Abstract
Background
Granulomatosis with polyangiitis (GPA) is a rare systemic vasculitis. Its severity ranges from indolent disease to fulminant that may cause death. With treatment, remission is seen in more than 80% of cases, although relapse is still common. There have been studies showing that there may be factors to predict relapse in GPA. Based on relapses, the decision to start treatment and/or to monitor the patients more closely is made. Therefore, predicting the relapse of GPA can be effective in controlling the disease. Our aim was to investigate possible factors for relapse in GPA.
We recruited 254 patients diagnosed with GPA who were under treatment at Alzahra hospital affiliated to Isfahan University of Medical Sciences (from 2013 to 2020) and Amir Alam Hospital affiliated to Tehran University of Medical Sciences (from 2020 to 2022) to plan a retrospective study. Chi-squared or Fisher’s exact tests were performed to compare categorical variables, while the Mann–Whitney U test was used to compare continuous variables.
Results
Analysis of our patients (aged 20–80,122 females) showed that 147 patients (57.9%) experienced relapse. Mean age in relapse group was 43.8 ± 16.6 and in no-relapse group was 45.6 ± 15.1 (P > 0.05). Among many potential predictors, we observed in multivariate analysis that positive PR3-ANCA (proteinase 3-antineutrophilic cytoplasmic antibodies) (P = 0.007, OR:2.62,CI:1.29–5.31),nose manifestations (P = 0.004, OR 3.00, CI 1.43–6.26), mucosal membranes involvement (P = 0.009, OR 4.21, CI 1.43–12.38), and gastrointestinal tract (GI) complications (P = 0.03, OR 5.64, CI 1.14–27.90) were significant predictors of GPA relapse.
Conclusion
Among clinical and laboratory features we studied, positive PR3-ANCA, nose manifestations, mucosal membranes involvement, and GI complications were independent predictors of relapse in patients with GPA.
Similar content being viewed by others
Background
Granulomatosis with polyangiitis (GPA) (Wegener’s granulomatosis), is a rare systemic vasculitis that causes inflammation of wall of small vessels and peri- and extravascular granulomatosis [1]. It predominantly manifests at the upper and lower respiratory tracts and kidneys but impairment of multiple organ systems is possible [2,3,4,5,6,7,8]. The severity of the disease ranges from indolent disease which involves only one site to fulminant and multi-organ vasculitis that may cause death [3]. The so-called classical triad of GPA includes sinusitis, pneumonia and glomerulonephritis [8]. Many features of the disease may be lacking at first, but may evolve after initial presentation [4,5,6]. It may be fatal if left untreated but current therapies can cure it in most cases, although relapses are common [2].
The annual incidence of the disease is estimated as 4–21 cases per million [9,10,11,12]. The peak incidence is seen in 4–7th decades of life [5,6,7, 13]. Men and women are equally affected [14]. Although the etiology of GPA remains unknown, studies have shown that the roles of genetic, immunologic, environmental factors, and microbial pathogens have been influential [15]. GPA is usually associated with antibodies against neutrophils (antineutrophilic cytoplasmic antibodies (ANCA)) and so the disease is a component of a spectrum of disorders entitled the ANCA-associated vasculitides (AAVs) [3, 16, 17]. AAVs are associated with ANCA specific for myeloperoxidase (MPO-ANCA) or proteinase 3 (PR3-ANCA) which are found in the azurophilic granules in neutrophils [2, 18].
The presence of ANCAs is a critical component to its diagnosis and it is highly specific, so positive ANCAs is of high diagnostic value [19]. Treatment options are chosen based on extent, acuity, sites, and severity of the disease [20]. Objective criteria are important to assess disease activity and response to therapy, and The Birmingham Vasculitis Activity Score (BVAS) is a valid index for this purpose [21]. Studies show that using immunosuppressants combined with corticosteroids fundamentally improves the prognosis of GPA [14, 22,23,24]. With treatment, remission is seen in more than 80% of cases, although relapse is still common (happens in more than 50% of cases) [25].
There have been studies showing that there may be factors to predict relapse in GPA. For example, some studies showed that ear, nose, and throat (ENT) involvement is associated with more relapses [26]. Presence of PR3-ANCA and cardiac involvement at the time of diagnosis, are other factors associated with increased risk of relapsing [27]. During the course of GPA, persistent ANCAs is associated with relapse too [28,29,30]. Disappearance of ANCAs, means there will be no relapse [27]. A number of studies have shown that relapses are much more common in patients with positive PR3-ANCA than in those with positive MPO-ANCA [31]. Based on these relapses and predicting factors, the decision to start treatment and/or to monitor the patients more closely is made [1]. Therefore, predicting the relapse of GPA can be effective in controlling the disease. Here, we retrospectively investigated possible factors for relapse in GPA in patients who presented to our hospitals and we analyzed the relationships between these factors and clinical manifestations.
Methods
After institutional ethics approval, we recruited 254 patients (age > 20 years) diagnosed with GPA and were under treatment at Alzahra Hospital affiliated to Isfahan University of Medical Sciences, Isfahan, Iran (from 2013 to 2020) and Amir Alam Hospital affiliated to Tehran University of Medical Sciences, Tehran, Iran (from 2020 to 2022) to plan a retrospective multi-center study. The diagnosis was established based on American College of Rheumatology and Revised International Chapel Hill Consensus criteria 2012 for the classification of GPA [32,33,34]. Inclusion criteria consisted of patients diagnosed as GPA using the criteria we mentioned earlier, who were followed more than 12 months. Exclusion criteria include patients with other autoimmune or neurologic or skin diseases, cancer, active, or chronic infection and abnormal thyroid function tests. All patients’ data were collected from medical records.
We recorded following data for the study: demographic features (gender, age, age at diagnosis of GPA), positive or negative MPO-ANCA and PR3-ANCA results, BVAS at diagnosis of patients, involved organs at initial referral and during the course of the disease and GPA relapses. A state of relapse was defined as (1) occurrence of new involvement, (2) recurrence or worsening of clinical manifestations of vasculitis [35].
Nose involvement was considered as presence of rhinitis, nasal ulcer, epistaxis, epithelial perforation, and polyp of nose. Sinus involvement included sinusitis, mastoiditis, erosion, and sclerosis of sinuses. Ear manifestations were determined as conductive hearing loss and sensory-neural hear loss. Lung involvement was considered as wheezing, hemoptysis, infiltration, ground glass opacity in CT-scan, alveolar hemorrhage, nodular cavity, effusion, atelectasis, bronchiolitis, bronchiectasis, interstitial lung disease, infarction, and endo-bronchial involvement. Kidney complications were considered as proteinuria, hematuria, and creatinine ≥ 1.4 mg/dL. Eye complications included episcleritis, scleritis, dacryocistitis, proptosis, petosis, cellulitis, blurred vision, visual loss, conjunctivitis, vasculitis, keratitis, and uveitis. Central nervous system (CNS) involvement considered as cranial nerve involvements, loss of consciousness, seizure, meningitis, and encephalitis. We included oral ulcer, salivary involvement, and genital ulcer as mucosal membrane involvement. Skin problems were skin ulcer, digital gangrene, and skin vasculitis. Pericardial effusion, cardiac thrombophlebitis, and heart failure were as heart involvement. GI complications included GI effusion, GI ischemia, pancreas involvement, splenomegaly, hepatomegaly, and hepatitis. Test results for biomarkers were collected for each patient at diagnosis: ANCAs titer, anti-PR3, and MPO antibody levels. For ANCA, indirect immunofluorescence (IIF) and for anti-PR3 and anti-MPO antibody levels, enzyme-linked immunosorbent assay (ELISA) was used. For ANCA IIF, serum samples were examined using INOVA neutrophil-coated slides.
We used SPSS (Statistical Package for the Social Sciences V. 26, IBM Corporation) for statistical analysis. The quantitative and categorical data were expressed as mean ± standard deviation and frequency and percentage, respectively. Statistical analysis was performed by chi-squared or Fisher’s exact tests to compare categorical variables, while the Mann–Whitney U test was used to compare continuous variables between groups. Variables with P ≤ 0.01 in the univariate analysis were entered into multivariable logistic regression analysis (binary logistic regression), odds ratio (OR), and 95% confidence interval for OR were reported. We also used receiver operating characteristic curve (ROC) to examine the best cutoff value of BVAS at diagnosis and reported the sensitivity, specificity, along with area under the curve (AUC) with 95% confidence interval (95% CI). P ≤ 0.05 was chosen as statistically significant.
Results
Mean diagnosis age in this study was 44.6 ± 16.2 and 48.0% of patients were women (n = 122). One hundred seven patients had no relapse (42.1%) and others experienced it at least once. Mean follow-up duration was 40.1 ± 22.1 months. Our patients had initial presentations as the following: ninety-five patients with ear (37.4%), 75 patients with nose (29.5%), 72 patients with sinus (28.3%), 11 patients with subglottal (4.3%), 17 patients with eye (6.7%), 5 patients with 7th nerve (2.0%), 16 patients with lung (6.3%), 1 patient with kidney (0.4%), 2 patients with skin (0.8%) manifestations, and 1 patient (0.4%) with arthritis.
One hundred sixty-two patients had initial presentation of cerebrovascular complications, 128 of them had left side of cerebral vessels involvement (79.0%), and others had right sided complications (n = 34, 21.0%). We also studied pseudotumors. Sixty-two patients had pseudotumor of different organs (24.4%). The most common organs having pseudotumor were eye (n = 24, 38.7%), nose (n = 9, 14.5%), sinus (n = 7, 11.3%), and nasopharynx (n = 5, 8.0%).
Thirty-six patients had positive MPO-ANCA (14.2%) and 163 patients had positive PR3-ANCA (64.2%). Ten patients had eosinophilia (3.9%). Biopsy was done for 168 patients (66.1%). Mean BVAS at diagnosis was 15.8 ± 7.7.
We also checked to see what organs were involved during admission and/or follow-up. Involved organs were as following: nose (n = 188, 74%), sinus (n = 238, 93.7%), glottal (n = 39, 15.4%), ear (n = 171, 67.3%), lung (n = 194, 76.4%), kidney (n = 117, 46.1%), eye (n = 82, 32.3%), CNS (n = 81, 31.9%), mucosal membranes (n = 35, 13.8%), skin (n = 30, 11.8%), heart (n = 10, 3.9%), GI (n = 19, 7.5%), and arthritis (n = 19, 7.5%).
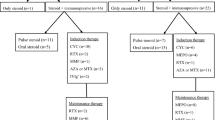
We performed univariate analysis for the disease relapse. Variables associated with this relapse with P ≤ 0.01 were as following: patients with initial presentation with lung manifestations (P = 0.01), initial presentation with nose manifestations (P = 0.03), initial presentation with sinus involvement (P = 0.07), positive PR3-ANCA and MPO-ANCA (respectively: P = < 0.001, P = 0.001), eosinophilia (P = 0.07), BVAS at diagnosis (P < 0.001), nose manifestations (P = 0.05), mucosal membranes involvement (P = 0.001), eye involvement (P = 0.08), skin manifestations (P = 0.05), heart involvement (P = 0.03), GI complication (P = 0.002), and arthritis (P = 0.01). We entered these variables in multivariate binary logistic regression. Results showed that patients with nose, mucosal membranes, GI involvement, and positive PR3-ANCA, were more likely to experience relapse for GPA. Although patients with initial presentation of nose involvement had less chance to experience relapse. It is worth to mention that ROC analysis’ results showed that the best cutoff for BVAS at diagnosis was 8.5 and if BVAS ≥ 8.5, it differentiates significantly patients with relapse from non-relapse (P < 0.001, sensitivity = 88.4%, specificity = 76.6%, AUC 0.641, CI 0.573–0.709), but it was not a predictor in multivariate analysis (Tables 1 and 2; Fig. 1).
Discussion
This multi-center study investigated relapse and factors affecting it in 254 patients who were diagnosed with GPA. Although a marked improvement was achieved in mortality and relapses area, the GPA relapse is still common [2, 25]. Relapse rate was higher in our study than those reported by Tufan et al. (2020, in Turkey) and Hogan et al. (2005, USA) (respectively: 58% vs. 46% and 42%) [36, 37]. We could think of two reasons why this relapse rate was more in our study: first, greater accuracy in registration of patients’ files that helped to record more patients with relapses. Second, patients’ cooperation in the treatment could be inappropriate. Treatment regimens in our centers were compatible with standard and update algorithms and guidelines, so we do not think of it as a reason about this issue.
Charles et al., Boomsma et al., and Hogan et al. identified PR3-ANCA and MPO-ANCA as factors for relapse [18, 37, 38] but patients with positive PR3-ANCA were more likely to relapse [18]. Boomsma et al. studied 100 patients with GPA (85 with PR3-ANCA, 15 with MPO-ANCA) prospectively from 1996 to 1998. Disease activity was assessed without knowledge of the ANCA levels, and they concluded that serial measurement of ANCA levels is valuable for early prediction of relapses in patients with GPA [38]. On the other hand, Hogan et al. studied 350 patients who received a new diagnosis of ANCA associated vasculitis between 1985 and 2003. They concluded that increased risk for relapse appears to be related to the presence of anti-PR3 and anti-MPO antibodies seropositivity [37]. We showed that PR3-ANCA was able to predict the relapse.
Naomi et al. studied 121 patients’ data in Japan and concluded that GI involvement was associated with relapse, like we could show [39]. We did not find any study to survey nose manifestations alone and mucosal membranes involvement as factors for relapse of the GPA. However, there are studies that have shown that ENT involvement could be a predicting factor for the relapse [26]. By contrast, Yoo et al. performed a study on 30 patients with GPA and concluded that ENT manifestations were in favor with the disease remission [33]. We, in this study, have shown that nose and mucosal membranes involvement were predicting factors for relapse. So, we could introduce novel variables to be more studied in the future to see whether they play a role in predicting relapse. It is worth to mention that, patients who referred to our hospitals with initial presentation of nose involvement, were less probable to encounter relapse in future, but patients whose nose manifestations were diagnosed during follow-ups, were more probable to experience relapse. We suggest more studies to be done to survey if initial presentation with nose manifestation could be a preventing factor for relapse.
Pagnoux et al. and Hogan et al., found that lung involvement is a predictor of relapse [37, 40]. However, Tufan et al. and Despujol et al., like our study, found that lung involvement is not a factor for relapse [36, 41]. A review of four studies reported that cardiovascular involvement is a risk factor for relapse [42]. Despujol et al. and Koldingsnes et al. have also shown that heart involvement causes increased risk of relapse [41, 43]. By contrast, we did not find heart involvement as a predictor for relapse. In a study which was done by Lega et al., unlike ours, skin involvement was shown to be a risk factor of relapse [44]. By contrast, Outh et al. found that relapse frequency was less in patients with skin involvement. They studied 99 patients diagnosed with AAV between 1990 and 2015 experiencing at least one relapse. They concluded that patients without relapse tended to have cutaneous manifestations more often than patients with relapse [45].
In a study that Hosokawa et al. done on 36 patients in Japan from 2013 to 2018, ear involvement was a factor to predict relapse, but we could not show this factor to be a predictor [35]. Despujol et al. conducted a randomized trial on 174 patients in 2010, one of the findings they concluded was about kidney involvement and that it is not a factor for relapse [41], like we showed. Despujol et al. and Tufan et al., like us, showed that there was no difference in eye complication between relapse group and no-relapse group [36, 41]. As Despujol et al. had mentioned, CNS involvement could not be a predictor, like we showed in our study [41]. Yoo et al. conducted a study on 30 patients in 2017 in Korea and showed that BVAS for GPA ≥ 9.5 was an independent predictor of refractory disease during follow-up [46]. Mehrabi Nejad et al. studied 133 patients from 2012 to 2021 and concluded that Patients with BVAS > 12 are more vulnerable to relapsing disease [47]. Although we were able to show a statistically significant cutoff for BVAS at diagnosis by ROC curve (8.5), but it was not a predictor in multivariate analysis. We think the reason why it was not statistically significant is that we didn’t find data of BVAS at follow up. With follow-up BVASs, maybe we could show this conclusion, too.
The main strength of our study was being a multi-center research with a proper number of patients included. Our study has a limitation, which is that it was a retrospective study that could be limited by the quality and inaccuracy in data reporting. This study identified several predictors of GPA relapse. We suggest that patients with these risk factors should be monitored carefully and closely for relapse. This different course of the disease may help to customize different treatment regimens. Also, focusing on a patient’s clinical features may be more practical than assigning a specific disease diagnosis when estimating risk for relapse.
Conclusion
Among clinical and laboratory features we studied, positive PR3-ANCA, nose manifestations, mucosal membranes involvement, and GI complications were independent predictors of relapse in patients with GPA. We suggest future studies that patients with these risk factors should be monitored carefully and closely for relapse.
Availability of data and materials
Data and material are included.
Abbreviations
- GPA:
-
Granulomatosis with polyangiitis
- GI:
-
Gastrointestinal tract
- ANCA:
-
Antineutrophilic cytoplasmic antibodies
- PR3:
-
Proteinase 3
- MPO:
-
Myeloperoxidase
- AAV:
-
ANCA-associated vasculitis
- BVAS:
-
The Birmingham Vasculitis Activity Score
- ENT:
-
Ear, nose, and throat
References
Puéchal X (2020) Granulomatosis with polyangiitis (Wegener’s). Joint Bone Spine 87(6):572–578. https://doi.org/10.1016/j.jbspin.2020.06.005
Witko-Sarsat V, Thieblemont N (2018) Granulomatosis with polyangiitis (Wegener granulomatosis): A proteinase-3 driven disease? Joint Bone Spine 85(2):185–189. https://doi.org/10.1016/j.jbspin.2017.05.004
Lynch JP 3rd et al (2018) Granulomatosis with Polyangiitis (Wegener’s Granulomatosis): Evolving Concepts in Treatment. Semin Respir Crit Care Med 39(4):434–458. https://doi.org/10.1055/s-0038-1660874
Lynch JP III, White E, Tazelaar H, Langford CA (2004) Wegener’s granulomatosis: evolving concepts in treatment. Semin Respir Crit Care Med 25(05):491–521
Hoffman GS, Kerr GS, Leavitt RY et al (1992) Wegener granulomatosis: an analysis of 158 patients. Ann Intern Med 116(06):488–498
Reinhold-Keller E, Beuge N, Latza U et al (2000) An interdisciplinary approach to the care of patients with Wegener’s granulomatosis: long-term outcome in 155 patients. Arthritis Rheum 43(05):1021–1032
Abdou NI, Kullman GJ, Hoffman GS et al (2002) Wegener’s granulomatosis: survey of 701 patients in North America. Changes in outcome in the 1990s. J Rheumatol 29(02):309–316
Heitkötter B et al (2018) Granulomatosis with polyangiitis (Wegener’s granulomatosis): a rare variant of sudden natural death. Int J Legal Med. 132(1):243–248
Watts RA, Gonzales-Gay MA, Garcia-Porrua C, Lane SE, Bentham G, Scott DG (2001) Geoepidemiology of systemic vasculitis: comparison of the incidence in two regions of Europe. Ann Rheum Dis 60(02):170–172
Watts RA, Lane SE, Bentham G, Scott DG (2000) Epidemiology of systemic vasculitis: a ten-year study in the United Kingdom. Arthritis Rheum 43(02):414–419
Koldingsnes W, Nossent H (2000) Epidemiology of Wegener’s granulomatosis in northern Norway. Arthritis Rheum 43(11):2481–2487
Pearce FA, Grainge MJ, Lanyon PC, Watts RA, Hubbard RB (2017) The incidence, prevalence and mortality of granulomatosis with polyangiitis in the UK Clinical Practice Research Datalink. Rheumatology (Oxford) 56(04):589–596
Cotch MF, Hoffman GS, Yerg DE, Kaufman GI, Targonski P, Kaslow RA (1996) The epidemiology of Wegener’s granulomatosis. Estimates of the five-year period prevalence, annual mortality, and geographic disease distribution from population-based data sources. Arthritis Rheum 39(01):87–92
Binda V, Moroni G, Messa P (2018) ANCA-associated vasculitis with renal involvement. J Nephrol 31(02):197–208
Sfiniadaki E et al (2019) Ocular manifestations of granulomatosis with polyangiitis: a review of the literature. Ophthalmol Ther 8(2):227–234. https://doi.org/10.1007/s40123-019-0176-8
Banerjee P et al (2021) Epidemiology and genetics of granulomatosis with polyangiitis. Rheumatol Int 41(12):2069–2089. https://doi.org/10.1007/s00296-021-05011-1
Garlapati, Priyatha. and Ahmad Qurie. Granulomatosis with Polyangiitis. StatPearls, StatPearls Publishing, 7 December 2021.
Jennette JC, Nachman PH (2017) ANCA glomerulonephritis and vasculitis. Clin J Am Soc Nephrol 12(10):1680–1691. https://doi.org/10.2215/CJN.02500317
Iudici M et al (2021) Granulomatosis with polyangiitis: Study of 795 patients from the French Vasculitis Study Group registry. Sem Arthritis Rheum 51(2):339–346. https://doi.org/10.1016/j.semarthrit.2021.02.002
Exley AR, Bacon PA, Luqmani RA, Kitas GD, Carruthers DM, Moots R (1998) Examination of disease severity in systemic vasculitis from the novel perspective of damage using the vasculitis damage index (VDI). Br J Rheumatol 37(01):57–63
Stone JH, Hoffman GS, Merkel PA et al (2001) International Network for the Study of the Systemic Vasculitides (INSSYS). A diseasespecific activity index for Wegener’s granulomatosis: modification of the Birmingham Vasculitis Activity Score. Arthritis Rheum 44(04):912–920
Fauci AS, Haynes BF, Katz P, Wolff SM (1983) Wegener’s granulomatosis: prospective clinical and therapeutic experience with 85 patients for 21 years. Ann Intern Med 98(01):76–85
Hoffman GS (1994) Wegener’s granulomatosis: the path traveled since 1931. Medicine (Baltimore) 73(06):325–329
Fauci AS, Wolff SM (1973) Wegener’s granulomatosis: studies in eighteen patients and a review of the literature. Medicine (Baltimore) 52(06):535–561
Puéchal X, Pagnoux C, Perrodeau E, Hamidou M, Boffa JJ, Kyndt X et al (2016) Long-term outcomes among participants in the WEGENT trial of remission-maintenance therapy for granulomatosis with polyangiitis (Wegener’s) or microscopic polyangiitis. Arthritis Rheumatol 68:690–701
Guillevin L, Lhote F, Gayraud M et al (1996) Prognostic factors in polyarteritis nodosa and Churg-Strauss syndrome. A prospective study in 342 patients. Medicine (Baltimore) 75:17–28
Mukhtyar C, Flossmann O, Hellmich B et al (2008) Outcomes from studies of antineutrophil cytoplasm antibody associated vasculitis: a systematic review by the European League Against Rheumatism systemic vasculitis task force. Ann Rheum Dis 67:1004–1010
Karras A, Pagnoux C, Haubitz M, de Groot K, Puéchal X, Cohen JW et al (2017) Randomised controlled trial of prolonged treatment in the remission phase of ANCA-associated vasculitis. Ann Rheum Dis 76:1662–1668
Morgan MD, Szeto M, Walsh M, Jayne D, Westman K, Rasmussen N et al (2017) Negative anti-neutrophil cytoplasm antibody at switch to maintenance therapy is associated with a reduced risk of relapse. Arthritis Res Ther 7(19):129
Terrier B, Pagnoux C, Perrodeau E, Karras A, Khouatra C, Aumaître O et al (2018) for the French Vasculitis Study Group. Long-term efficacy of remission-maintenance regimens for ANCA-associated vasculitides. Ann Rheum Dis 77:1150–6
Cornec D et al (2016) ANCA-associated vasculitis—clinical utility of using ANCA specificity to classify patients. Nat Rev Rheumatol 12(10):570–579
Zimba O et al (2021) Challenges in diagnosis of limited granulomatosis with polyangiitis. Rheumatol Int 41(7):1337–1345. https://doi.org/10.1007/s00296-021-04858-8
Yoo J, Kim HJ, Ahn SS, Jung SM, Song JJ, Park YB, Lee SW (2018) The utility of the ACR/EULAR 2017 provisional classification criteria for granulomatosis with polyangiitis in Korean patients with antineutrophil cytoplasmic antibody-associated vasculitis. Clin Exp Rheumatol 36(2):85–87
Jennette JC, Falk RJ, Bacon PA, Basu N, Cid MC, Ferrario F et al (2013) 2012 revised international Chapel Hill consensus conference nomenclature of vasculitides. Arthritis Rheum 65:1–11
Hosokawa Y et al (2021) The association between ear involvement and clinical features and prognosis in ANCA-associated vasculitis. Auris, Nasus, Larynx. 48(5):885–889. https://doi.org/10.1016/j.anl.2021.01.023
Tufan MA et al (2021) Factors affecting relapse in patients with Granulomatosis Polyangiitis: a single-center retrospective cohort study. Turkish J Med Sci 4:1719–1726. https://doi.org/10.3906/sag-2008-217
Hogan SL, Falk RJ, Chin H, Cai J, Jennette CE et al (2005) Predictors of relapse and treatment resistance in antineutrophil cytoplasmic antibody-associated small-vessel vasculitis. Ann Intern Med 143(9):621–631. https://doi.org/10.7326/0003-4819-143-9-200511010-00005
Boomsma MM, Stegeman CA, van der Leij MJ et al (2000) Prediction of relapses in Wegener’s granulomatosis by measurement of antineutrophil cytoplasmic antibody levels: a prospective study. Arthritis Rheum 43:2025–2033
Tsurikisawa N et al (2017) Longterm prognosis of 121 patients with eosinophilic granulomatosis with polyangiitis in Japan. J Rheumatol. 44(8):1206–1215. https://doi.org/10.3899/jrheum.161436
Pagnoux C, Hogan SL, Chin H, Jennette JC, Falk RJ et al (2008) Predictors of treatment resistance and relapse in antineutrophil cytoplasmic antibody-associated small-vessel vasculitis: comparison of two independent cohorts. Arthritis Rheum 58(9):2908–2918. https://doi.org/10.1002/art.23800
Pierrot-DeseillignyDespujol C et al (2010) Predictors at diagnosis of a first Wegener’s granulomatosis relapse after obtaining complete remission. Rheumatology (Oxford, England) 49(11):2181–90. https://doi.org/10.1093/rheumatology/keq244
Walsh M, Flossmann O, Berden A, Westman K, Höglund P et al (2012) Risk factors for relapse of antineutrophil cytoplasmic antibody-associated vasculitis. Arthritis Rheumatol 64(2):542–548. https://doi.org/10.1002/art.33361
Koldingsnes W, Nossent JC (2003) Baseline features and initial treatment as predictors of remission and relapse in Wegener’s granulomatosis. J Rheumatol 30:80–88
Lega JC, Seror R, Fassier T, Aumaître O, Quere I et al (2014) Characteristics, prognosis, and outcomes of cutaneous ischemia and gangrene in systemic necrotizing vasculitides: a retrospective multicenter study. Semin Arthritis Rheum 43(5):681–688. https://doi.org/10.1016/j.semarthrit.2013.09.001
Outh R, Lemaire A, Mania A, Berland P, Gerbaud L et al (2020) Relapses in patients with anti-neutrophil cytoplasmic antibody-associated vasculitis: a retrospective study. Clin Rheumatol 39(5):1601–1608. https://doi.org/10.1007/s10067-019-04816-7
Yoo J et al (2017) Birmingham vasculitis activity score of more than 9.5 at diagnosis is an independent predictor of refractory disease in granulomatosis with polyangiitis. Int J Rheum Dis 20(10):1593–1605. https://doi.org/10.1111/1756-185X.13144
Nejad MMM et al (2022) Predicting factors for relapse in patients with granulomatosis with polyangiitis: results from a long-term cohort. Clin Rheumatol 41(8):2457–2465. https://doi.org/10.1007/s10067-022-06159-2
Acknowledgements
We gratefully thank Isfahan University of Medical Sciences and Tehran University of Medical Sciences for the support.
Funding
This work was supported solely by institutional and departmental sources.
Author information
Authors and Affiliations
Contributions
Sara Safari: writing and data collection. Samira Alesaeidi: writing and edition, suggesting the idea, and responsible for conceptualization. Bahram Pakzad: writing and edition. Sina Abbaspour: statistical analysis and edition. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval (IR.MUI.MED.REC.1399.299, 8/12/2020) and consent to participate were established.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Safari, S., Alesaeidi, S., Pakzad, B. et al. Predictors of relapse in granulomatosis with polyangiitis: a multi-center study. Egypt Rheumatol Rehabil 49, 59 (2022). https://doi.org/10.1186/s43166-022-00160-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43166-022-00160-y