Abstract
Background
Reversibility measured by spirometry in chronic obstructive pulmonary disease (COPD) is defined as an increase in forced expiratory volume in first second (FEV1) that is both more than 12% and 200 mL above the pre-bronchodilator value in response to inhaled bronchodilators. FEV1 only may not fully reverberate the changes caused by reduction in air trapping or hyperinflation. To date, the studies that examined the effect of inhaled bronchodilators (BD) on residual volume (RV) and total lung capacity (TLC) are limited. This study was carried out to assess the differences between flow and volume responses after bronchodilator reversibility testing in patients with different COPD GOLD stages (GOLD stage I to stage IV). Spirometry and whole body plethysmography were done before and 15 min after inhalation of 400 μg salbutamol.
Results
Majority (53.3%) of cases were volume responders, 18.7% were flow responders, 20% were flow and volume responders, and 8% were non responders. Significant increase in Δ FEV1% was found in 15% of cases while 55% showed a significant increase in Δ FVC (P= < 0.001). Mean difference of Δ FVC (L) post BD was significantly increased with advancing GOLD stage (P= 0.03). A cutoff point > 20% for Δ RV% had 70% sensitivity and 60% specificity and > 12% for Δ TLC% showed 90% sensitivity and 45% specificity for prediction of clinically significant response to BD based on FEV1. A cutoff point > 18% for Δ RV% had 78% sensitivity and 29% specificity and > 14% for Δ TLC% had 50% sensitivity and 70% specificity for prediction of clinically significant response to BD based on FVC.
Conclusion
ΔFEV1 underestimates the true effect of bronchodilators with advancing GOLD stage. Measurement of lung volumes in addition to the standard spirometric indices is recommended when determining bronchodilator response in COPD patients.
Similar content being viewed by others
Background
Spirometry is the most commonly used method for assessment of airflow limitation in COPD. Reversibility in COPD is defined by an improvement in FEV1 that is both greater than 0.2 L and 12% above the pre-bronchodilator (pre-BD) FEV1 value [1]. Forced expiratory volume in one second (FEV1) is the parameter used by the Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines.
Many studies relied on FEV1 only for assessment of reversibility [2,3,4,5,6,7,8] and others proposed that forced vital capacity (FVC) is an underutilized measure of reversibility [9].
FEV1 and FVC are not the only measured parameters that change in response to bronchodilators inhalation during reversibility testing. Lung volumes have been found to respond to bronchodilators inhalation independent of FEV1 [10,11,12,13,14,15,16,17].
Lung volumes are potentially useful parameters in detecting response to inhaled bronchodilators, yet they are not used frequently despite having important clinical implications [10].
Static hyperinflation is considered a risk factor for mortality [18]. Dynamic hyperinflation increases work of breathing [19] and has reversibility parameters which correlate with the inspiratory capacity (IC) but not with the FEV1 [15, 20].
There are a significant number of patients whose total lung capacity (TLC) and residual volumes (RV) exhibit bronchodilator-responsiveness even if their FEV1 or FVC do not.
This study aimed to assess the differences between flow and volume responses after bronchodilator reversibility testing in patients with different COPD GOLD stages (GOLD stage I to stage IV).
Methods
This prospective cohort study included 300 patients (228 males and 72 females) who presented to the outpatient clinic during the period from May 2018 to May 2020. Informed consent was taken from all patients who participated in the study. This study was approved by the research ethics committee of the Faculty of Medicine.
Inclusion criteria
The diagnosis of COPD was established by clinical assessment and spirometric tests according to the GOLD 2017 guidelines [1].
-
Patients diagnosed as COPD according to GOLD 2017 guidelines (post bronchodilator FEV1″/FVC″ ˂ 0.70 by spirometry [1]
-
Age ˃40 years
Exclusion criteria
-
Current infective exacerbation of COPD
-
Patients with current or previous clinical history or investigation suggestive of bronchial asthma
-
Decompensated cor-pulmonale
-
Respiratory failure
-
Contraindication to spirometry and body plethysmography procedure [21]:
*Recent myocardial infarction (1 month), ophthalmic surgery, abdominal/thoracic surgery, pneumothorax, or pulmonary embolism, stroke
*Presence of hemoptysis
*Thoracic, aortic, cerebral aneurysm
*Uncontrolled hypertension
All patients were subjected to the following:
-
1.
Assessment of eligibility for entry to the study was determined by full clinical history taking including smoking index [22] and physical examination.
-
2.
Modified Medical Research Council (m MRC) scale for rating patients’ dyspnea score.
-
3.
Spirometry (Cosmed SrL, Quark PFTs ergo, P/N Co9035 – 12-99
-
4.
made in Italy) and whole body plethysmography (D 97723; ZAN300, Oberthulba, Germany)
Patients were asked to omit short-acting inhaled bronchodilators for at least 8 h, and long acting beta-agonists for at least 12 h. The technique of spirometry and whole body plethysmography were demonstrated and a trial run of these tests were performed until reasonable technique and consistent reproducible readings were obtained.
3. Reversibility test was done by inhalation of short-acting B2-agonist (400 μg salbutamol). Spirometry and whole body plethysmography were performed again 15 min after the bronchodilator (BD) was inhaled. The presence of a post-BD FEV1/FVC ratio < 0.7 confirms the presence of persistent airflow limitation. Bronchodilator response was expressed as a percentage and an absolute change in milliliters of the baseline values. FEV1 (flow responders) and FVC (volume responders) responsiveness were defined by >12% and >200 mL improvement of baseline values [23, 24].
4. GOLD staging. Patients were classified according to the severity of air flow obstruction into:
GOLD I: FEV1 ≥ 80% of predicted
GOLD II: FEV1 ≤ 50-< 80% of predicted
GOLD III: FEV1 ≤ 30-< 50% of predicted
GOLD IV: FEV1 < 30% of predicted
Statistical analysis
Data was collected and analyzed using SPSS (Statistical Package for the Social Science, version 20, IBM, and Armonk, New York). Continuous data was expressed in form of mean ± SD and range while nominal data was expressed in the form of frequency (percentage).
Chi2 test was used to compare the nominal data of different groups while continuous data of two groups were compared with Student t test, and ANOVA test was used in case of more than two groups. Correlation of mean differences of FEV1 and FVC with RV and TLC was assessed by Pearson correlation. Level of confidence was kept at 95% and P value was significant if < 0.05.
Results
Baseline data of enrolled patients
The current study included 300 patients with COPD. Mean age was 61.98 ± 10.43 years. Majority (76%) of enrolled patients were males. Two hundred and ninety-four (83%) patients were employed. As regarding smoking index, it was noticed that 6 (2%), 9 (3%), and 213 (71%) patients were mild, moderate, and heavy smokers, respectively. Based on GOLD staging of COPD, stages I, II, III, and IV present in 3 (1%), 36 (12%), 129 (43%), and 132 (44%) patients, respectively (Table 1).
Spirometry and body plethysmograpghy parameters among enrolled patients before and after bronchodilators
There was a significant increase in FEV1 (L) and FEV1% predicted after BD with mean difference 0.06 ± 0.29L and 6.56 ± 6.27%, respectively. Also, after BD, the FVC (L) and FVC% predicted were significantly increased with mean difference 0.06 ± 0.67L and 8.88 ± 7.09%, respectively.
There was a significant increase in the IC% predicted and the RV (L) after BD with mean difference was 5.16 ± 14.54% and 0.76 ± 3.49L, respectively. The RV/TLC significantly increased after BD with 9.13 ± 14.60 mean difference. All other parameters showed no significant changes after BD (Table 2).
Pre-BD parameters among enrolled patients based on type of response
It was noticed that volume responders (only FVC response to BD) had significantly lower FEV1 (L and % predicted), FVC (L and % predicted), and FEV1/FVC ratio in comparison to other types of response (Table 3).
Distribution of patients based on percentage of change in FEV1
Based on percentage of change in FEV1 after BD, it was noticed that 15% of patients showed a significant increase (12% increase calculated from the pre-BD value and a 0.2 L increase), 80% of patients showed a non-significant increase and 5% of patients had no change in FEV1 after BD (Table 4).
Distribution of patients’ based percentage of change in FVC
Based on percentage of change in FVC after BD, it was noticed that majority (55%) of patients showed significant increase. Non-significant increase was noticed in 126 (42%) patients while 9 (3%) patients had no change in FVC after BD (Table 5).
Relation between percentage of change in FEV1 and FVC
There were significant differences between percentage of FEV1 and that of FVC. It also shows that the number of patients who showed significant reversibility response of FVC was much higher than those who showed the same response of FEV1 after bronchodilator (55% and 15%, respectively). In contrast, number of patients who showed insignificant reversibility response of FEV1 was much higher than those who showed the same response of FVC after bronchodilator (80% and 42%, respectively) (Table 6).
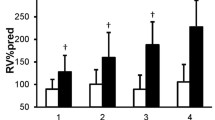
Mean differences of FEV1 and FVC based on GOLD stage among enrolled patients
It was noticed that mean difference of Δ FEV1 (L) after bronchodilator was significantly (P=0.01) decreased with advancing GOLD stage while mean difference of Δ FVC (L) post bronchodilator was significantly increased with advancing GOLD stage (P= 0.03) (Table 7).
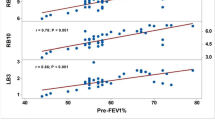
Accuracy of Δ RV and Δ TLC in prediction of significant response based on FEV1
At cutoff point > 20%, Δ RV had 70% sensitivity and 60% specificity with overall accuracy was 61% for prediction of clinical significant response to BD based on FEV1.
Also, at cutoff point > 12%, Δ TLC had 90% sensitivity and 45% specificity with 50% overall accuracy for prediction of clinically significant response to BD based on FEV1 (Table 8, Fig. 1).
Accuracy of Δ RV and Δ TLC in prediction of significant response based on FVC
At cutoff point > 18%, percentage of change in RV had 78% sensitivity and 29% specificity with overall accuracy was 55% for prediction of clinical significant response to BD based on FVC.
Also, at cutoff point > 14%, percentage of change in TLC had 50% sensitivity and 70% specificity with overall accuracy was 64% for prediction of clinical significant response to BD based on FVC (Table 9, Fig. 2).
Distribution of patients based on Δ TLC and Δ RV
Based on calculated cut-off point of Δ RV by receiver operator characteristics (ROC), 11 (3.6%) patients showed non-significant decrease after BD while 165 (55%) patients showed significant decrease. One hundred twenty-four (41.3%) patients had no change after BD.
Based on calculated cutoff point of Δ TLC by receiver operator characteristics (ROC), 249 (73.3%) patients showed no change after BD while only 51 (16.7%) patients showed a significant decrease. Thirty (10%) patients showed non-significant decrease after BD (Table 10).
FEV1 and FVC among the enrolled patients based on mMRC stages
Table 11 showed that different mMRC stages had significant differences as regarding pre BD FEV1 (L), FVC (L), TLC (L), RV (L), and post BD FVC (L) and RV(L) only (P˂ 0.05) (Table 11).
Discussion
COPD is a major cause of chronic morbidity and mortality throughout the world; many people suffer from this disease for years and die prematurely from it or it’s complications. Globally, the COPD burden is projected to increase in the coming decades because of continued exposure to COPD risk factors and aging of the population [25].
Spirometry is required to make the diagnosis in this clinical context; the presence of a post-bronchodilator FEV1/FVC < 0.70 confirms the presence of persistent airflow limitation and thus of COPD in patients with appropriate symptoms and significant exposures to noxious stimuli [1].
Expiratory flow response after administration of a bronchodilator is widely and frequently used as an indicator for the degree of reversibility of airflow limitation in patients with COPD. In severe COPD, flow response after bronchodilator may almost be negligible. Bronchodilator response in terms of lung volumes has been addressed by several authors, as well as the relationship between flow response and volume response [26].
The current study included 300 patients (228 males and 72 females) who were recruited from the outpatient clinic during the period from May 2018 to May 2020. Patients are diagnosed as COPD according to GOLD guidelines 2017 (post bronchodilator FEV1/FVC 0.70 by spirometry).
The purpose of the study was to assess the differences between flow and volume responses after bronchodilator reversibility testing in patients with different COPD GOLD stages (GOLD stage I to GOLD stage IV) and to study the correlation between the bronchodilator response and the severity of the disease. The current study showed that most patients (44%) were classified as severe COPD (GOLD stage IV), whereas only 3 patients met the criteria for mild COPD (GOLD stage I).
Schermer et al. demonstrated that most patients (58.7%) were classified as moderate COPD (GOLD stage II), whereas only 45 (2%) patients met the criteria for very severe COPD (GOLD stage IV). This is possibly because patients in our locality delay seeking medical advice consequencing an advanced GOLD stage at presentation [27].
Falco et al. [28] conducted a retrospective study upon 594 patients with COPD and studied the differences in bronchodilator response regarding flow and the volume parameters in COPD patients at different GOLD stages. They reported that 33.5% of cases were females. In the current study, 24% of cases were female, possibly because smoking habits are more frequent among females in the western society.
Ben Saad et al. [29] reported baseline FEV1=1.46 L and FVC=2.62 L, post BD FEV1=1.59 L and FVC=2.89 L, while the current study found lower baseline and post BD values for FEV1 and FVC. They also reported, ΔFEV1=0.14 L, Δ FEV1% = 11%, Δ FVC=0.27 L, and Δ FVC% =12%. Meanwhile the current study showed ΔFEV1= 0.06 L, Δ FEV1% = 6.56%, whereas ΔFVC= 0.06 L and Δ FVC%=8.88%. These differences may be attributed to different disease severity of the enrolled population in both studies
Reversibility testing showed that 15% of patients had significant increase in FEV1, whereas 55% of patients had significant increase in FVC after bronchodilator inhalation. Thus, FVC detected 40% more responders than FEV1. These results were similar to the results of Ben Saad et al. [29] and Falco et al. [28].
Fortis et al. [30] examined the bronchodilator response (BDR), 5.45% had FEV1-BDR, 15.63% had FVC-BDR, and 11.34% had combined BDR.
Pisi et al. found that 16% of cases were volume responders, 8% were flow responders, and 7% were volume and flow responders [31].
Schermer et al. [27] assumed that the link between flow and volume responses would reverse along with the progression of COPD.
Da Costa et al. [32] agreed with Schermer et al. [27] who suggested that the response measured by FVC is greater at the most severe stages of the disease. The altered effect of lung inflation on airway caliber, due either to loss of lung elastic recoil or compression by enlarged (emphysematous) air spaces may explain the lack of sensitivity to bronchodilatation as assessed by changes in FEV1 in the more severe stages of COPD. Also, Vigna M et al. found that patients belonging to the first GOLD classes tend to be more responsive in terms of flow, a feature that is lost in severe forms, where a volume response prevails [33].
In line with the previous studies, Galal et al. [34] found that ΔFVC increased with the level of airflow obstruction. This volume response, that is increasing improvement in FVC with the level of airflow limitation, makes it a more sensitive parameter to measure the BDR than FEV1 that shows response decline as airways obstruction worsens.
Similar findings were mentioned by Falco et al. [28], Pisi et al. [31], and Boni et al. [15] who concluded that the magnitude of Δ FEV1 decreased as the GOLD stage became more severe and the Δ FVC increased in the more severe GOLD stages.
Newton et al. [17] reported significant increases in FVC and IC and significant reduction in FRC, RV, and TLC following the administration of salbutamol in severely and moderately hyperinflated COPD patients although minority of patients showed significant improvements in FEV1. This was in agreement with the current results.
Cerveri et al. showed an inverse relationship between bronchodilators-induced increments in FEV1 and various indexes of emphysema, in spite of conspicuous increments of FVC. They concluded that isolated volume response to bronchodilators is a characteristic of severe emphysema involving more than 40% of lung parenchyma [35].
Jarenbäck et al. performed spirometry and body plethysmography at baseline and after bronchodilator. Their results stated that volume response does not follow the flow response (FEV1) and flow parameters were more significant in less advanced stage, whereas parameters reflecting volume response (FVC) were more prominent in patients with more severe stages of COPD [36].
Barjaktarevic et al. showed that mild COPD (GOLD I) was characterized by greater BDR in terms of FEV1 than BDR in terms of FVC (35.6% vs 19.2%), a difference that was less marked in GOLD grades II and III. In very severe COPD (GOLD IV), BDR in terms of FEV1 was infrequent (11.3%). To the contrast, the prevalence of BDR in terms of FVC increased with advanced obstruction and was observed most frequently (54.3%) in patients with GOLD IV stage [37].
McCartney et al. [26] studied RV responsiveness at different thresholds for percentage change: 8, 10, 12, 15, and 20%. They concluded that the higher the threshold for RV responsiveness used, the fewer patients were responsive. At threshold for RV (8%), 21.3% of subjects had a RV reduction. At the highest threshold for RV (20%), 4.6% of their total patient population had a reduction in RV. Therefore, 7.7% of subjects currently characterized as being non responsive to bronchodilators have a 20% reduction in their residual volume. The total lung capacity in their study showed increasing response with increasing obstruction.
Measurements of lung volumes before and after bronchodilators added sensitivity when examining for bronchodilator responsiveness. Notably, in hyperinflated patients, the measurement of FVC before and after bronchodilator administration identified a response that may not be uncovered by the measurement of FEV1 alone.
In this study, there were significant changes regarding Δ FVC% in 55%, Δ RV% in 55%, and Δ TLC% in 16.7% of the studied patients after use of bronchodilators. This was concordant with the results of Vigna et al. who stated that FVC improvements after bronchodilator administration are related to the reduction in residual volume (RV), a parameter linked to the improvement in exercise tolerance and dyspnea perception [33].
Limitations of the study are, first, relatively small number of patients in GOLD stages I and II, because this category of patients generally do not ask for medical advice except in the cases of complications or exacerbations and this can be traced back to the culture of the community and that most patients are financially unable and do not pay attention to simple symptoms.
Second, addition of an anticholinergic agent was not a part of the bronchodilator reversibility testing. The use of salbutamol alone will probably not have achieved maximal bronchodilatation in all patients.
This study addressed a category of patients who were residual volume responders; this may put a light on a complementary approach in interpreting bronchodilator reversibility that includes RV to obtain a better understanding of how patients respond to bronchodilators.
In our opinion, more studies are needed to understand the difference between flow and volume responders in all phenotypes of COPD. Future studies should identify the reproducibility and most accurate cut-off values of these volume-based definitions that appear to be useful in defining the effect of bronchodilators in symptomatic COPD patients.
Studies examining the efficacy of new treatments also should pay closer attention to the effect on lung volumes. Further prospective studies examining the behavior of lung volumes after bronchodilator administration in patients with definite clinical diagnoses of COPD are required.
Conclusion
Measurement of lung volumes in addition to the standard spirometric indices is recommended when determining bronchodilator response in COPD patients. A significant proportion of COPD patients showed significant reductions in lung volumes after bronchodilator inhalation, despite classified as being nonresponsive based on spirometry results with minimal or no change in the FEV1.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- COPD:
-
Chronic obstructive pulmonary disease
- FEV1:
-
Forced expiratory volume in first second
- FVC:
-
Forced vital capacity
- GOLD:
-
The Global Initiative for Chronic Obstructive Lung Disease
- BD:
-
Bronchodilator
- RV:
-
Residual volume
- TLC:
-
Total lung capacity
- IC:
-
Inspiratory capacity
References
Global Strategy For The Diagnosis, Management, And Prevention Of Chronic Obstructive Pulmonary Disease (2017 Report). p. 25. https://goldcopd.org/wp-content/uploads/2017/11/GOLD-2018-v6.0-FINALrevised-20-Nov_WMS.pdf
Barros MJ, Rees PJ (1992) Assessment of reversibility in patients with chronic airflow obstruction. Br J Clin Pract 46(2):132–135
Brand PL, Quanjer PH, Postma DS, Kerstjens HA, Koter GH, Dekhuijzen PN et al (1992) Interpretation of bronchodilator response in patients with obstructive airways disease. The Dutch Chronic NonSpecific Lung Disease (CNSLD) Study Group. Thorax 47(6):429–436. https://doi.org/10.1136/thx.47.6.429
Burrows B (1981) An overview of obstructive lung diseases. Med Clin North Am 65(3):455–471. https://doi.org/10.1016/S0025-7125(16)31509-7
Clausen JL (1990) The diagnosis of emphysema, chronic bronchitis, and asthma. Clin Chest Med 11(3):405–416
Rodríguez-Carballeira M, Heredia JL, Rué M, Quintana S, Almagro P (2007) The bronchodilator test in chronic obstructive pulmonary disease: interpretation methods. Respir Med 101(1):34–42. https://doi.org/10.1016/j.rmed.2006.04.018
Shim C (1989) Response to bronchodilators. Clin Chest Med 10(2):155–164
Calverley PM, Albert P, Walker PP (2013) Bronchodilator reversibility in chronic obstructive pulmonary disease: use and limitations. Lancet Respir Med 1(7):564–573. https://doi.org/10.1016/S2213-2600(13)70086-9
Ben Saad H, Prefaut C, Tabka Z, Zbidi A, Hayot M (2008) The forgotten message from gold: FVC is a primary clinical outcome measure of bronchodilator reversibility in COPD. Pul Pharmacol Ther 21(5):767–773. https://doi.org/10.1016/j.pupt.2008.04.005
Manning HL (2000) Bronchodilator therapy in chronic obstructive pulmonary disease. Curr Opin Pulm Med 6(2):99–103. https://doi.org/10.1097/00063198-200003000-00003
Deesomchok A, Webb KA, Forkert L, Lam YM, Ofir D, Jensen D, O’Donnell DE (2010) Lung hyperinflation and its reversibility in patients with airway obstruction of varying severity. COPD 7(6):428–437. https://doi.org/10.3109/15412555.2010.528087
Figueroa-Casas JB, Diez AR, Rondelli MP, Figueroa-Casas MP, Figueroa-Casas JC (2003) Assessment of bronchodilator response through changes in lung volumes in chronic airflow obstruction. Med (B Aires) 63(5):377–382
O’Donnell DE, Forkert L, Webb KA (2001) Evaluation of bronchodilator responses in patients with “irreversible” emphysema. Eur Respir J 18(6):914–920. https://doi.org/10.1183/09031936.01.00216501
Quadrelli SA, Roncoroni AJ, Montiel GC (1999) Evaluation of bronchodilator response in patients with airway obstruction. Respir Med 93(9(9):630–636. https://doi.org/10.1016/S0954-6111(99)90102-6
Boni E, Corda L, Franchini D, Chiroli P, Damiani GP, Pini L, Grassi V, Tantucci C (2002) Volume effect and exertional dyspnoea after bronchodilator in patients with COPD with and without expiratory flow limitation at rest. Thorax 57(6):528–532. https://doi.org/10.1136/thorax.57.6.528
Ramsdell JW, Tisi GM (1979) Determination of bronchodilation in the clinical pulmonary function laboratory. Role of changes in static lung volumes. Chest 76(6):622–628. https://doi.org/10.1378/chest.76.6.622
Newton MF, O’Donnell DE, Forkert L (2002) Response of lung volumes to inhaled salbutamol in a large population of patients with severe hyperinflation. Chest 121(4):1042–1050. https://doi.org/10.1378/chest.121.4.1042
Casanova C, Cote C, de Torres JP, Aguirre-Jaime A, Marin JM, Pinto-Plata V, Celli BR (2005) Inspiratory-to-total lung capacity ratio predicts mortality in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 171(6):591–597. https://doi.org/10.1164/rccm.200407-867OC
Calverley PM (2006) Dynamic hyperinflation: is it worth measuring? Proc Am Thorac Soc 3(3):239–244. https://doi.org/10.1513/pats.200508-084SF
O’Donnell DE, Lam M, Webb KA (1999) Spirometric correlates of improvement in exercise performance after anticholinergic therapy in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 160(2):542–549. https://doi.org/10.1164/ajrccm.160.2.9901038
Steenbruggen I, Mitchell S, Severin T, Palange P, Cooper BG, Spirometry HERMES Task Force. Harmonising spirometry education with HERMES: training a new generation of qualified spirometry practitioners across Europe. Eur Respir J 2011; 37:479–481, 3, doi: https://doi.org/10.1183/09031936.00187810.
V Nitti, G de Michele, B Famiglietti, E Miniccuci, G Ortolani, T Sessa, N Lauro Epidemiological survey of chronic obstructive pulmonary disease in the city of Naples with particular reference to the role of various exogenous factors. Bull Int Union Tuberc.1976;51:685-699, 1 Pt 2.
American Thoracic Society (1991) Lung function testing: selection of reference values and interpretative strategies. Am Rev Respir Dis. 144:1202–1218
Tashkin D, Kesten S (2003) Long-term treatment benefits with tiotropium in COPD patients with and without short-term bronchodilator responses. Chest. 123:1441–1449, 5. https://doi.org/10.1378/chest.123.5.1441
Kim V, Crapo J, Zhao H, Jones PW, Silverman EK, Comellas A, Make BJ, Criner GJ, COPDGene Investigators (2015) Comparison between an alternative and the classic definition of chronic bronchitis in COPDGene. Ann Am Thorac Soc. 12(3):332–339. https://doi.org/10.1513/AnnalsATS.201411-518OC
McCartney CT, Weis MN, Ruppel GL, Nayak RP (2016) Residual volume and total lung capacity to assess reversibility in obstructive lung disease. Respir Care. 61(11):1505–1512. https://doi.org/10.4187/respcare.04323 Epub 2016 Aug 23
Schermer T, Heijdra Y, Zadel S, van den Bemt L, Boonman-de Winter L, Dekhuijzen R, Smeele I (2007) Flow and volume responses after routine salbutamol reversibility testing in mild to very severe COPD. Respir Med. 101(6):1355–1362. https://doi.org/10.1016/j.rmed.2006.09.024
Falco J, Martin V, Marozzi L, Marco A, Aramayo S, Hernández M, Sobrino E et al (2016) Volume response to a bronchodilator in patients with COPD. RAMR 2:144–149
Ben Saad H, Préfaut C, Tabka Z, Zbidi A, Hayot M (2008) The forgotten message from gold: FVC is a primary clinical outcome measure of bronchodilator reversibility in COPD. Pulm Pharmacol Ther. 21(5):767–773. https://doi.org/10.1016/j.pupt.2008.04.005
Fortis S, Comellas A, Make BJ, Hersh CP, Bodduluri S, Georgopoulos D, Kim V, Criner GJ, Dransfield MT, Bhatt SP, Crapo JD, Silverman EK, Make BJ, Regan EA, Beaty T, Begum F, Busch R, Castaldi PJ, Cho M, DeMeo DL, Boueiz AR, Foreman MG, Halper-Stromberg E, Hansel NN, Hardin ME, Hayden LP, Hersh CP, Hetmanski J, Hobbs BD, Hokanson JE, Laird N, Lange C, Lutz SM, ML MD, Parker MM, Qiao D, Regan EA, Santorico S, Silverman EK, Wan ES, Won S, al Qaisi M, Coxson HO, Gray T, MLK H, Hoffman EA, Humphries S, Jacobson FL, Judy PF, Kazerooni EA, Kluiber A, Lynch DA, Newell JD Jr, Regan EA, Ross JC, San Jose Estepar R, Schroeder J, Sieren J, Stinson D, Stoel BC, Tschirren J, van Beek E, van Ginneken B, van Rikxoort E, Washko G, Wilson CG, Jensen R, Everett D, Crooks J, Moore C, Strand M, Wilson CG, Hokanson JE, Hughes J, Kinney G, Lutz SM, Pratte K, Young KA, Curtis JL, Martinez CH, Pernicano PG, Hanania N, Alapat P, Atik M, Bandi V, Boriek A, Guntupalli K, Guy E, Nachiappan A, Parulekar A, DL DM, Hersh C, Jacobson FL, Washko G, Barr RG, Austin J, D’Souza B, GDN P, Rozenshtein A, Thomashow B, MacIntyre N Jr, HP MA, Washington L, McEvoy C, Tashjian J, Wise R, Brown R, Hansel NN, Horton K, Lambert A, Putcha N, Casaburi R, Adami A, Budoff M, Fischer H, Porszasz J, Rossiter H, Stringer W, Sharafkhaneh A, Lan C, Wendt C, Bell B, Foreman MG, Berkowitz E, Westney G, Bowler R, Lynch DA, Rosiello R, Pace D, Criner G, Ciccolella D, Cordova F, Dass C, D’Alonzo G, Desai P, Jacobs M, Kelsen S, Kim V, Mamary AJ, Marchetti N, Satti A, Shenoy K, Steiner RM, Swift A, Swift I, Vega-Sanchez ME, Dransfield M, Bailey W, Bhatt S, Iyer A, Nath H, Wells JM, Ramsdell J, Friedman P, Soler X, Yen A, Comellas AP, Newell J Jr, Thompson B, MLK H, Kazerooni E, Martinez CH, Billings J, Begnaud A, Allen T, Sciurba F, Bon J, Chandra D, Fuhrman C, Weissfeld J, Anzueto A, Adams S, Maselli-Caceres D, Ruiz ME (2019) Combined forced expiratory volume in 1 second and forced vital capacity bronchodilator response, exacerbations, and mortality in chronic obstructive pulmonary disease. Ann Am Thorac Soc 16(7):826–835. https://doi.org/10.1513/AnnalsATS.201809-601OC
Pisi R, Aiello M, Zanini A, Paleari D, Marangio E, Spanevello A, et al (2015) Small airway dysfunction and flow and volume bronchodilator responsiveness in patients with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 1191–1197
Da Costa GM, Faria ACD, Di Mango AMGT, Lopes AJ, Lopes De Melo P (2014) Respiratory impedance and response to salbutamol in healthy individuals and patients with COPD. Respiration. 88(2):101–111. https://doi.org/10.1159/000362691
Vigna M, Aiello M, Bertorelli G, Crisafulli E, Chetta A (2018) Flow and volume response to bronchodilator in patients with COPD. Acta Biomed. 89(7):332–336.
Galal I, Mohammad Y, Nada A, Mohran Y (2018) Medication adherence and treatment satisfaction in some Egyptian patients with chronic obstructive pulmonary disease and bronchial asthma. Egypt J Bronchol. 12(1):33–40
Cerveri I, Pellegrino R, Dore R, Corsico A, Fulgoni P, Van De Woestijne KP et al (2000) Mechanisms for isolated volume response to a bronchodilator in patients with COPD. J Appl Physiol. 88(6):1989–1895. https://doi.org/10.1152/jappl.2000.88.6.1989
Jarenbäck L, Eriksson G, Peterson S, Ankerst J, Bjermer L, Tufvesson E (2016) Bronchodilator response of advanced lung function parameters depending on COPD severity. Int J COPD. 11(1):2939–2950. https://doi.org/10.2147/COPD.S111573
Barjaktarevic IZ, Buhr RG, Wang X, Hu S, Couper D, Anderson W, et al (2019) Clinical signifiance of bronchodilator responsiveness evaluated by forced vital capacity in COPD: SPIROMICS cohort analysis. Int J Chron Obstruct Pulmon Dis. 2927–2938.
Acknowledgements
Not applicable
Funding
None
Author information
Authors and Affiliations
Contributions
GR: conception and of the work, analysis of data, drafted the work and substantively revised it, have approved the submitted version. MM: conception and of the work, analysis of data, drafted the work and substantively revised it, have approved the submitted version. AB: data acquisition and analysis, have approved the submitted version. MF: conception and of the work, analysis of data, drafted the work and substantively revised it, have approved the submitted version. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the ethics committee of the Faculty of Medicine, Assiut University, IRB number 17100284.
All participants or those responsible for them gave written informed consent.
Consent for publication
Consent to publish has been obtained from all participants.
Competing interests
None.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Agmy, G., A. Mahmoud, M., Ali, A.B.ED. et al. Diagnostic performance of lung volumes in assessment of reversibility in chronic obstructive pulmonary disease. Egypt J Bronchol 15, 26 (2021). https://doi.org/10.1186/s43168-021-00066-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43168-021-00066-x