Abstract
Background
There is a clear relationship between poor mental health, obesity, and osteoarthritis (OA). Individuals who experience symptoms of anxiety and depression are more likely to report higher levels of pain and disability in OA. In addition, higher body mass index (BMI) levels can contribute to additional pain and disability in individuals with OA. We aimed to explore the interplay of Body composition, pain intensity, and psychological status in Egyptian patients with knee OA.
Results
This cross-sectional study included 60 patients with Knee OA diagnosed clinically according to the American College of Rheumatology (ACR) criteria. Body composition measurement was performed with an InBody analyzer. Pain was assessed by the pain visual analog scale (VAS), disability was measured with Western Ontario and McMaster Universities Osteoarthritis (WOMAC) scores, and depressed mood and/or anxiety was measured by the Hospital Anxiety and Depression Scale (HADS). Body mass index (BMI), total body fat (TBF) %, fat mass (FM), and fat mass index (FMI) were positively correlated with pain and disability in patients with knee OA. TBF% was positively correlated with depression and anxiety.
Conclusions
This study has shed light on the association between mental disorders, body composition measurements, knee pain, and disability. Interventions to treat osteoarthritis in elderly patients should focus on treating mood changes such as anxiety and depression, psychological support, and controlling body mass with proper diet and exercise programs.
Similar content being viewed by others
Background
Knee osteoarthritis is a common degenerative inflammatory debilitating disease, affecting middle and old age individuals, its global incidence is about 22.9% [1, 2]. Obesity is a well-known risk factor for knee OA due to its important role in its pathogenesis. Not only for the mechanical overload but also for the systemic obesity-induced inflammatory status [3]. The adipose tissue generates adipokines like leptin and enhances the inflammatory profile by increasing the production of interleukin-6 and tumor necrosis factor-alpha [4].
Pain is an early symptom of knee OA even before radiographic changes. Pain usually worsens with disease progression and structural changes, in addition to central sensitization [5].
Obesity can aggravate pain and structural damage, leading to more functional limitations [5, 6], especially if accompanied by muscle mass loss [7]. The level of obesity determined by Body mass index (BMI) was found to be directly associated with clinical consequences of knee OA, but further studies are needed to investigate the effect of different body compositions [8].
Knee OA is more common in overweight and depressed people than in the general population. These conditions are also strongly correlated with pain and limitations on exercise. There is accumulating evidence that being overweight, defined as BMI ≥ 25 kg/m2, and depressive mood, both are linked with the same biological and psychological developmental processes [9].
Patients with knee OA are impacted bio-psychosocially [10]. These patients frequently report having anxiety/depression with a significant correlation between pain and anxiety/depression severity, underlining the need for routine evaluation by clinicians [11]. Both BMI and depressed mood are interrelated and positively associated with pain and activity limitations in knee OA [12].
Body mass index is a widely used measure for body adiposity, although it barely reflects the body composition [13]. Therefore, the assessment of body composition may provide additional information about body fat and skeletal muscle mass, which seem to be linked to numerous musculoskeletal disorders, including knee OA [14]. Bioimpedance analysis (BIA) is used for detailed analyses of different body composition. It is a non-invasive, inexpensive, quick, and reproducible examination [15]. It relies on the fact that tissues rich in water and electrolytes conduct electrical current effectively, while adipose tissue and bone mass exhibit poor conductivity [16].
Analysis of body composition in knee OA patients could be helpful in the evaluation of pain, self-reported function, and psychological status.
Subjects and methods
-
The current cross-sectional study was performed after the approval of the Ethical Committee with ethical approval number 0305839. Informed consent was obtained from each subject included in this study.
-
Sixty patients fulfilled the American College of Rheumatology (ACR) criteria for primary Knee OA with Knee pain and Kellgren-Lawrence grade ≥ 2 [17, 18].
-
All patients were subjected to the following:
-
History taking and full clinical examination (general and local knee examination)
-
Pain assessment by VAS (0–10 scale) [19].
-
Physical functioning assessment by Western Ontario and McMaster University Osteoarthritis Index (WOMAC). It includes three subscales to measure pain, physical function, and joint stiffness [20].
-
Psychological assessment by Hospital Anxiety and Depression Scale (HADS) (a self-screening, 14-item questionnaire incorporating anxiety and depression subscales [21].
-
Body composition analysis using Inbody analyzer ( BODECODE Inbody composition analysis CHL818E, China) to measure indicators of body composition (body mass index, total body fat percentage, visceral fat index, total body water percentage, skeletal muscle percentage, bone mineral content, basal metabolic rate], and to measure fat-free mass and fat mass analysis [fat mass, fat mass index, fat-free mass, fat-free mass index, ratio of fat to skeletal muscle)
-
The sample size was estimated by G-POWER 3.0.10 based on assuming a 95% confidence level and 80% study power, with alpha error equals 0.05, the sample size was calculated to be 54 patients.
-
Statistical analysis was performed using Statistical Package for the Social Sciences Version 25.0 for Windows (SPSS Inc. UK Ltd., Working). Continuous variables were described using means and standard deviation. Pearson correlation was used to measure the degree of association between quantitative variables. Univariate and multivariate regression analyses were performed to study the association and predictive values of body composition or psychological assessment with pain or function in patients with knee OA. The 0.05 level or below was used as the cutoff value for statistical significance.
Results
Sixty patients with knee OA completed this work; 52 females (86.70%) and 8 males (13.3%), their mean age was 52.12 ± 8.4 years old, and the mean disease duration in years was 8.1 ± 3.3.
Scores for pain, functional assessment, HADS, and body composition analysis of the patients are represented in Table 1.
Each of BMI, TBF %, FM, and FMI was positively correlated with the VAS for pain and pain subscale WOMAC score. Total body water (TBW) % was negatively correlated with the VAS.
None of the body composition analysis items was correlated with the stiffness subscale of the WOMAC score, while BMI was positively correlated with the function subscale of the WOMAC score (r = 0.27, p = 0.04*) as seen in Table 2.
VAS for pain was positively correlated with the anxiety subscale of HADS (r = 0.3, p = 0.014*), as well as a strong positive correlation was noted between total WOMAC score and anxiety, depression, and total HADS (r = 0.4, 0.5, 0.5) respectively, and p value 0.0001* (Table 3).
TBF % was positively correlated with anxiety and depression subscales in HADS, while TBW % was negatively correlated with them. There was a significant negative correlation between SM% and the anxiety subscale of HADS (Table 4).
Table 5 represents the results of univariate and multivariate analysis to study the association between BMI, FMI, anxiety component of HADS, and pain:
BMI, FMI, and anxiety were positively and independently associated with VAS for pain.
Table 6 represents the results of univariate and multivariate analysis to study the association between BMI, anxiety, and WOMAC score:
BMI and anxiety were positively and independently associated with WOMAC scores.
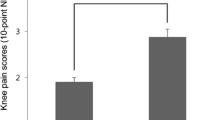
Female patients showed statistically significant higher levels of anxiety, depression, and total HADS in comparison to male patients (Table 7).
Discussion
Knee OA is a significant public health issue that leads to impaired function and reduced quality of life worldwide. In addition to physical symptoms like pain, restricted mobility, and muscle weakness, knee OA can also result in social isolation and depression [9, 22].
This study aims to investigate the relationship between body composition, depressed mood, anxiety, knee pain, and activity limitations in individuals with knee OA. In previous research, there has been a common reliance on indirect measurements of adiposity, such as BMI and waist circumference (WC) [23]. While these measurements are widely used in clinical practice, they may not provide a comprehensive understanding of total body fat and fail to differentiate between lean mass and fat mass. To address this limitation, our current study employed BIA to determine total lean mass and the percentage of body fat aiming to provide more precise and nuanced insights into the distribution and composition of body fat, ultimately contributing to a better understanding of individuals’ overall body composition [24]. Combining both body composition measurements and BMI provides a more comprehensive understanding of physical performance. Previous studies have shown that increased lean mass and muscle strength are associated with a reduced risk of developing symptoms of knee OA. Preserving lean mass is important for maintaining muscle strength, which is crucial for daily activities in individuals with knee OA.
By monitoring both body composition measurements and BMI, it may be possible to gain additional insights into predicting physical performance and the ability to carry out daily activities in individuals with knee OA. This combined approach offers a more nuanced understanding of an individual's overall physical health and functionality [24].
This study represents a seminal contribution to the field, filling a crucial gap in knowledge and paving the way for further investigations in this area.
Our study yielded several interesting results. First, in our current study, we found a positive and significant relationship between anxiety and depression with TBF%. This suggests the relationship between total fat and psychiatric symptoms in overweight individuals which is an important topic in clinical practice. However, we did not observe any significant relationship between depression, anxiety, and BMI. These results are contradictory to those reported by Skilton and colleagues [25], who found an association between BMI categories and depression but not anxiety. Similarly, Scott and colleagues conducted a study across 13 countries and found statistically significant relationships between obesity and both depressive and anxiety disorders. Thus, the findings on the association between mental disorders and BMI remain inconclusive and vary across studies [26].
Several studies have indicated that depressive symptoms can be a significant predictor of abdominal obesity. This relationship is believed to be mediated by the hypothalamus–pituitary–adrenal (HPA) axis. Mood disorders, as chronic stressors, are thought to affect cortisol secretion, thereby stimulating the HPA axis [23].
In our study, we propose that the positive relationship between anxiety and TBF% may be attributed to factors such as pain-related disability, which can limit individuals’ ability to engage in daily activities. Additionally, obesity may hinder the ability of housewives to carry out household activities and provide care for their family members, which can further increase anxiety levels.
Second, there was a direct significant relationship between anxiety with FAT/SM with an inverse correlation found between anxiety and SM. Overall, these findings also indicate a potential relationship between muscle mass and psychiatric symptoms. Patients with a better psychological profile may have higher levels of physical activity, resulting in increased muscle mass. Conversely, individuals with reduced lean mass may be more vulnerable to developing depressive symptoms [23].
It was found that the severity of OA symptoms, as measured by the WOMAC score was directly correlated with FAT/SM. This suggests that individuals with lower muscle mass tend to experience more pain and dysfunction in their knees [27].
Body composition is associated with physical performance in individuals with knee osteoarthritis, this implies that individuals with lower amounts of lean mass may be more susceptible to developing certain psychiatric symptoms and pain. This bidirectional relationship underscores the importance of considering both physical and mental health factors in understanding the interplay between muscle mass and psychiatric symptoms in KOA [23, 24].
Quadriceps weakness is frequently observed in patients with knee OA and has been linked to increased knee pain and reduced physical function. The quadriceps muscles play a crucial role in stabilizing the knee joint and supporting its movement. Therefore, when these muscles are weak, it can lead to greater pain, decreased mobility, and difficulty performing daily activities.
To address this issue, it is crucial to encourage physical activity and physiotherapy in individuals who are at risk for or already experiencing OA. Regular exercise and targeted strengthening exercises can help improve muscle mass, including the quadriceps, and consequently alleviate pain and improve physical function. Physiotherapy interventions, such as muscle strengthening exercises, can be tailored to the individual’s needs and may include techniques such as resistance training, balance exercises, and range of motion exercises.
By promoting physical activity and physiotherapy, healthcare professionals and caregivers can help KOA patients maintain or increase their muscle mass, ultimately reducing pain and improving their quality of life. It is important to emphasize that these interventions should be prescribed and supervised by qualified professionals to ensure safety and effectiveness [24].
Third, this study found that HADS-depression and anxiety were significantly correlated with WOMAC scores in patients with knee OA, suggesting a triadic relationship between physical function, restricted mobility, pain with depression, and anxiety. These conditions may share common neurological and psychological mechanisms.
Neurotransmitters such as serotonin and norepinephrine, as well as other neuropeptides, play a role in the development of pain, depression, and anxiety. Activation of the sympathetic nervous system, involvement of the Hypothalamic Pituitary axis, and down-regulation of benzodiazepine receptors in the frontal cortex are additional mechanisms that may explain the link between these conditions. Psychological factors, such as catastrophizing and hypervigilance, can also mediate the relationship between pain, depression, and anxiety [28].
Similar findings have been reported in previous studies, with anxiety and depression being related to both current pain and increased pain in the future. Kinesio-phobia; fear of exacerbating pain through movement, and pain catastrophizing have been found to predict more severe pain and disability in patients with chronic pain [29]. Chronic pain is known to provoke psychological reactions, including helplessness, anxiety, depression, and anger [30].
Various mechanisms have been proposed to explain the associations between BMI, depressed mood, knee pain, and activity limitations in patients with knee OA. Increased mechanical stress due to excess weight is believed to contribute to knee pain and activity limitations [31].
Fatigue, which is associated with both depressed mood and pain, may also play a role in limiting motor activity and causing activity limitations. Furthermore, low-grade inflammation and dysregulation of the hypothalamic–pituitary–adrenal axis (HPA axis) may explain the interrelations between BMI, depressed mood, knee pain, and activity limitations. Both overweight and depressed individuals have been associated with inflammation, and chronic low-level inflammation may contribute to pain [32].
Low self-efficacy, or low confidence in one's ability to complete tasks or activities, may also explain the connections between BMI, depressed mood, and activity limitations. In both overweight and depressed individuals, low self-efficacy may lead to activity avoidance and subsequent limitations [33]. However, further research is needed to validate these proposed mechanisms in patients with knee OA.
Fourth, we found a direct significant correlation between VAS (assessing knee pain) and WOMAC score (assessing knee pain, stiffness, and physical function) with TBF%, FM, and FMI. Obesity has been associated with chronic inflammation and systemic effects, contributing to musculoskeletal pain. The metabolic syndrome may also play a role in the relationship between obesity and arthritic pain. It was reported that pain is more prevalent among individuals with metabolic syndrome [34].
The adipose tissue, commonly known as body fat, is now acknowledged to be an active endocrine organ that secretes various bioactive molecules, known as adipokines, which play a crucial role in metabolism and inflammation.
Adipokines are hormones and cytokines secreted by adipocytes, the primary cell type in adipose tissue. They could influence energy metabolism, insulin sensitivity, lipid metabolism, inflammation, and vascular function. Some of the important adipokines include Leptin, Adiponectin, Resistin, and Visfatin.
Leptin is known as the “satiety hormone” as it regulates appetite and energy expenditure. It functions by inhibiting appetite and increasing energy expenditure, thereby contributing to body weight regulation. Leptin levels are generally proportional to adipose tissue mass. The dysregulation of adipokines in obesity can lead to various metabolic disturbances, including insulin resistance, chronic inflammation, and cardiovascular diseases. Therefore, understanding the role of adipokines and their interactions is crucial in managing obesity-related complications and developing potential therapeutic strategies.
To sum up, fat tissue is not just a passive storage site for energy but an active endocrine organ that secretes adipokines. These adipokines play a significant role in regulating metabolism, inflammation, and other physiological processes. The dysregulation of adipokines in obesity contributes to metabolic disturbances, highlighting the importance of further research in this area [35,36,37].
Fifth, in our study we found that TBW% was inversely correlated with WOMAC Scale, anxiety, and depression. Bioelectrical impedance analysis (BIA) is a useful tool for determining changes in the volume of body fluids. This is because body fluids act as conductors, allowing the measurement of electrical impedance. The assessment of body fluid volume is particularly important in individuals, as adequate fluid balance is crucial for efficient energy and oxygen delivery to vital organs like the brain, heart, and lungs [37].
The significant negative association between total body water distribution in knee OA patients and both VAS and WOMAC scores, observed in the present study, suggests that decreased total body water likely contributes to altered water distribution within the knee joint contributing to the structural and functional changes found in these patients. Water content plays a crucial role in maintaining the integrity and function of joint tissues [24].
By utilizing BIA, medical professionals can potentially reduce the need for costly and invasive tests, while still gathering important information about fluid status in elderly patients. Routine screening of body fluid volume using BIA can aid in the management, allowing for early detection of imbalances and timely interventions to optimize their health and well-being. Embracing BIA as a part of routine screening protocols would not only streamline healthcare practices but also contribute to promoting healthier lifestyles among the elderly population [37].
The relationship between mental disorders such as depression and anxiety and obesity has been a topic of significant research interest in recent years. Some studies have found a positive relationship between anxiety, depression, and BMI, suggesting that higher levels of anxiety and depression may be associated with higher BMI [26, 38].
However, another study found no significant relationship between mental disorders and BMI [39]. As a result, the findings on the relationship between mental disorders and BMI remain inconsistent.
Furthermore, our research has highlighted a significant gender difference in the occurrence of depression among individuals diagnosed with knee osteoarthritis (OA). Specifically, our findings suggest that women suffering from knee OA are more prone to experiencing higher levels of depression when compared to OA male patients. These findings align with the research conducted by Silverwood et al., who also observed elevated levels of depression among women with OA, in comparison to men [40].
Several factors may contribute to the lower prevalence of depression in men with knee OA. Continued engagement in activities and limited participation in outdoor activities among women may be influencing this disparity. Men may be more likely to maintain involvement in activities that promote their mental well-being, potentially shielding them from experiencing depression. Conversely, women may have fewer opportunities for engagement due to societal expectations and traditional gender roles that tend to assign them primary roles as wives and caregivers. These expectations may contribute to the higher levels of depression observed in women with knee OA.
Overall, our findings highlight the importance of recognizing the gender-specific impact of knee OA on mental health, particularly focusing on addressing societal expectations and enabling equal opportunities for engagement and participation in activities. By acknowledging and addressing these gender disparities, we can work towards improving the mental well-being of individuals afflicted by knee OA and provide more targeted interventions for those most at risk.
Conclusion
In conclusion, this study has shed light on the association between mental disorders, body composition measurements, knee pain, and activity limitations. It highlights the significance of addressing total body fat (TBF), fat mass (FM), and mood disorders such as depression and anxiety in the management of knee osteoarthritis (OA). By considering these factors together, healthcare professionals can enhance treatment outcomes for patients. Future research should explore these psychosocial factors in more detail and investigate their interactions with other biological and mechanical factors to develop comprehensive treatment approaches.
Ultimately, if BIA can be established as an effective tool for predicting knee OA progression, it would offer significant benefits in terms of early intervention and personalized treatment strategies. However, additional research is required to fully elucidate the potential of BIA in this regard.
Study limitations
There are a few limitations to consider in this study. The first limitation is that it had a cross-sectional design. Future longitudinal studies, which follow participants over time, would be needed to confirm and explore the findings in greater depth.
The second limitation is the relatively small sample size. A small sample size can decrease the generalizability of the results and may limit the statistical power to detect small but meaningful effects. To enhance the reliability and generalizability of the findings, future studies could involve larger sample sizes.
Another limitation is the exclusive use of bioelectrical impedance analysis (BIA) for measuring body composition. While BIA is a widely used method for estimating body composition, there are other methods available such as dual-energy X-ray absorptiometry (DXA) and air displacement plethysmography (ADP). Comparing the results from different measurement methods could provide a more comprehensive and accurate assessment of body composition.
Overall, while this study provides valuable insights, it is important to acknowledge these limitations and consider them when interpreting the findings. Further research with longitudinal studies to assess the treatment of anxiety and depression by drugs versus psychological support on VAS for OA pain. Comparing the VAS score of patients living in senior homes with those living family lives or living alone.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ACR:
-
American College of Rheumatology
- BIA:
-
Bioimpedance analysis
- BMC:
-
Bone mineral content
- BMI:
-
Body mass index
- FFM:
-
Fat-free mass
- FFMI:
-
Fat-free mass index
- FM:
-
Fat mass
- FMI:
-
Fat mass index
- HADS:
-
Hospital Anxiety and Depression Scale
- OA:
-
Osteoarthritis
- SM:
-
Skeletal muscle
- TBF:
-
Total body fat
- TBW:
-
Total body water
- VAS:
-
Visual analog scale
- VFI:
-
Visceral fat index
- WOMAC:
-
Western Ontario and McMaster Universities Osteoarthritis scores
References
Salis Z, Gallego B, Nguyen TV, Sainsbury A (2023) Association of decrease in body mass index with reduced incidence and progression of the structural defects of knee osteoarthritis: a prospective multi-cohort study. Arthritis Rheumatol 75(4):533–543
Du X, Liu ZY, Tao XX, Mei YL, Zhou DQ, Cheng K et al (2023) Research progress on the pathogenesis of knee osteoarthritis. Orthop Surg. 15(9):2213–24
Shumnalieva R, Kotov G, Monov S (2023) Obesity-related knee osteoarthritis—current concepts. Life 13(8):1650
Fantuzzi G (2005) Adipose tissue, adipokines, and inflammation. J Allergy Clin Immunol. 115(5):911–9. (Quiz 20)
Mahmoudian A, Lohmander LS, Mobasheri A, Englund M, Luyten FP (2021) Early-stage symptomatic osteoarthritis of the knee — time for action. Nat Rev Rheumatol 17(10):621–632
Driban JB, Price LL, Lynch J, Nevitt M, Lo GH, Eaton CB, McAlindon TE (2016) Defining and evaluating a novel outcome measure representing end-stage knee osteoarthritis: data from the Osteoarthritis Initiative. Clin Rheumatol 35:2523–2530
Kim BS, Lee SY, Kim BR, Choi JH, Kim SR, Lee HJ, Lee SJ (2021) Associations between obesity with low muscle mass and physical function in patients with end-stage knee osteoarthritis. Geriatr Orthop Surg Rehabil 12:21514593211020700
Raud B, Gay C, Guiguet-Auclair C, Bonnin A, Gerbaud L, Pereira B et al (2020) Level of obesity is directly associated with the clinical and functional consequences of knee osteoarthritis. Sci Rep 10(1):3601
Holla JF, van der Leeden M, Knol DL, Roorda LD, van der Esch M, Voorneman RE et al (2013) The association of body-mass index and depressed mood with knee pain and activity limitations in knee osteoarthritis: results from the Amsterdam osteoarthritis cohort. BMC Musculoskelet Disord 14:1–7
Foo CN, Arumugam M, Lekhraj R, Lye M-S, Mohd-Sidik S, Jamil OZ (2020) Effectiveness of health-led cognitive behavioral-based group therapy on pain, functional disability and psychological outcomes among knee osteoarthritis patients in Malaysia. Int J Environ Res Public Health 17(17):6179
Fonseca-Rodrigues D, Rodrigues A, Martins T, Pinto J, Amorim D, Almeida A, Pinto-Ribeiro F (2021) Correlation between pain severity and levels of anxiety and depression in osteoarthritis patients: a systematic review and meta-analysis. Rheumatology 61(1):53–75
Holla JFM, van der Leeden M, Knol DL, Roorda LD, van der Esch M, Voorneman RE et al (2013) The association of body-mass index and depressed mood with knee pain and activity limitations in knee osteoarthritis: results from the Amsterdam osteoarthritis cohort. BMC Musculoskelet Disord 14(1):296
Ponti F, Santoro A, Mercatelli D, Gasperini C, Conte M, Martucci M et al (2020) Aging and imaging assessment of body composition: from fat to facts. Front Endocrinol 10:861
Ferreira AS, Mentiplay BF, Taborda B, Pazzinatto MF, de Azevedo FM, Silva DDO (2023) Exploring overweight and obesity beyond body mass index: a body composition analysis in people with and without patellofemoral pain. J Sport Health Sci 12(5):630–638
Hemmingsson E, Uddén J, Neovius M (2009) No apparent progress in bioelectrical impedance accuracy: validation against metabolic risk and DXA. Obesity 17(1):183–187
Kahraman A, Hilsenbeck J, Nyga M, Ertle J, Wree A, Plauth M et al (2010) Bioelectrical impedance analysis in clinical practice: implications for hepatitis C therapy BIA and hepatitis C. Virol J 7(1):1–8
Altman R, Asch E, Bloch D, Bole G, Borenstein D, Brandt K et al (1986) Development of criteria for the classification and reporting of osteoarthritis: classification of osteoarthritis of the knee. Arthritis Rheumatol 29(8):1039–1049
Felson DT, Niu J, Guermazi A, Sack B, Aliabadi P (2011) Defining radiographic incidence and progression of knee osteoarthritis: suggested modifications of the Kellgren and Lawrence scale. Ann Rheum Dis 70(11):1884–1886
Hawker GA, Mian S, Kendzerska T, French M (2011) Measures of adult pain: Visual analog scale for pain (vas pain), numeric rating scale for pain (nrs pain), mcgill pain questionnaire (mpq), short-form mcgill pain questionnaire (sf-mpq), chronic pain grade scale (cpgs), short form-36 bodily pain scale (sf-36 bps), and measure of intermittent and constant osteoarthritis pain (icoap). Arthritis Care Res (Hoboken) 63(S11):S240–S252
Guermazi M, Poiraudeau S, Yahia M, Mezganni M, Fermanian J, Elleuch MH, Revel M (2004) Translation, adaptation and validation of the Western Ontario and McMaster Universities osteoarthritis index (WOMAC) for an Arab population: the Sfax modified WOMAC. Osteoarthr Cartil 12(6):459–468
Terkawi AS, Tsang S, AlKahtani GJ, Al-Mousa SH, Al Musaed S, AlZoraigi US et al (2017) Development and validation of Arabic version of the hospital anxiety and depression scale. Saudi J Anaesth 11(Suppl 1):S11
Fouad R, Hassan B (2017) Relationship between pain intensity, body mass index and psychological status of geriatric patients with knee osteoarthritis. IOSR-JNHS 06:35–43
Guedes EP, Madeira E, Mafort TT, Madeira M, Moreira RO, Mendonça LM et al (2013) Body composition and depressive/anxiety symptoms in overweight and obese individuals with metabolic syndrome. Diabetol metab syndr 5:1–5
Davis HC, Blue MN, Hirsch KR, Luc-Harkey BA, Anderson KC, Smith-Ryan AE, Pietrosimone B (2020) Body composition is associated with physical performance in individuals with knee osteoarthritis. J Clin Rheumatol. 26(3):109–14
Skilton MR, Moulin P, Terra J-L, Bonnet F (2007) Associations between anxiety, depression, and the metabolic syndrome. Biol Psychiatry 62(11):1251–1257
Scott KM, Bruffaerts R, Simon GE, Alonso J, Angermeyer M, De Girolamo G et al (2008) Obesity and mental disorders in the general population: results from the world mental health surveys. Int J Obes 32(1):192–200
Davis HC, Blue MNM, Hirsch KR, Luc-Harkey BA, Anderson KC, Smith-Ryan AE, Pietrosimone B (2020) Body composition is associated with physical performance in individuals with knee osteoarthritis. J Clin Rheumatol 26(3):109–114
Bair MJ, Wu J, Damush TM, Sutherland JM, Kroenke K (2008) Association of depression and anxiety alone and in combination with chronic musculoskeletal pain in primary care patients. Psychosom Med 70(8):890
Smith BW, Zautra AJ (2008) The effects of anxiety and depression on weekly pain in women with arthritis. Pain 138(2):354–361
Picavet HSJ, Vlaeyen JW, Schouten JS (2002) Pain catastrophizing and kinesiophobia: predictors of chronic low back pain. Am J Epidemiol 156(11):1028–1034
Elbaz A, Debbi EM, Segal G, Haim A, Halperin N, Agar G et al (2011) Sex and body mass index correlate with Western Ontario and McMaster Universities Osteoarthritis Index and quality of life scores in knee osteoarthritis. Arch Phys Med Rehabil 92(10):1618–1623
Hawker GA, Gignac MA, Badley E, Davis AM, French MR, Li Y et al (2011) A longitudinal study to explain the pain-depression link in older adults with osteoarthritis. Arthritis Care Res 63(10):1382–1390
Tomey K, Sowers MR, Harlow S, Jannausch M, Zheng H, Bromberger J (2010) Physical functioning among mid-life women: associations with trajectory of depressive symptoms. Soc Sci Med 71(7):1259–1267
Karelis AD, St-Pierre DH, Conus F, Rabasa-Lhoret R, Poehlman ET (2004) Metabolic and body composition factors in subgroups of obesity: what do we know? J Clin Endocrinol Metab 89(6):2569–2575
Pottie P, Presle N, Terlain B, Netter P, Mainard D, Berenbaum F (2006) Obesity and osteoarthritis: more complex than predicted!. Ann Rheum Dis 65(11):1403–5
Sowers M, Yosef M, Jamadar D, Jacobson J, Karvonen-Gutierrez C, Jaffe M (2008) BMI vs. body composition and radiographically defined osteoarthritis of the knee in women: a 4-year follow-up study. Osteoarthr. Cartil. 16(3):367–72
Ertürk C, Altay MA, Sert C, Levent A, Yaptı M, Yüce K (2015) The body composition of patients with knee osteoarthritis: relationship with clinical parameters and radiographic severity. Aging Clin Exp Res 27:673–679
Atlantis E, Baker M (2008) Obesity effects on depression: systematic review of epidemiological studies. Int J Obes 32(6):881–891
John U, Meyer C, Rumpf HJ, Hapke U (2005) Relationships of psychiatric disorders with overweight and obesity in an adult general population. Obes Res 13(1):101–109
Silverwood V, Blagojevic-Bucknall M, Jinks C, Jordan J, Protheroe J, Jordan K (2015) Current evidence on risk factors for knee osteoarthritis in older adults: a systematic review and meta-analysis. Osteoarthr Cartil 23(4):507–515
Acknowledgements
Not applicable.
Funding
The authors received no specific funding for this work.
Author information
Authors and Affiliations
Contributions
All authors shared in writing and reviewing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The local Ethics Committee of Faculty of Medicine, Alexandria University, Egypt (IRB NO:00012098-FWA NO:00018699) approved the study. Serial number: 0305839. Informed consent was obtained from every patient.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Khalil, N.F.W., Hassan, M.M. & Elshatby, N.M. The interplay of body composition, pain intensity, and psychological status in Egyptian patients with knee osteoarthritis. Egypt Rheumatol Rehabil 51, 15 (2024). https://doi.org/10.1186/s43166-024-00248-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43166-024-00248-7