Abstract
Background
Intervertebral disc degeneration (IVD) is a main underlying cause for low back pain (LBP). Oswestry Disability Index (ODI) is a valuable tool used to measure patient’s low back functional outcome. Our aim is to evaluate the relation between clinical assessment of LBP and health related quality of life with the use of ODI and magnetic resonance image (MRI) findings in patients with degenerative prolapsed IVD disease.
Result
There was a significant correlation between Pfirrmann grades and ODI (p < 0.0001) and with type of disc morphology mostly protrusion (p < 0.0001) but insignificant correlation with visual analogue scale (VAS) (p = 0.198) and most of the clinical parameters (p > 0.05). There was a significant correlation between ODI and VAS (p = 0.003). Higher Pfirrmann grades were found at lower lumbosacral levels L4-5 and L5-S1.
Conclusion
Higher Pfirrmann grades correlated with the increased ODI. No association was found between MRI grading in lumbosacral spine with pain intensity and most of the clinical parameters among persons with discogenic LBP. Chronic LBP is widely accepted to be a multifactorial disorder that could not be contained within a single lumbar compartment. Clinician should not depend on MRI findings only in the diagnosis. History from the patient and clinical examination is particularly important to reach the final diagnosis. ODI might be convenient in achieving patient’s confidence and decreasing unnecessary investigations.
Similar content being viewed by others
Introduction
Low back pain (LBP) is a major debilitating condition with negative socioeconomic consequences that affects 80% of the general population at some point in time. LBP impairs daily function, lowers quality of life, and raises work disability and healthcare costs [1]. A main underlying cause for LBP incidence is intervertebral disc degeneration (IVD), the risk of which has been attributed to genetic, environmental, and lifestyle factors [2, 3]; among these, overweight and obesity, or rather body fat, have been associated with increased LBP rates. Even though body weight exerts its deleterious effects on the spine due to altered biomechanics (e.g., loading), it is suggested that fat-induced biochemical and metabolic changes may play a role in the development of IVD and LBP [4, 5].
The Oswestry Disability Index (ODI), known as the Oswestry Low Back Pain Disability Questionnaire, is an extremely important tool used by researchers and disability evaluators to measure patient’s permanent functional disability and is considered a “gold standard” low back functional outcome tool [6].
The gold standard for assessing the relationship of disc material to soft tissue and neural structure is magnetic resonance imaging (MRI)s [7]. The IVD is a fibrocartilaginous structure made up of three distinct components (nucleus pulposus, annulus fibrosus, and the cartilaginous endplates). If the integrity of those three structures is disturbed, this may result in a compromised function of the whole IVD leading to dynamic morphologic and cellular alterations with age and degeneration. Pfirrmann et al. suggested a morphologic grading system which is based on T2-weighted sagittal images that showed a good interobserver accuracy [8].
Our study aimed to evaluate the relation between clinical assessments of LBP and health related quality of life using ODI and MRI findings in patients with degenerative prolapsed IVD disease.
Subjects and methods
Subjects
The study included 100 patients with LBP due to degenerative prolapsed IVD disease with duration more than 3 months (patients were selected after MRI testing). Patients were recruited from the Rheumatology and Rehabilitation Outpatient Clinic Mataria Teaching Hospital. Patients with vertebral fractures, trauma, spinal inflammatory disease, spinal infection, spinal malignancies, spondylolisthesis, congenital spinal deformities, cauda equine syndrome, myelopathy, pregnancy, and psychogenic back pain were excluded from the study. The study was explained to the studied subjects, and an informed consent was given by each.
Methods
All study populations were subjected to the following:
-
Full history and complete general and full neurological examination
-
Pain intensity assessment using visual analogue scale (VAS) [9]
-
Measurements of body mass index (BMI) calculated as weight (kg)/[height (m)] [2] and waist circumference (WC) [2]
-
The Oswestry Low Back Pain Disability Questionnaire (Oswestry Disability Index (ODI)) [10]: In a questionnaire of 10 sections (translated into Arabic), each one focuses on a different aspect of daily life, such as pain intensity, personal care, lifting, walking, sitting, standing, sleeping, sex life, social life, or travelling. The patient was asked to rate how much LBP has affected each of these aspects of his/her life. The total score/50 × 100 = percentage of disability.
-
Interpretation: The ODI score ranges from 0% (no disability) to 100% (maximum disability). In zero to 20% (minimal disability), the patient can manage most living activities. In total of 21–40% (moderate disability), the patient suffers more pain and difficulty with sitting, lifting, and standing. Travelling and social activities are more difficult for them, and they may be unable to work; personal care sexual activity and sleeping are not completely affected. In total of 41–60% (severe disability), pain is the main problem, but there is affection of activities of daily living. In total of 61–80% (crippled), back pain interferes with all aspects of patient’s life. In total of 81–100%, these patients are bed bound or exaggerating their symptoms. The optimal cutoff value was estimated to be 12 [11].
-
Image acquisition: MRI of lumbosacral spine (LSS) from L2-3 to L5-S1 was obtained with a closed 1.5-Tesla instrument (Ingenia Philips, The Netherlands devices) with the following sequences: T1WI axial and sagittal TR/TE T2WI axial and sagittal. Sagittal images (T2 weighted) were obtained for evaluation, and these images had a repetition/echo time of 2000/110 ms, an acquisition matrix of 256 × 256 pixels, and a slice thickness/inter-slice gap of 5/0.5 mm. The corresponding disc level’s cerebrospinal fluid was used as a reference for signal intensity [12]. The findings analyzed were as follows:
Grading of the IVD was determined using the T2-weighted, midsagittal disc signal according to the Pfirrmann grading [8].
Pfirrmann and his colleagues suggested a 5-point MRI-based scale (grade 1-grade 5) based on MRI signal intensity, disc structure, and distinction between nucleus and annulus and disc height. The disc degeneration was graded from grade 1 (homogenous disc structure, with clear distinction of nucleus and annulus, signal intensity is high, and intervertebral height is normal) to grade 5 (disc structure is black and inhomogeneous without distinction of nucleus and annulus, signal intensity is low, and height is collapsed).
Type of disc herniation: Discs are classified according to the morphology of their contour using the terms normal, bulge, protrusion, and extrusion [13]. Disc bulge is a regular circumferential disc extension outside the interspace, disc protrusion an asymmetrical extension of the disc outside the interspace with broad base, and disc extrusion is a localized disc extension outside the interspace with narrow base, and separated fragments are referred as sequestration.
Nerve root compression: Lumbar nerve root compromise was graded according to Pfirrmann et al. [13]
-
Grade 0: No compromise
-
Grade 1: There is contact of the disc material with the nerve root, and epidural fat layer between them is not obvious.
-
Grade 2: Dorsal dislocation of the nerve by the disc material
-
Grade 3: Nerve root compression between the disc material and the spinal canal wall
Ethics approval and consent to participate
This study was conducted after the approval of the ethics committee of the General Organization for Teaching Hospitals and Institutes (GOTHI), with reference number HM000118. All patients in this study gave written informed consent to participate in this research.
Statistical analysis
The statistical package IBM SPSS version 25 software was used for the analysis. Descriptive statistics were used to summarize them: mean, standard deviation, minimal and maximum values for quantitative variables, and number and percentage for qualitative values. One-way ANOVA was used to test for statistical differences between groups. Pearson’s correlation was used to examine the independent variables that were significantly associated with the parameters under consideration. p-values ≤ 0.05 were considered statistically significant.
Results
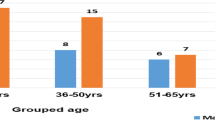
This study included 100 patients with LBP due to degenerative prolapsed IVD with mean age 44.7 ± 10.8 years (ranged from 21 to 70 years). Seventy-nine percent of the patients were women, and 21% were men. Twelve percent were smokers. Regarding the employment, 69% were hard workers, and 31% were sedentary. The mean BMI was 33.6 ± 6.8 and ranging from 20 to 56.6 kg/m2. The mean waist circumference was 98.68 ± 14.5 and ranging from 77 to 139 cm, while the mean disease duration was 5.16 ± 4.7 and ranging from 0.03 to 21.67 years (Table 1).
Clinical assessment in the study population
Sacroiliac pain was detected in 18% of the patients, 6% on the right side, and 3% on the left side, and 9% was bilaterally presented. Numbness/paresthesia was present in 78% and 73% of patients respectively, and claudication pain was found in 41% of patients. Radicular leg pain was found in 93% of the patients, 31% on the right side, and 22% on the left side, and 40% was bilaterally presented. Spinal stiffness and back muscle spasm were detected in 67% and 39% of patients respectively. Lumbar ROM showed limited flexion in 48% patients and limited extension in 37% patients with limited lateral flexion in 43%. Straight leg raising (SLR) test was positive in 86% of patients, 36% of them were on the right leg, 20% in the left, and bilaterally presented in 30% of patients. Femoral stretch test was positive in 50% of patients. Thirty-six percent of patients had lower extremities muscle weakness, and urinary symptoms were found in 15% of patients. Pain intensity using VAS for back pain ranged from 3 to 10 with a mean 7.43 ± 1.3.
Functional disability score as assessed by ODI
Considering the distribution of LBP patients according to the degree of disability, the mean value for ODI was 49.14 ± 17.4 ranging from 12 to 90. The majority of patients suffered moderate (27%) to severe (46%) disability. Minimal disability was reported among 4% of patients, while 16% were crippled, and 7% were bedridden (Table 2).
Pfirrmann grading system of disc degeneration in the study population
In total, 400 lumbar discs at the levels from L2-3 to L5-S1 were analyzed in 100 patients. The analysis of Pfirrmann grading system revealed that the prevalence of grades was as follows: grade 1 (2%), grade 2 (14%), grade 3 (38%), grade 4 (35%), and grade 5 discs (11%) (Table 3, Fig. 1). Table 4 summarizes the disc degeneration grades number and percentage. The evaluation revealed that in grade 1, the frequency was low at the L2-3 (5%) and L3-4 (3%) levels with no change at levels L4-5 and L5-S1. Grade 2 changes were higher at upper lumbar levels (L2-3 (26%) and L3-4 (15%)) than lower levels (L4-5 (9%) and L5-S1 (6%)). Grade 3 frequency changes were higher at upper lumbar levels (L2-3 (60%) and L3-4 (46%)) than lower lumbar levels (L4-5 (19%) and L5-S1 (27%)). Grade 4 was lower at the L2-3 (6%) and L3-4 (32%) but increased at lower levels L4-5 (59%) and L5-S1 (43%). Grade 5 showed lower frequency at the L2-3 (3%) and L3-4 (4 %) but higher frequency at lower lumbosacral levels L4-5 (13%) and L5-S1 (24%).
Assessment of disc morphology
Considering disc morphology in 400 discs, 13% had normal morphology, 32.5% showed disc bulge, 48% had disc protrusion, and 6.5% had disc extrusion and sequestration (Table 3).
Evaluation of nerve root compression grading
Concerning nerve root compression grading in 400 discs, 31% discs had grade 0 (normal), grade 1 (contact) was present in 27% discs, and grade 2 (deviation) and grade 3 (compression) were present in 22% and 20% discs, respectively.
Other MRI findings
Other findings such as spinal canal stenosis was detected in 18% of patients, osteoarthritis of the facet joint in 42% of patients, and ligamentum flavum hypertrophy in 21% (Table 3).
Correlation study
The correlation studies between functional disability, radiological findings, and clinical parameters were done (Table 5).
Correlation between ODI and different parameters
Statistically significant positive correlation was found between ODI and VAS (r = 0.292**, p = 0.003), Pfirrmann grading (r = 0.584**, p < 0.0001), BMI (r = 0.320**, p = 0.001), SLR (r = 0.268**, p = 0.007), paresthesia (r = 0.237*, p = 0.017), and muscle weakness (r = 0.252*, p = 0.012).
Correlation study between VAS and different parameters
Statistically significant positive correlation is between VAS and ODI (r = 0.292**, p = 0.003) and SLR (r = 0.234, p = 0.019).
No significant association was found between VAS and Pfirrmann grading (r = 0.130, p = 0.198), BMI (r = 0.133, p = 0.187), paresthesia (r = 0.114, p = 0.259), or muscle weakness (r = 0.072, p = 0.476).
Correlation study between Pfirrmann grading and different parameters
There were statistically significant positive correlation between Pfirrmann grading and ODI (r = 0.584, p < 0.0001) and SLR (r = 0.240*, p = 0.016). No significant association was found between grading and VAS (r = 0.130, p = 0.198), BMI (r = 0.097, p = 0.339), paresthesia (r = 0.176, p = 0.08), or muscle weakness (r = 0.143, p = 0.155).
Correlation study between type of disc herniation (morphology) and different parameters
There were statistically significant positive correlation between type of disc herniation and ODI (r = 0.403**, p < 0.0001), VAS (r = 0.251*, p = 0.012), Pfirrmann grading (r = 0.819**, p < 0.0001), SLR (r = 0.204*, p = 0.042), paresthesia (r = 0.260**, p = 0.009), and muscle weakness (r = 0.215*, p = 0.032). No statistically significance difference was found between type of disc herniation and BMI (r = 0.085, p = 0.339).
There was a significant relationship between severity of ODI and VAS compared to disc morphology mostly protrusion (p < 0.001) (Table 6).
Discussion
LBP represents a frequent musculoskeletal disorder in all age groups around the world. Its prevalence ranges between 25 and 60%, making it a common cause of activity restriction in people under the age of 50. Besides, more than 85% of all people had LBP at some time in their life [6]. Because almost all lumbar structures are potential sources of LBP, it could be a cause. One of the main causes of LBP is IVD of the lumbar spine [14]. Pain is an extremely individual dependent experience and is affected by a multifactorial factor [15]. The IVD is a compound of a fibrocartilaginous structure made up of three distinct components. Those are the nucleus pulposus, the annulus fibrosus, and the cartilaginous end plates. If the integrity of any of those three structures is disturbed, compromised function of the whole IVD may result which undergoes dynamic morphologic and cellular alterations with age and degeneration [4]. Our aim was to evaluate the relation between clinical assessments of LBP and health related quality of life with the use of ODI and MRI findings in patients with degenerative prolapsed IVD.
This study found that disc degeneration was more common in females than males, which was consistent with Kaadeh et al. [16] where 55.4% of the patients were females and were inconsistent with prior studies and that the male patients were more affected than female patients [17,18,19].
Being overweight had a great association with IVD [2, 5, 15, 20,21,22]. In this study, the mean of BMI was 33.62 ± 6.87 and was in agreement with prior studies as obesity is a result of poor lifestyle which affects the deterioration of back pain.
In our study, functional disability was assessed by using ODI with a mean of 49.14 ± 17.4. Various studies reported that this self-administered questionnaire was reproducible, constant, valid, and very useful in assessing disability in patients complaining of LBP due to disc disease and had a response rate of 100%. Although ODI score could not assess pain directly, it offered an idea by evaluating the disability level due to LBP [23, 24]. There was a strong correlation between ODI and VAS in patients with disc herniation which was consistent with Hasanović-Vučković et al. [25] and was inconsistent with Bajpai et al. [26] and Corniola et al. [27] A statistically significant difference was seen between ODI and clinical parameters (p < 0.05).
The most common site of degenerative changes of lumbosacral spine was L4-5 followed by L5-S1 level, and the least was L2-3 in accordance with other studies [17, 26, 28,29,30,31]. As regards the disc morphology, the commonest type was disc protrusion (48%), 32.5% showed disc bulge, and 6.5% had disc extrusion and sequestration, and this agreed with Ravikanth et al. [17]; they found that the commonest type was disc protrusion (69.4%). There was a highly significant correlation between disc morphology and ODI (p < 0.0001), VAS (p = 0.012), and clinical symptomatology of lumbar disc disease (p = <0.05). The data was in support with Ravikanth et al. [17]; they deduced that there was a highly significant correlation between disc protrusion and clinical symptomatology of lumbar disc disease; also, Hamada and Abou-Zeid [32] found few clinical correlations with herniated fragment morphology. Bajpai et al. [26] confirmed that the most significant finding was that the degree of disc herniation was correlated well with the symptoms.
In this study, an analysis of the Pfirrmann grading revealed that there were a higher number of lumbar discs with Pfirrmann grades 3 and 4 changes (38% and 35%) in comparison with lumbar discs with Pfirrmann grades 2 and 5 (14% and 11%). Only 2% showed no degenerative changes in lumbar discs. There was an association between MRI findings and functional disability among persons with LBP (p < 0.0001), which is in favor with Middendorp et al. [15] and Kaadeh et al. [16], as there was a weak correlation between grading and ODI. This finding was against Wani and Deshpande [33] as there was no relation between ODI and MRI grading (p < 0.759). There was no association between pain intensity recorded on VAS and MRI findings which is in favor of Wani and Deshpande [33] and Kohat et al. [28] results. This finding might suggest that although MRI is a good marker of a patient’s clinical status, it is still difficult to diagnose the cause of LBP by imaging alone. Kaadeh et al. [16] found a significant relationship between the pain severity and MRI findings with the exception of L4-5-disc degeneration; there was significant pain in the patients with L4-5 disc degeneration grade 2 (p = 0.005). There was also no statistically significant difference between clinical parameters and MRI grading as p > 0.05. The finding of our study is in favor of other studies Hamada and Abou-Zeid [32] and Corniola et al. [27], which prospectively studied 284 patients with degenerative disc disease scheduled for lumbar spine surgery. They investigated their cases with numerous clinical questionnaires (including ODI and VAS) and imaging scans. At last, they failed to find an association between questionnaires’ scores and imaging features. They discovered that there was not any significant association between any radiological grading scales and any one of the clinical tests. The data was not in agreement with other studies that found a correlation between clinical and MRI grading [26, 34,35,36]. The lack of relationship between MRI grading and clinical parameters suggested that it might be determined by multiple factors. These data clarified the difficulty to rate the clinical symptoms accurately based only on imaging findings. All structures are considered possible causes of LBP, and therefore, it is necessary to consider everything. For this reason, we correlated grading with ODI in this study in which a strong correlation was found between signs of degeneration and ODI. The studies of Corniola et al. [27] and Middendorp et al. [15] provided compelling evidence that the association between lumbar spine degeneration on MRI and the clinical symptoms is doubtful. Therefore, the patient’s history and neurological examination should be the basis for any clinical decisions. Imaging results should help to support the clinical diagnosis and point out any other important features of the illness or other potential diagnoses, such as instability, infections, or neoplastic disease. In fact, the presented findings appeared to support the common thesis that chronic LBP is a multifactorial disorder that cannot be explained by focusing solely on one lumbar compartment.
Study limitations
One of the limitations was the limited sample size. Also, depression and anxiety were not evaluated. Regarding strengths of the study, all the cases and their imaging scans were reviewed by the same radiologist.
Conclusion
Higher Pfirrmann grades correlated with increased ODI. No association was found between MRI grading in lumbosacral spine with pain intensity and most of the clinical parameters among persons with discogenic LBP. Chronic LBP is widely accepted to be a multifactorial disorder that cannot be contained within a single lumbar compartment. Clinician should not depend on MRI findings only in the diagnosis. History from the patient and clinical examination are particularly important to reach the final diagnosis. ODI might be convenient in achieving patient’s confidence and decreasing unnecessary investigation for them.
Availability of data and materials
All data generalized and/or analyzed during the current study are available from the principal author upon reasonable request.
Abbreviations
- BMI:
-
Body mass index
- GOTHI:
-
General Organization for Teaching Hospitals and Institutes
- IVD:
-
Intervertebral disc
- LBP:
-
Low back pain
- LSS:
-
Lumbosacral spine
- MRI:
-
Magnetic resonance image
- ODI:
-
Oswestry Disability Index
- SLR:
-
Straight leg raising
- VAS:
-
Visual analogue scale
- WC:
-
Waist circumference
References
Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M et al (2012) Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the global burden of disease study 2010. Lancet 380:2163–2196
Samartzis D, Karppinen J, Chan D, Luk KD, Cheung KM (2012) The association of lumbar intervertebral disc degeneration on magnetic resonance imaging with body mass index in overweight and obese adults: a population-based study. Arthritis Rheum 64:1488–1496
Samartzis D, Karppinen J, Cheung JP, Lotz J (2013) Disk degeneration and low back pain: are they fat-related conditions? Global Spine J 3(3):133
Takatalo J, Karppinen J, Niinimäki J, Taimela S, Näyhä S, Mutanen P, Sequeiros RB, Kyllönen E, Tervonen O (2011) Does lumbar disc degeneration on magnetic resonance imaging associate with low back symptom severity in young Finnish adults? Spine 36:2180–2189
Takatalo J, Karppinen J, Taimela S, Niinimäki J, Laitinen J, Sequeiros RB, Samartzis D, Korpelainen R, Näyhä S, Remes J, Tervonen O (2013) Association of abdominal obesity with lumbar disc degeneration—a magnetic resonance imaging study. PLoS One 8:56244
Fairbank JC, Pynsent PB (2000) The Oswestry disability index. Spine 25(22):2940–2952 discussion 52
Li Y, Fredrickson V, Resnick DK (2015) How should we grade lumbar disc herniation and nerve root compression? A systematic review (2015). Clin Orthop Relat Res 473(6):1896–1902
Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N (2001) Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine 26(17):1873–1878
Hawker GA, Mian S, Kendzerska T, French M (2011) Measures of adult pain. Visual analog scale for pain (vas pain), numeric rating scale for pain (nrs pain), mcgill pain questionnaire (mpq), short-form mcgill pain questionnaire (sf-mpq), chronic pain grade scale (cpgs), short form-36 bodily pain scale (sf-36 bps), and measure of intermittent and constant osteoarthritis pain (icoap). Arthritis Care Res 63(S11):S240–S252
Veresciagina K, Ambrozaitis V, Spakauskas B (2009) The measurements of health related quality-of-life and pain assessment in the preoperative patients with low back pain. Medicina (Kaunas) 45(2):111–122
Tonosu J, Takeshita K, Hara N, Matsudaira K, Kato S, Masuda K, Chikuda H (2012) The normative score and the cut-off value of the Oswestry disability index (ODI). Eur Spine J 21(8):1596–1602
Luoma K, Raininko R, Nummi P, Luukkonen R (1993) Is the signal intensity of cerebrospinal fluid constant? Intensity measurements with high and low field magnetic resonance imagers. Magn Reson Imaging 11(4):549–555
Pfirrmann CW, Dora C, Schmid MR, Zanetti M, Hodler J, Boos N (2004) MR image based grading of lumbar nerve root compromise due to disc herniation: reliability study with surgical correlation. Radiology 230:583–588
Cheung KM, Samartzis D, Karppinen J, Luk KD (2012) Are “patterns” of lumbar disc degeneration associated with low back pain? New insights based on skipped level disc pathology. Spine 37(7):E430–E438
Middendorp M, Vogl TJ, Kollias K, Kafchitsas K, Khan MF, Maataoui A (2017) Association between intervertebral disc degeneration and the Oswestry disability index. J Back Musculoskelet Rehabil 30(4):819–882
Kaadeh T, Rafeemanesh E, Omidi-Kashani F (2018) Investigating a possible link between MRI findings and clinical complaints in the patients with chronic low back pain. Austin J Orthopade Rheumatol 5(2):1070
Ravikanth R (2020) Magnetic resonance evaluation of lumbar disc degenerative disease as an implication of low back pain: a prospective analysis. Neurol India 68(6):1378–1384
Peterson CK, Bolton JE, Wood AR (2000) A cross-sectional study correlationg lumbar spine degeneration with disability and pain. Spine 25:218–223
Selvaraj R, Narayana GSJ, Ranganathan J, Anandan H (2017) Clinical correlation of magnetic resonance imaging with symptom complex in prolapsed intervertebral disc disease: a cross-sectional study. Int J Sci Study 5(5):261–265
Hangai M, Kaneoka K, Kuno S, Hinotsu S, Sakane M, Mamizuka N, Sakai S, Ochiai N (2008) Factors associated with lumbar intervertebral disc degeneration in the elderly. Spine J 8(5):732–740
Takatalo J, Karppinen J, Taimela S, Niinimäki J, Laitinen J, Blanco Sequeiros R, Paananen M, Remes J, Näyhä S, Tammelin T, Korpelainen R, Tervonen O (2013) Body mass index is associated with lumbar disc degeneration in young Finnish males: subsample of northern Finland birth cohort study 1986. BMC Musculoskelet Disord 14:87
Ibrahimi-Kaçuri D, Murtezani A, Rrecaj S, Martinaj M, Haxhiu B (2015) Low back pain and obesity. Mediev Archaeol 69(2):114–116
Goni VG, Hampannavar A, Gopinathan NR, Singh P, Sudesh P, Logithasan RK, Sharma A, Bk S, Sament R (2014) Comparison of the Oswestry disability index and magnetic resonance imaging findings in lumbar canal stenosis: an observational study. Asian Spine J 8(1):44–50
Arpinar VE, Gliedt JA, King JA, Maiman DJ, Muftuler LT (2020) Oswestry disability index scores correlate with MRI measurements in degenerating intervertebral discs and endplates. Eur J Pain 24(2):346–353
Hasanović-Vučković S, Jusufbegović M, Vegar-Zubović S, Milisic L, Sehic A, Hasanbegovic I, Beganovic A (2020) Assessment of lumbar spine disc degenerationin coherence to Pfirrmann grades and Oswestry disability index. J Health Sci 10(10):1–5
Bajpai J, Saini S, Singh R (2013) Clinical correlation of magnetic resonance imaging with symptom complex in prolapsed intervertebral disc disease: a cross-sectional doubleblind analysis. J Craniovertebr Junction Spine 4(1):16–20
Corniola M-V, Stienen MN, Joswig H, Smoll NR, Schaller K, Hildebrandt G, Gautschi OP (2016) Correlation of pain, functional impairment, and health related quality of life with radiological grading scales of lumbar degenerative disc disease. Acta Neurochir 158(3):499–505
Kohat AK, Kalita J, Ramanivas S, Misra UK, Phadke RV (2017) Clinical significance of magnetic resonance imaging findings in chronic low backache. Indian J Med Res 145:796–803
Singh R, Kumar P, Wadhwani J, Yadav RK, Khanna M, Kaur S (2021) A comparative study to evaluate disc degeneration on magnetic resonance imaging in patients with chronic low back pain and asymptomatic individuals. J Orthop Trauma Rehabilitation 28:1–7
Modic MT, Ross JS (1991) Magnetic resonance imaging in the evaluation of low back pain. Orthop Clin North Am 22:283–301
Garrido E (1993) Lumbar disc herniation in the pediatric patient. Neurosurg Clin N Am 4:149–152
Hamada SM, Abou-Zeid AH (2015) Clinical and surgical correlation with MRI findings in herniated lumbar disc: towards clinical and surgical application of the current classification. Egy Spine 14:32–45
Wani SK, Deshpande N (2014) Correlation of pain and disability with MRI findings in patients with lumbar discogenic back PAIN. Int J Physiother Res 2(2):418–423
Boden SD, Davis TS, Patronas NJ, Wiesel SW (1990) Abnormal magnetic resonance scans of the lumbar spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg Am 72:403–408
Kerr RS, Cadoux-Hudson TA, Adams CB (1988) The value of accurate clinical assessment in the surgical management of lumbar disc protrusion. J Neurol Neurosurg Psychiatry 51:169–173
Masui T, Yukawa Y, Nakamura S, Kajino G, Matsubara Y, Kato F, Ishiguro N (2005) Natural history of patients with lumbar disc herniation observed by magnetic resonance imaging for minimum 7 years. J Spinal Disord Tech 18(2):121–126
Acknowledgements
Not applicable.
Funding
The study had no funding from any resource.
Author information
Authors and Affiliations
Contributions
Idea of research, AOE. All authors shared in the design and methodology. Selection of patients and clinical examination, AOH and SIE. Interpretation of data and analysis by AOH, RAI, SIE, and SSE. Manuscript writing and editing were done by AOH and RAI. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted after the approval of the ethics committee of the General Organization for Teaching Hospitals and Institutes (GOTHI), with reference number HM000118. All patients in this study gave written informed consent to participate in this research. A written informed consent was obtained from all participants to contribute in this study.
Consent for publication
Not applicable.
Competing interests
The corresponding author is an associate editor in Egyptian Rheumatology and Rehabilitation journal, with no other competing interests. The other authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
El-Hady, A.O., El Molla, S.S., Elwan, S.I. et al. Evaluation of health related quality of life with the use of Oswestry disability index in degenerative discogenic low back pain. Egypt Rheumatol Rehabil 50, 4 (2023). https://doi.org/10.1186/s43166-022-00166-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43166-022-00166-6