Abstract
Background
Severe coronavirus disease 2019 (COVID-19) infections are associated with increased levels of C-reactive protein (CRP) and several pro-inflammatory cytokines leading to cytokine storm. Vitamin D has been proved to be associated with biological activities of the innate and adaptive immune systems. There is a growing number of data showing an association between serum vitamin D level and the different clinical outcomes of COVID-19 infection. Our aim is to evaluate the relation between serum vitamin D levels and the severity and mortality of COVID-19 infection in an Egyptian cohort.
Results
The study included 80 COVID-19 patients, 38 males (47.5%) and 42 females (52.5%), with a mean age of 52 ± 11.4 years (18–80 years). The serum vitamin D levels ranged between 2 and 30 ng/mL with a mean of 12.05 ± 9.04. Patients who were intubated had the lowest levels of serum vitamin D (7.26 ng/ml ± 5.21), while patients who had no need for oxygen supply had the highest levels (20.00 ng/ml ± 9.23) (P = 0.025). A highly significant negative correlation was found between serum vitamin D level and each of CRP and serum ferritin (r = − 0.346 and − 0.313) (P = 0.002 and 0.005). Of the enrolled 80 patients, 63 (79%) recovered (group 1) and 17 (21%) died (group 2). Group 2 had significantly lower vitamin D levels (6.17 ng/mL ± 3.22) and hemoglobin (10.75 ± 1.74) than group 1 patients (13.63ng/mL ± 9.46) (12.10 ± 1.85) (P = 0.002 and 0.009 respectively).
Conclusion
Serum vitamin D levels are significantly lower in patients needing mechanical ventilation, and in deceased patients, and are inversely related to the inflammatory markers CRP and serum ferritin, suggesting a relation between vitamin D insufficiency and poor COVID-19 outcome.
Similar content being viewed by others
Background
The coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was first reported in the city of Wuhan (China) in December 2019 and was declared a global pandemic by the World Health Organization (WHO) on March 11, 2020 [1].
Over the following months, COVID-19 has placed a huge burden on healthcare systems worldwide, posing serious threats to global health. Older age and underlying comorbid conditions have emerged as major risk factors for mortality related to COVID-19 [2]. Patients with severe manifestations of COVID-19 exhibit significantly increased circulating levels of C-reactive protein and several pro-inflammatory cytokines and chemokines that all lead to cytokine storm and eventually death [3].
Over the last decade, vitamin D has been proved to be associated with the biological activities of the innate and adaptive immune systems, as well as induction of the anti-inflammatory pathways in response to different pathogens [4]. Vitamin D deficiency represents a global pandemic, affecting individuals across all age groups worldwide. There is a growing number of data showing an association between serum 25-hydroxyvitamin D level and the different clinical outcomes of COVID-19 infection, particularly the related severity and mortality [5].
The aim of this study was to evaluate the relation between serum vitamin D and severity and mortality of COVID-19 infection in an Egyptian cohort.
Methods
Eighty COVID-19 patients were randomly recruited from the wards and the intensive care units (ICU) of the Ain Shams University Hospitals including the El Medany Hospital, El Demerdash Hospital, and El Obour Specialized Hospital. Approval was taken from the Ethical Committee of Scientific Research, Ain Shams University. After giving their informed written consent, patients were enrolled in this cross-sectional observational study during the period between June 2021 and December 2021.
All recruited patients were confirmed COVID-19 cases who had a positive result on real-time reverse transcriptase-polymerase chain reaction (RT-PCR) of nasopharyngeal and oropharyngeal swab specimens. Patients with malignancy, chronic kidney disease, chronic liver disease, parathyroid disease, current use of vitamin D or calcium supplements, pregnancy, and obesity were excluded.
All patients were subjected to detailed medical history with emphasis on symptoms of COVID-19 besides associated medical comorbidities (hypertension, diabetes, ischemic heart diseases, and chronic obstructive pulmonary diseases (COPD)). Clinical assessment of each participant was done as well as recording the need and type of oxygen supply and the fate of the disease either recovery or mortality. To study the relation between vitamin D levels and mortality, patients were divided into 2 groups. Group 1 included patients who recovered from COVID-19 infection, and group 2 included the deceased patients. Comparison was done between both groups as regards laboratory data and serum vitamin D level.
Laboratory tests included complete blood count (CBC), C-reactive protein (CRP), serum ferritin, D-dimer, serum calcium, serum phosphorus, renal function tests (blood urea nitrogen (BUN) and creatinine), liver enzymes (alanine aminotransferase (ALT), and aspartate aminotransferase (AST)). Serum 25-hydroxycholecalciferol level was measured for all the participants on hospital admission. Blood samples were collected in anticoagulant-free tubes. Immediate centrifugation (3500 rpm) for 20 min at +4C and serum was stored at – 20 °C until analysis. Serum vitamin D levels were measured by automated competitive electrochemiluminescence protein binding assay method with an autoanalyzer (Beckman Coulter in DXI 800).
All patients underwent non-contrast-enhanced chest computed tomography (CT) that assessed the COVID-19 Reporting and Data System (CO-RADS) grading score. CO-RADS score grades the level of suspicion of pulmonary involvement of COVID-19 infection as follows:
CO-RADS 1: COVID-19 is highly unlikely, CT is normal, or there are findings indicating a non-infectious disease. CO-RADS 2: the level of suspicion of COVID-19 infection is low, and CT findings are consistent with other infections. CO-RADS 3: COVID-19 infection is unsure or indeterminate, and CT abnormalities indicate infection but are unsure whether COVID-19 is involved. CO-RADS 4: the level of suspicion is high, and most CT findings are suspicious but not extremely typical as unilateral ground glass, confluent, or multifocal consolidations without a typical location or any other typical findings. CO-RADS 5: the level of suspicion is high with typical CT findings [6].
Statistical analysis
Data were entered to the Statistical Package for Social Science (SPSS) version 20. Qualitative data were presented as number and percentages, while quantitative data were presented as mean, standard deviations, and ranges. The comparison between 2 groups with qualitative data were done using chi-square test, and Fisher exact test was used when the expected count in any cell was < 5. The comparison between 2 quantitative data with parametric distribution was done using independent T-test. P-value ≤ 0.05 was considered significant.
Results
The current study included 80 COVID-19 patients, 38 males (47.5%) and 42 females (52.5%), with a mean age of 52 ± 11.4 (18–80 years). Participants had different pre-existing comorbidities; 40 patients (50%) were diabetic, 41 patients (51.25%) were hypertensive, 16 patients (20%) had ischemic heart disease, and 13 patients (16.25%) had COPD. Chest CT revealed a CO-RADS 3 stage in 34 patients (42.5%), 25 patients (31.25%) had CO-RADS 4, and 21 patients (26.25%) had CO-RADS 5.
Of the enrolled patients, 23.75% were intubated, 30% were on nasal oxygen, 35% needed different modes of non-invasive oxygen therapy, and 11% did not need any oxygen therapy. Laboratory data of the included patients are shown in Table 1.
The serum vitamin D levels of the enrolled COVID-19 patients ranged between 2 and 30 ng/mL with a mean of 12.05 ± 9.04. Serum vitamin D levels did not differ significantly in males and females (P = 0.58) nor in patients with different comorbidities. Although patients with different grades of CO-RADS staging on chest CT did not have significantly different levels of serum vitamin D level (P = 0.28), patients with CORAD 5 had the lowest vitamin D levels.
A significant difference of serum vitamin D level was found in patients on different modes of oxygen supply. Patients who were intubated (critical COVID-19 patients) had the lowest levels of serum vitamin D (7.26 ng/ml ± 5.21), while patients who had no need for oxygen supply (non-severe COVID-19) had the highest levels (20.00 ng/ml ± 9.23) (P = 0.025) (Table 2).
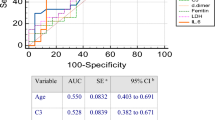
A highly significant negative correlation was found between serum vitamin D level and each of CRP (Fig. 1), serum ferritin (Fig. 2), and alkaline phosphatase (r = − 0.346, − 0.313, and − 0.343, P = 0.002, 0.005, and 0.002 respectively).
Patients were divided into two groups according to the fate of COVID-19 illness. Of the enrolled 80 patients, 63 (79%) recovered (group 1) and 17 (21%) died (group 2). Gender did not affect the survival; 53% of the deceased patients were males, while 47% were females. The mean age of group 1 patients (50 ± 11 years) was not significantly lower than that of group 2 patients (52 ± 11 years). Mortality was not significantly affected by different comorbidities in the enrolled patients as shown in Table 3.
Group 2 patients who did not survive had significantly lower vitamin D levels (6.17ng/mL ± 3.22) and hemoglobin (10.75 ± 1.74) than group 1 patients (13.63 ng/mL ± 9.46) (12.10 ± 1.85) (P = 0.002 and 0.009 respectively). In addition, group 2 patients had significantly higher levels of white blood cell count (WBCs), BUN, and alkaline phosphatase than group 1 patients (P = 0.008, 0.002, and 0.031 respectively) (Table 1).
Discussion
During the COVID-19 pandemic period, researchers focus on deep survey of the modifiable factors which can reduce the severity of the COVID-19 infection. Vitamin D is known to play a key role in modulation of the immune response in infectious diseases. Different studies showed that severity of COVID-19 infection is directly related to vitamin D level [5, 7,8,9,10,11,12,13].
The current study included 80 COVID-19 hospitalized patients and investigated the relationship between serum vitamin D levels and the severity of COVID 19 disease. The mean age of the patients was 52 ± 11.4 years. This was not surprising and goes along with the work of Basaran et al. [7] (57.55 ± 17.89 years), as older COVID-19 patients are more likely to need hospitalization.
We found no significant difference in vitamin D levels according to age or sex. This finding goes along with that of Yosef et al. [14] who also conducted their study on an Egyptian cohort. In contrast, many other studies showed lower levels of vitamin D in older patients than younger patients and in females than males [15, 16].
In the present study, a significant difference in serum vitamin D level was found in patients on different modes of oxygen therapy. Patients who were intubated had the lowest levels of serum vitamin D level (7.26 ng/ml ± 5.21), while patients who had no need for oxygen supply had the highest levels (20.00 ng/ml ± 9.23) (P = 0.025). This goes along with the analyzed data of 144 patients in USA that proved that sufficient vitamin D level was independently significantly associated with lower need for invasive mechanical ventilation (odds ratio 0.96; P = 0.01) [10], while another study conducted in UAE reported that vitamin D levels were not correlated to the need for mechanical ventilation [8].
In this study, a decrease in vitamin D levels was associated with more severe COVID-19 cases, as evidenced by significantly higher blood levels of inflammatory markers CRP and serum ferritin (P = 0.005 and 0.002 respectively), suggesting that vitamin D might have a beneficial role on the systemic inflammatory state of this viral disease. Consistent with our data, in a cohort of 235 COVID-19 patients, Maghbooli et al. [17] showed that CRP levels were lower in patients with vitamin D > 30 ng/ml. Similarly, Saporano et al. [9] found a significant inverse correlation between vitamin D levels and each of CRP, D-Dimer, and interleukin 6 (IL6). In another study by Daneshkhah et al. [18], high levels of CRP were associated with hypovitaminosis D. On the other hand, Hafez et al. [8] found a significant inverse correlation between vitamin D level and both lactate dehydrogenase (LDH) and fibrinogen, but not CRP or ferritin.
Few studies also evaluated the relationship between D-dimer levels and serum vitamin D level. In contrast to our data that did not show a significant relation between vitamin D levels and D-dimer, the retrospective study by Demir et al. [19] on 227 COVID-19 patients showed that D-dimer was higher in the presence of low vitamin D levels. Similar results were reported by Giannini et al. [20] in a cohort of 91 patients.
Regarding the parameters affecting mortality, age, sex, and presence of different comorbidities did not differ significantly between survivors (group 1) and deceased patients (group 2). Similarly, Alsafar et al. [11] showed that gender and comorbidities did not contribute to the mortality. However, in a retrospective two-center cohort study in UK including 433 COVID-19 patients, non-survivors were significantly older and more likely to have comorbidities [21]. This goes in line with a Brazilian study that had indicated a statistically significant correlation between mortality and both diabetes mellitus and hypertension [12]. The inconsistency between different studies suggests the presence of several confounding factors affecting the results, so further well-controlled clinical trials are required.
Considering serum vitamin D levels, they were significantly lower in COVID-19 deceased patients. This comes in harmony with many studies. One study in Turkey revealed that a significantly higher ratio of the deceased patients had vitamin D deficiency compared to surviving patients (92.8% vs. 48.8%, P < 0.001) and proved vitamin D deficiency to be an independent predictor of mortality [13]. Another retrospective study conducted upon 185 COVID-19 patients in Germany found that vitamin D deficiency at the time of admission was associated with higher risk of mortality (P = 0.001) [22]. In a recent meta-analysis including six studies and 376 COVID-19-positive patients, poor prognosis defined as severe symptoms, ICU admission, or death was present in 150 patients who also showed significantly lower levels of vitamin D, compared with patients with good prognosis [23]. Notably, Campi et al. [24] found that a 1-ng/ml increase in vitamin D levels was associated with a decrease of risk of death of 4%. However, Chen et al. [25] reported that neither vitamin D deficiency (< 20 ng/ml) nor insufficiency (< 30 ng/ml) was associated with increased risk of COVID-19 in-hospital death. Another study conducted in Iran with a cohort of 329 cases of COVID-19 showed no relationship between vitamin D status and death rate [26]. Additionally, a cohort study using UK Biobank showed no evidence that the hazard of COVID-19 mortality was higher among participants with vitamin D insufficiency or deficiency [27].
Additionally, deceased patients had significantly higher levels of WBCS, and BUN (P = 0.008 and 0.002 respectively). This is compatible with the results of a retrospective single center study in China, concluding that WBC count at admission is significantly correlated with death in COVID-19 patients [28].
Moreover, group 2 patients had significantly lower hemoglobin and potassium levels than group 1 patients (P = 0.023 and 0.013 respectively). This is in agreement with a prospective study in Iran reporting that anemic patients were significantly more likely to develop poor outcomes of COVID-19, including ICU admission and death [29]. Exacerbation of inflammation by the cytokine storm which occurs during the SARS-CoV-2 infection can explain the higher degrees of anemia found in the deceased patients.
Our study has some limitations. Our sample size was relatively small. In addition, no dietary assessment was carried out, and therefore, information on dietary habits is lacking.
Conclusion
In conclusion, serum vitamin D levels were significantly lower in patients needing mechanical ventilation and in deceased patients. Moreover, serum vitamin D levels were significantly inversely related to the inflammatory markers CRP and serum ferritin, advocating the favorable effect of vitamin D on morbidity and mortality. Our study has clinical implications, as it suggests that vitamin D may calm down the inflammatory cascades that lead to severe outcomes from COVID-19. Provided its low cost and availability; further investigation of vitamin D supplementation as a preventive and therapeutic strategy for COVID-19 with randomized trials is warranted.
Availability of data and materials
The datasets generated and analyzed during the current study are available from the corresponding author upon request.
Abbreviations
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase
- BUN:
-
Blood urea nitrogen
- CBC:
-
Complete blood count
- CO-RADS:
-
COVID-19 Reporting and Data System
- COVID-19:
-
Coronavirus disease
- CRP:
-
C-reactive protein
- CT:
-
Computed tomography
- ICU:
-
Intensive care unit
- LDH:
-
Lactate dehydrogenase
- RT-PCR:
-
Reverse transcriptase-polymerase-chain reaction
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus 2
- SPSS:
-
Statistical Package for Social Science
- WBC:
-
White blood cell count
- WHO:
-
World Health Organization
References
Cucinotta D, Vanelli M (2020) WHO declares COVID-19 a pandemic. Acta Biomed 91:157–160
Gao YD, Ding M, Dong X, Zhang JJ, Kursat Azkur A, Azkur D et al (2021) Risk factors for severe and critically ill COVID-19 patients: a review. Allergy 76(2):428–455
Darif D, Hammi I, Kihel A, El Idrissi SI, Guessous F, Akarid K (2021) The pro-inflammatory cytokines in COVID-19 pathogenesis: what goes wrong? Microb Pathog 153:104799
Bae JH, Choe HJ, Holick MF, Lim S (2022) Association of vitamin D status with COVID-19 and its severity: vitamin D and COVID-19: a narrative review. Rev Endocr Metab Disord 23(3):579–599
Chiodini I, Gatti D, Soranna D, Merlotti D, Mingiano C, Fassio A et al (2021) Vitamin D status and SARS-CoV-2 infection and COVID-19 clinical outcomes. Front Public Health 9:736665
Prokop M, Van Everdingen W, Van Rees VT (2020) CO-RADS: A categorical CT assessment scheme for patients suspected of having COVID-19 definition and evaluation. Radiology 296(2):E97–E104
Basaran N, Adas M, Gokden Y, Turgut N, Yildirmak T, Guntas G (2021) The relationship between vitamin D and the severity of COVID-19. Bratisl Lek Listy 122(3):200–205
Hafez W, Saleh H, Arya A, Alzouhbi M, Fdl Alla O, Lal K et al (2022) Vitamin D status in relation to the clinical outcome of hospitalized COVID-19 patients. Front Med (Lausanne) 9:843737
Saponaro F, Franzini M, Okoye C, Antognoli R, Campi B, Scalese M et al (2022) Is there a crucial link between vitamin D status and inflammatory response in patients with COVID-19? Front Immunol 12:745713
Angelidi AM, Belanger MJ, Lorinsky MK, Karamanis D, Chamorro-Pareja N, Ognibene J et al (2021) Vitamin D status is associated with in-hospital mortality and mechanical ventilation: a cohort of COVID-19 hospitalized patients. Mayo Clin Proc 96(4):875–886
AlSafar H, Grant WB, Hijazi R, Uddin M, Alkaabi N, Tay G et al (2021) COVID-19 disease severity and death in relation to vitamin D status among SARS-CoV-2-positive UAE residents. Nutrients 13(5):1714
de Almeida-Pititto B, Dualib PM, Zajdenverg L, Dantas JR, de Souza FD, Rodacki M et al (2020) Brazilian Diabetes Society Study Group (SBD). Severity and mortality of COVID 19 in patients with diabetes, hypertension and cardiovascular disease: a meta-analysis. Diabetol Metab Syndr 12:75
Karahan S, Katkat F (2021) Impact of Serum 25(OH) Vitamin D level on mortality in patients with COVID-19 in Turkey. J Nutr Health Aging 25(2):189–196
Yosef TM, Saleh SA, Ali SF, Ahmed AE (2022) Vitamin D assessment in patients with COVID-19 virus and correlation with severity. Egypt J Intern Med 34(1):52
Sanghera DK, Sapkota BR, Aston CE, Blackett PR (2017) Vitamin D status, gender differences, and cardiometabolic health disparities. Ann Nutr Metab 70(2):79–87
Pagano MT, Peruzzu D, Ruggieri A, Ortona E, Gagliardi MC (2020) Vitamin D and sex differences in COVID-19. Front Endocrinol (Lausanne) 11:567824
Maghbooli Z, Sahraian MA, Ebrahimi M, Pazoki M, Kafan S, Tabriz HM et al (2020) Vitamin D sufficiency, a serum 25-hydroxyvitamin D at least 30 ng/mL reduced risk for adverse clinical outcomes in patients with COVID-19 infection. PLoS One 15(9):e0239799
Daneshkhah A, Agrawal V, Eshein A, Subramanian H, Roy HK, Backman V (2020) Evidence for possible association of vitamin D status with cytokine storm and unregulated inflammation in COVID-19 patients. Aging Clin Exp Res 32(10):2141–2158
Demir M, Demir F, Aygun H (2021) Vitamin D deficiency is associated with COVID-19 positivity and severity of the disease. J Med Virol 93:2992–2999
Giannini S, Passeri G, Tripepi G, Sella S, Fusaro M, Arcidiacono G et al (2021) Effectiveness of in-hospital cholecalciferol use on clinical outcomes in comorbid COVID-19 patients: a hypothesis-generating study. Nutrients 13(1):219
Zafar M, Karkhanis M, Shahbaz M, Khanna A, Barry L, Alam S et al (2022) Vitamin D levels and mortality with SARS-COV-2 infection: a retrospective two-centre cohort study. Postgrad Med J 98(1161):523–528
Radujkovic A, Hippchen T, Tiwari-Heckler S, Dreher S, Boxberger M, Merle U (2020) Vitamin D deficiency and outcome of COVID-19 patients. Nutrients 12(9):2757
Munshi R, Hussein MH, Toraih EA, Elshazli RM, Jardak C, Sultana N et al (2021) Vitamin D insufficiency as a potential culprit in critical COVID-19 patients. J Med Virol 93(2):733–740
Campi I, Gennari L, Merlotti D, Mingiano C, Frosali A, Giovanelli L et al (2021) Vitamin D and COVID-19 severity and related mortality: a prospective study in Italy. BMC Infect Dis 21(1):566
Chen J, Mei K, Xie L, Yuan P, Ma J, Yu P et al (2021) Low vitamin D levels do not aggravate COVID-19 risk or death, and vitamin D supplementation does not improve outcomes in hospitalized patients with COVID-19: a meta-analysis and GRADE assessment of cohort studies and RCTs. Nutr J 20(1):89
Nasiri M, Khodadadi J, Molaei S (2021) Does vitamin D serum level affect prognosis of COVID-19 patients? Int J Infect Dis. 107:264–267
Lin LY, Mulick A, Mathur R, Smeeth L, Warren-Gash C, Langan SM (2022) The association between vitamin D status and COVID-19 in England: A cohort study using UK Biobank. PLoS One 17(6):e0269064. Published 2022 Jun 6. https://doi.org/10.1371/journal.pone.0269064
Zhu B, Feng X, Jiang C, Mi S, Yang L, Zhao Z et al (2021) Correlation between white blood cell count at admission and mortality in COVID-19 patients: a retrospective study. BMC Infect Dis. 21(1):574
Faghih Dinevari M, Somi MH, Sadeghi Majd E, Abbasalizad Farhangi M, Nikniaz Z (2021) Anemia predicts poor outcomes of COVID-19 in hospitalized patients: a prospective study in Iran. BMC Infect Dis. 21(1):170
Acknowledgements
Not applicable.
Funding
Nil.
Author information
Authors and Affiliations
Contributions
Study was designed by Dr. RAH. Data collected by Dr. ETY. Data interpreted by Dr. RAH, Dr. CSM, Dr. SAK, and Dr. ETY. Manuscript written and edited by Dr. CSM and Dr. SAK. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ain Shams University, Faculty of Medicine Research Ethics Committee (REC) FWA 000017585. An informed written consent was taken from patients enrolled in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Morad, C.S., Habeeb, R.A., Yassin, E.T. et al. Serum vitamin D level in COVID-19 patients and its correlation with disease severity. Egypt Rheumatol Rehabil 49, 55 (2022). https://doi.org/10.1186/s43166-022-00155-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43166-022-00155-9