high response rate (160/164) out of those who approached the research staff. We also report both intention-to-treat and complete-case analysis for the ease of interpretation. Importantly, the results of GEE are similar for both of these analyses. A study limitation is that complete blinding of the participants was not possible as those in the intervention group were the users of the web-based MVC program. However, the participants and the recruiters were kept blind until they opened the envelopes with the allocation assignment. Another limitation is the post-intervention measurement at 8 weeks which was immediately after the intervention delivery. The trial sample size estimation was geared towards testing the impact of intervention on mental health outcomes. Future research with a larger sample and a longer follow-up is recommended to comprehensively examine the impact of the MVC on students’ quality of life. The participant sample had more female than male students though this trend has been noted in other studies with university students [56, 57]. Finally, the study was conducted in a large university located in a metropolitan city, which warrants caution in interpretation of the results for other institutions.
Conclusion
This study is the first, in our best knowledge, to report the impact of web-based CBT-mindfulness program on the quality of life of undergraduate students. The 8-week-long web-based Mindfulness Virtual Community was effective in supporting the students’ quality of life in the studied sample. Our study also documents the association between the QOLS score and students’ access to mental health services, which offers insights for policymaking geared towards post-secondary students. A multi-site study with multiple institutions and longer follow-up would enhance further understanding and transferability of results.
Availability of data and materials
The corresponding author (CE) could be approached to access the trial protocol and/or related dataset on reasonable request.
References
Kabat-Zinn J. An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: theoretical considerations and preliminary results. Gen Hosp Psychiatry. 1982;4(1):33–47.
Davidson RJ, Kabat-Zinn J, Schumacher J, Rosenkranz M, Muller D, Santorelli SF, et al. Alterations in brain and immune function produced by mindfulness meditation. Psychosom Med. 2003;65(4):564–70.
Kabat-Zinn J. Mindfulness-based interventions in context: past, present, and future. Clin Psychol Sci Pract. 2003;10(2):144–56.
Hölzel BK, Hoge EA, Greve DN, Gard T, Creswell JD, Brown KW, et al. Neural mechanisms of symptom improvements in generalized anxiety disorder following mindfulness training. Neuroimage Clin. 2013;2:448–58.
Lazar SW, Kerr CE, Wasserman RH, Gray JR, Greve DN, Treadway MT, et al. Meditation experience is associated with increased cortical thickness. NeuroReport. 2005;16(17):1893–7.
Robins CJ, Keng SL, Ekblad AG, Brantley JG. Effects of mindfulness-based stress reduction on emotional experience and expression: a randomized controlled trial. J Clin Psychol. 2012;68(1):117–31.
Garland EL, Geschwind N, Peeters F, Wichers M. Mindfulness training promotes upward spirals of positive affect and cognition: multilevel and autoregressive latent trajectory modeling analyses. Front Psychol. 2015;6:15.
de Vibe M, Bjørndal A, Fattah S, Dyrdal GM, Halland E, Tanner-Smith EE. Mindfulness-based stress reduction (MBSR) for improving health, quality of life and social functioning in adults: a systematic review and meta-analysis. Campbell Syst Rev. 2017;13(1):1–264.
Creswell JD. Mindfulness interventions. Annu Rev Psychol. 2017;68:491–516.
Segal ZV, Williams JM, Teasdale JD. Mindfulness-Based Cognitive Therapy for depression: a new approach to preventing relapse. New York, NY: Guilford Press; 2002.
Lappalainen P, Langrial S, Oinas-Kukkonen H, Tolvanen A, Lappalainen R. Web-based acceptance and commitment therapy for depressive symptoms with minimal support: a randomized controlled trial. Behav Modif. 2015;39(6):805–34.
Mak WW, Chio FH, Chan AT, Lui WW, Wu EK. The efficacy of internet-based mindfulness training and cognitive-behavioral training with telephone support in the enhancement of mental health among college students and young working adults: randomized controlled trial. J Med Internet Res. 2017;19(3):e84.
Rasanen P, Lappalainen P, Muotka J, Tolvanen A, Lappalainen R. An online guided ACT intervention for enhancing the psychological wellbeing of university students: a randomized controlled clinical trial. Behav Res Ther. 2016;78:30–42.
Spijkerman MP, Pots WT, Bohlmeijer ET. Effectiveness of online mindfulness-based interventions in improving mental health: a review and meta-analysis of randomised controlled trials. Clin Psychol Rev. 2016;45:102–14.
World Health Organization (WHO). The World Health Organization Quality of Life (WHOQOL). Geneva: World Health Organization (WHO); 1998. Accessed 16 Nov 2021.
Ben Nasrallah C, Ghammem R, Mihoubi A, Ben Rejeb M. Factors associated with the quality of life among paramedical students in Sousse governorate. Eur J Public Health. 2021;31(Supplement_3):iii503.
Chattu VK, Sahu PK, Seedial N, Seecharan G, Seepersad A, Seunarine M, et al. An exploratory study of quality of life and its relationship with academic performance among students in medical and other health professions. Med Sci (Basel). 2020;8(2):e10.
Leong Bin Abdullah MFI, Mansor NS NS, Mohamad MA MA, Teoh SH SH. Quality of life and associated factors among university students during the COVID-19 pandemic: a cross-sectional study. BMJ Open. 2021;11(10):e048446.
Solis AC, Lotufo-Neto F. Predictors of quality of life in Brazilian medical students: a systematic review and meta-analysis. Braz J Psychiatry. 2019;41(6):556–67.
Grande RAN, Berdida DJE, Maniago JD, Ablao JN, Llaguno MBB, Manood EG. Predictors of quality of life of nursing internship students from five Saudi universities. J Taibah Univ Med Sci. 2021;16(5):747–54.
Rickwood DJ, Mazzer KR, Telford NR. Social influences on seeking help from mental health services, in-person and online, during adolescence and young adulthood. BMC Psychiatry. 2015;15:40.
Pagnini F, Bercovitz KE, Phillips D. Langerian mindfulness, quality of life and psychological symptoms in a sample of Italian students. Health Qual Life Outcomes. 2018;16(1):29.
Moir F, Henning M, Hassed C, Moyes SA, Elley CR. A Peer-support and mindfulness program to improve the mental health of medical students. Teach Learn Med. 2016;28(3):293–302.
Damião Neto A, Lucchetti ALG, da Silva EO, Lucchetti G. Effects of a required large-group mindfulness meditation course on first-year medical students’ mental health and quality of life: a randomized controlled trial. J Gen Intern Med. 2020;35(3):672–8.
Ahmad F, El Morr C, Ritvo P, Othman N, Moineddin R, Team M. An eight-week, web-based mindfulness virtual community intervention for students’ mental health: randomized controlled trial. JMIR Ment Health. 2020;7(2):e15520.
El Morr C, Ritvo P, Ahmad F, Moineddin R, Team MVC. Effectiveness of an 8-week web-based mindfulness virtual community intervention for university students on symptoms of stress, anxiety, and depression: randomized controlled trial. JMIR Ment Health. 2020;7(7):e18595.
Ritvo P, Ahmad F, El Morr C, Pirbaglou M, Moineddin R, Team MVC. A mindfulness-based intervention for student depression, anxiety, and stress: randomized controlled trial. JMIR Ment Health. 2021;8(1):e23491.
Flanagan JC. Measurement of quality of life: current state of the art. Arch Phys Med Rehabil. 1982;63(2):56–9.
Boutron I, Altman DG, Moher D, Schulz KF, Ravaud P, Group CN. CONSORT statement for randomized trials of nonpharmacologic treatments: A 2017 update and a CONSORT extension for nonpharmacologic trial abstracts. Ann Intern Med. 2017;167(1):40–7.
Eysenbach G, Group C-E. CONSORT-EHEALTH: improving and standardizing evaluation reports of Web-based and mobile health interventions. J Med Internet Res. 2011;13(4):e126.
Ahmad F, El Morr C, Ritvo P. Mindfulness virtual community for student mental health. Toronto: Center for Innovation in Campus Health Conference; 2018.
El Morr C, Maule C, Ashfaq I, Ritvo P, Ahmad F. A student-centered mental health virtual community needs and features: a focus group study. Stud Health Technol Inform. 2017;234:104–8.
Doig GS, Simpson F. Randomization and allocation concealment: a practical guide for researchers. J Crit Care. 2005;20(2):187–91 (discussion 91-3).
Burckhardt CS, Anderson KL, Archenholtz B, Hägg O. The Flanagan Quality Of Life Scale: evidence of construct validity. Health Qual Life Outcomes. 2003;1:59.
Burckhardt CS, Woods SL, Schultz AA, Ziebarth DM. Quality of life of adults with chronic illness: a psychometric study. Res Nurs Health. 1989;12(6):347–54.
Burckhardt CS, Clark SR, Bennett RM. Fibromyalgia and quality of life: a comparative analysis. J Rheumatol. 1993;20(3):475–9.
Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders Patient Health Questionnaire. JAMA. 1999;282(18):1737–44.
Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56(6):893–7.
Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–96.
Bohlmeijer E, ten Klooster PM, Fledderus M, Veehof M, Baer R. Psychometric properties of the five facet mindfulness questionnaire in depressed adults and development of a short form. Assessment. 2011;18(3):308–20.
StataCorp. Stata Statistical Software:Release 13. College Station: StataCorp LP; 2013.
Elharake JA, Akbar F, Malik AA, Gilliam W, Omer SB. Mental health impact of COVID-19 among children and college students: a systematic review. Child Psychiatry Hum Dev. 2022;54(3):913–25.
López-Navarro E, Giorgetti D, Errasti J, Al-Halabí S. Does dispositional mindfulness mediate the relationship between anxiety and exam performance? Revista de Investigación en Educación. 2020;18(3):324–31.
Hop Wo NK, Anderson KK, Wylie L, MacDougall A. The prevalence of distress, depression, anxiety, and substance use issues among Indigenous post-secondary students in Canada. Transcult Psychiatry. 2020;57(2):263–74.
Turner JC, Keller A. College Health Surveillance Network: Epidemiology and health care utilization of college students at US 4-year universities. J Am Coll Health. 2015;63(8):530–8.
Burckhardt CS, Anderson KL. The Quality of Life Scale (QOLS): reliability, validity, and utilization. Health Qual Life Outcomes. 2003;1:60.
Kleiveland B, Natvig GK, Jepsen R. Stress, sense of coherence and quality of life among Norwegian nurse students after a period of clinical practice. PeerJ. 2015;3: e1286.
Sareen J, Jagdeo A, Cox BJ, Clara I, ten Have M, Belik SL, et al. Perceived barriers to mental health service utilization in the United States, Ontario, and the Netherlands. Psychiatr Serv. 2007;58(3):357–64.
Downs N, Galles E, Skehan B, Lipson SK. Be true to our schools-models of care in college mental health. Curr Psychiatry Rep. 2018;20(9):72.
Broderick PC, Jennings PA. Mindfulness for adolescents: a promising approach to supporting emotion regulation and preventing risky behavior. New Dir Youth Dev. 2012;2012(136):111–26, 11.
Docksai R. A mindful approach to learning: new research shows potential for "mindfulness training" to boost student productivity. The Free Library. 2013. 8–10. Retrieved April 2, 2022 from https://www.thefreelibrary.com/A+mindful+approach+to+learning%3A+new+research+shows+potential+for...-a0339734724.
Rodgers L. A calmer happier child. Scholastic Parent Child. 2014;21(6):60.
Quach D, Jastrowski Mano KE, Alexander K. A randomized controlled trial examining the effect of mindfulness meditation on working memory capacity in adolescents. J Adolesc Health. 2016;58(5):489–96.
Dong Fang J-D, Teng P-C, Wang F-J. The impact of physical education classes on health and quality of life during the COVID-19. Appl Sci. 2021;11(11):8813.
Schonert-Reichl K, Lawlor M. The effects of a mindfulness-based education program on pre- and early adolescents’ well-being and social and emotional competence. Mindfulness. 2010;1(3):137–51.
O’Driscoll M, Byrne S, Mc Gillicuddy A, Lambert S, Sahm LJ. The effects of mindfulness-based interventions for health and social care undergraduate students - a systematic review of the literature. Psychol Health Med. 2017;22(7):851–65.
van der Riet P, Levett-Jones T, Aquino-Russell C. The effectiveness of mindfulness meditation for nurses and nursing students: an integrated literature review. Nurse Educ Today. 2018;65:201–11.
Acknowledgements
We are highly appreciative of all the students who volunteered in the study and to the ForaHealthyMe.com Inc. as our industry partner. We thank Dr. Nasih Othman for assistance in analysis.
MVC Team (alphabetical order by last name)
Sahir Abbas1, Farah Ahmad1, Yvonne Bohr2, Christo El Morr1, Manuela Ferrari3, Wai Lun Alan Fung4, Louise Hartley2, Amin Mawani5, Kwame McKenzie6, Jan E. Odai1, Paul Ritvo2
1. School of Health Policy and Management, York University, Toronto, Canada
2. Dept. of Psychology, York University, Toronto, Canada
3. The Douglas Research Centre, McGill University, Montreal, Canada
4. Tyndale University College, Toronto, Canada
5. Schulich School of Business, York University, Toronto, Canada
6. Centre Addiction & Mental Health, Toronto, Canada
Funding
The project was funded by the Grant number EH1- 143553, which was awarded by the Canadian Institutes for Health Research (CIHR) eHealth Innovations Partnership Program Grant (eHIPP) to CE (nominated), FA, and PR as principal investigators. The funding body had no role in the study design, data collection, analysis and interpretation of the results.
Author information
Authors and Affiliations
Consortia
Contributions
FA, CE, and PR contributed equally in the design of study and in receiving funds; they agree to be accountable for all aspects of the submitted paper. The development of modules was led by PR who provided written content and voice. The first draft of paper was prepared by FA. All authors provided critical feedback and revised it. The MVC Team includes (alphabetically): Sahir Abbas, BSc; Yvonne Bohr, PhD; Manuela Ferrari, PhD; Wai Lun Alan Fung MD, ScD, FRCPC; Louise Hartley, PhD; Amin Mawani, PhD; Kwame McKenzie, MD, FRCPC; and Jan E. Odai, BA – they made contribution to the project in many ways for data collection, analysis and writeup, and approve the submitted paper.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The research ethics approval for the trial was obtained from the Human Participants Review Committee of York University Research Ethics Board, Canada (Certificate No.: e216-345) and conforms to the standards of the Canadian Tri-Council Research Ethics guidelines. All participants provided written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ahmad, F., El Morr, C., Ritvo, P. et al. Examining the impact of web-based mindfulness on undergraduate student’s quality of life: a randomized controlled trial. BMC Digit Health 1, 22 (2023). https://doi.org/10.1186/s44247-023-00023-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s44247-023-00023-2