Abstract
Background
One of the most important and dangerous complications of rheumatoid arthritis (RA) is bone loss, which manifested by erosions and juxta-articular or systemic bone loss. Anti-carbamylated protein (anti-CarP) antibodies which are also called anti-homocitrulline antibodies have recently been found in RA. Increase anti-CarP antibody titres may lead to severe disease and increase the progression of bone loss. Osteoprotegrin and receptor activator for nuclear factor kappa B and its ligand (RANKL) are the main players in the pathogenesis of osteoporosis. Thus, we aimed to investigate and detect the presence and prevalence of anti-CarP in rheumatoid arthritis and their association with disease severity and osteoporosis, as well as with OPG/RANKL in 80 Egyptian RA patients to highlight this relationship which could be useful in managing RA patients with osteoporosis.
Results
Serum anti-CarP levels were significantly increased in the RA group compared with the control group (P< 0.001). We found a negative association between anti-CarP and anti-CCP and disease activity (r=−0.878, −0.534, respectively, P<0.001). We also found a positive correlation between anti-CarP and the Larsen score, DEXA score, RF, HAQ, and RANKL (r=0.646, 0.287, 0.243, 0.892, 0.671, 0.869 [respectively], P<0.001) and there was negative correlation between anti-CarP and OPG (r=−0.553, P<0.001).
Conclusion
Anti-CarP antibodies are associated with disease severity and disability in RA patients. They could play an important and significant role in the pathogenesis of osteoporosis in these patients.
Similar content being viewed by others
Background
Rheumatoid arthritis is a chronic autoimmune inflammatory disease that is manifested by synovitis and joint destruction [1]. Erosion and bone loss (juxta-articular or systemic) are prevalent [2].
Erosion usually occurs at the bone surface beneath the inflamed tendon and synovium and it is defined as focal loss of bone (cortical and trabecular) [3]. RA patients have higher risk of osteoporosis than normal subjects. This mostly occurs in the lumbar spine (LS) and hip region [4, 5]; and there is a high risk of fractured hip and spine depending on duration of the disease and medications that are used [6,7,8,9].
The increased risk of osteoporosis in RA patients can be caused by many factors such as corticosteroid medications that are taken for the disease. Decreased activity due to pain may also increase the risk of osteoporosis; and this risk may also increase due to disease progression [10].
In the complex system of bone remodeling, RANKL/OPG pathway is the coupling factor between bone formation and bone resorption. RANKL acts through binding to its receptors on the surface of osteoclasts and activates differentiation of these cells. Also, the balance between OPG and RANKL determines osteoblast proliferation and activity, and OPG binding to RANKL lead to inhibition of osteoclastic bone resorption [11].
Anti-carbamylated protein (anti-CarP) antibodies are the most recent antibodies that have been detected in RA. Increase anti-CarP antibody titres may lead to severe disease and increase the progression of bone loss. Even within ACPA-negative patients, carbamylation is a process in which a cyanate group is added on self-proteins to determine the changes in the tertiary structure. This can lead to new epitope generation and production of autoantibodies. Additionally, anti-CarP antibodies seem to play an important pathogenic role in RA which is similar to ACPA. Anti-CarP antibodies may be found in the serum for a long time before disease manifestations appearance [12].
The aim of our study was to investigate the prevalence of anti-CarP in RA, its correlation and its association with the severity of the disease and osteoporosis as well as with OPG/RANKL. Thus, these antibodies could be very useful in managing of RA patients with osteoporosis.
Methods
This was a cross-sectional study in which 80 RA patients were selected randomly and forty healthy controls that were matched for age and sex were included for laboratory investigations.
The patients and control subjects were chosen from the inpatient unit and outpatient clinic in the Rheumatology and Rehabilitation Department at our University Hospital from October 2019 to February 2020.
Inclusion criteria
We included all patients with RA who were diagnosed according to the American College of Rheumatology (ACR)/European League against Rheumatism (EULAR) 2010 criteria for the diagnosis of RA [13].
Exclusion criteria
We excluded RA patients who were taking anti-resorptive drugs, patients with other inflammatory arthritic diseases, and those receiving corticosteroids or other medications that affect bone remodeling.
Written informed consent was obtained from the patients and controls at the beginning of the study, and our study was approved by the ethics committee at our university (approval code 34206-10-19) and it was conducted in accordance with the Declaration of Helsinki. All patients provided a detailed history and underwent full clinical examinations. We used a predesigned and validated questionnaire sheet that included the following: sociodemographic data such as sex, age, and disease duration, measures of disease activity using disease activity score 28 (DAS28) [14], Health Assessment Questionnaire (HAQ) [15], and plain X-ray of hands and feet for assessment of radiographic damage by a modified Larsen’s score [16].
Laboratory assessments
Blood sampling
After 12 h of overnight fasting, venous blood samples were obtained from our patients and controls. Some of the blood was collected in centrifuge tubes that were sterile and dry. After allowing the blood to clot, it was centrifuged for 10 min, and the serum was stored frozen at −80 °C after collection until analysis. Another sample was collected into heparinized tube and stored at −80 °C until peripheral blood mononuclear cells preparation.
Biochemical assay
1-Erythrocyte sedimentation rate (ESR in mm/h) was detected by using the Westergren method [17].
2-Serum C-reactive protein (CRP in mg/L) was quantified by using the latex slide semi-quantitative test [18].
3-Rheumatoid factor (RF) was measured by using the slide hemagglutination Rose Waaler test [19].
4-Anti-cyclic citrullinated peptide antibodies (anti-CCP) were measured using commercial ELISA plates coated with second-generation citrullinated peptides [20].
5-Serum osteoprotegerin (OPG) levels were detected using an enzyme linked immunosorbent assay technique (ELISA) [11].
6-Serum anti-CarP levels were detected using an ELISA kit (Cat # MBS7253927, MyBioSource, Inc., San Diego, CA, USA) [21].
7-Receptor activators of nuclear factor Kappa B ligand (RANKL) levels in the serum were determined using an ELISA kit (Cat # MBS2024017, MyBioSource, Inc.) [11].
Bone mineral density (BMD) measurements
The BMD was measured by using DEXA at the following locations: total hip (TH), lumber spine (LS), and the forearm. T-score of –2.5 or less is considered to be diagnostic for osteoporosis [22].
Statistical analysis
Statistical analyses were performed using the SPSS statistical software v21.0. For independent groups, we used the t test. Spearman’s test was used to determine the presence of correlation. Multiple logistic regression analyses were used to assess the prediction of osteoporosis by anti-CarP.
Results
Table 1 presents the demographic data from the patients and controls: The mean age of the RA patients was 46.76 ± 10.03 years (range, 30–65 years) and 71 were females (88.8%) and nine were males (11.3%). The control group comprise 40 participants who were matched for age (44.66 ± 7.22years) and gender34 female (85%) and 6 male (15%).
Table 2 presents the number and percentage of positive anti-CarP RA patients according to the DEXA score. The percentage of patients who had osteoporosis in the LS and TH was higher than that for the forearm. Table 3 presents the number and percentage of the patients according to positive laboratory test results.
Anti-CarP was positive in 37.5% of patients. Correlations of anti-CarP with laboratory findings in the patients were shown in Table 4. There was a positive correlation between RF and RANKL and a negative correlation between anti-CCP, ESR, and CRP and OPG.
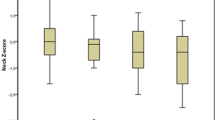
Correlations between anti-CarP and clinical parameters, DEXA and modified Larsen score in our patients were presented in Table 5, there was positive correlation between anti-CarP and VAS, HAQ, Larsen and DEXA score, and a negative correlation between anti-CarP and DAS score.
Discussion
Carbamylation is a process in which nonenzymatic posttranslational modification occurs in lysine residues. Serum anti-CarP antibody levels are increased in a high percentage of RA patients, and the presence of these autoantibodies leads to more severe disease and increased an incidence of bone erosions [23].
Patients with arthralgia who are positive for anti-CarP antibodies show higher prevalence of RA, and these antibodies can be found in patients’ serum before symptoms appear [24]. There was a significant increase in anti-CarP positivity in RA patients compared to the normal control group (Table 1). Anti-CarP positive results were also present in a large percentage of the patients (Table 3). This is in agreement with other study that showed anti-CarP antibodies were elevated in the serum of high percentage of RA patients [25].
We found double positivity in anti-CarP antibodies and anti-CCP in about 3.8% only of patients; there were anti-CarP and RF antibodies in 10% (Table 3). The percentage are slightly more than the results of other study which detect double positivity between anti carp and anti-CCP in 1.1% and between it, and RF is 2.2% only [26] but agree with findings of some studies which detect anti-CarP antibodies in seronegative patients [27]. Presence of many autoantibodies is giving a chance for early and accurate diagnosis of the disease [28].
There was a negative association between anti-CarP and disease activity parameters (ESR, CRP) and anti-CCP (Table 4). This result disagrees with other studies which found that increased disease activity was associated with increased level of anti-CarP in the serum of inflammatory polyarthritis patients [29, 30]. In a recent study, no association was observed between the presence of anti-CarP antibodies and disease activity in rheumatoid arthritis patient [26, 31]. More studies on large number of patients and long-term follow-up are needed to determine the utility of anti-CarP antibodies regarding correlation with disease activity.
There was a positive association between anti-CarP antibodies and RF and HAQ in agreement with Othman et al. who demonstrated that anti-CarP antibodies were linked to increased disease disability in inflammatory polyarthritis patients and increased disability to them [31].
There was a positive correlation between anti-CarP and Larsen score and DEXA score (Table 5) which suggests that anti-CarP may play a role in bone loss, joint erosion, and destruction in RA. This is in agreement with some studies which demonstrated that elevated serum level of anti-CarP antibodies is associated with increased rate of radiographic destruction [26, 31]. Our work also agrees with a study showing decreased bone mineral density in arthritis patients with increased level of anti-CarP antibodies [32], which may be because ACPA and anti-CarP influence osteoclasts activity.
Binding of ACPA to osteoclast cells and their precursors enhances its differentiation and activity and promotes proinflammatory and proosteoclastogenic cytokines release [12]. This is the same mechanism that occurs in positive anti-CarP patients with inflammatory disease.
BMD was decreased more in the LS and TH than in the forearm in patients who were positive for anti-CarP (Table 2), which suggests that the high anti-CarP antibodies titers may lead to systemic bone loss.
In our study, there was positive correlation between anti-CarP and RANKL. There was a negative correlation between anti-CarP and OPG. The OPG/RANKL system is an important regulator of osteoclasts activity [33]. RANKL is expressed by many cells and cytokines and mainly by osteoblasts and synovial cells which is similar to IL1, IL6, and IL17. RANKL is responsible for osteoclasts activation and it is an important factor for bone damage in inflammatory arthritis [34, 35].
Neutrophils, especially neutrophil extracellular tarps (NETs), can lead to the generation of modified autoantigens in RA synovium. Studies have shown that NETs containing carbamylated autoantigens can enhance pathogenic adaptive immunity which leads to production of anti-CarP. Anti-NET protein antibodies can stimulate macrophages to produce proinflammatory cytokines to release RANKL, which promote osteoclast formation and activation. Anti–CarP antibodies can also lead to immune complex formation which can increase osteoclast formation and bone resorption [36].
Previous studies have shown that radiographic progression can be predicted by presence of RANKL or the RANKL/OPG ratio [37, 38]. An increased Larsen score is associated with combined increased RANKL and anti-CarP concentrations [34]. These findings suggest that there is a novel correlation between anti-CarP antibodies and RANKL and radiographic changes in early RA.
Conclusion
In conclusion, anti-CarP antibodies may have an additive diagnostic value and may play a role in the pathogenesis of RA especially in osteoporosis related to RA as it shows positive correlation to RANKL and a negative correlation to OPG. Also, it may be a good predictor of the severity of the disease and play a role in the development of osteoporosis in the rheumatoid patients.
More extensive studies with long-term follow-up are required with more patients to detect its exact role in the disease progression and osteoporosis.
The limitations of our study are the relatively small number of patients; also, we did not perform ultrasonographic study for our patients which could detect the erosions earlier that X-ray. Future studies are recommended with long-term follow-up to highlight the relationship between the anti-CarP and osteoporosis.
Availability of data and materials
Not applicable
Abbreviations
- anti-CarP:
-
Anti-carbamylated protein
- RA:
-
Rheumatoid arthritis
- RF:
-
Rheumatoid factor
- Anti-CCP:
-
Anti-cyclic citrullinated peptide
- DAS28:
-
Disease activity for 28 joint indices score
- HAQ:
-
Health Assessment Questionnaire
- ESR:
-
Erythrocyte sedimentation rate
- CRP:
-
C-reactive protein
- OPG:
-
Osteoprotegerin
- RANKL:
-
Receptor activator of nuclear factor κB ligand
- BMD:
-
Bone mineral density
- LS:
-
Lumbar spine
- TH:
-
Total hip
References
Smolen JS, Aletaha D, McInnes IB (2016) Rheumatoid arthritis. Lancet 388:2023–2038
Kleyer A, Schett G (2014) Arthritis and bone loss: a hen and egg story. Curr Opin Rheumatol 26:80–84
Schett G, Gravallese E (2012) Bone erosion in rheumatoid arthritis: mechanisms, diagnosis and treatment. Nat Rev Rheumatol 8:656–664
Haugeberg G, Uhlig T, Falch JA, Halse JI, Kvien TK (2000) Bone mineral density and frequency of osteoporosis in female patients with rheumatoid arthritis: results from 394 patients in the Oslo County Rheumatoid Arthritis register. Arthritis Rheum. 43(3):522–530
Haugeberg G, Uhlig T, Falch JA, Halse JI, Kvien TK (2000) Reduced bone mineral density in male rheumatoid arthritis patients: frequencies and associations with demographic and disease variables in ninety-four patients in the Oslo County Rheumatoid Arthritis Register. Arthritis Rheum. 43(12):2776–2784
Van Staa TP, Geusens P, Bijlsma JW, Leufkens HG, Cooper C (2006) Clinical assessment of the long-term risk of fracture in patients with rheumatoid arthritis. Arthritis Rheum. 54(10):3104–3112
Orstavik RE, Haugeberg G, Mowinckel P, Hoiseth A, Uhlig T, Falch JA et al (2004) Vertebral deformities in rheumatoid arthritis: a comparison with population-based controls. Arch Intern Med. 164(4):420–425
Bultink IE, Lems WF (2014) Performance of vertebral fracture assessment in addition to dual energy X-ray absorptiometry in patients with rheumatoid arthritis. Rheumatology (Oxford). 53(5):775–776
Mohammad A, Lohan D, Bergin D, Mooney S, Newell J, O’Donnell M et al (2014) The prevalence of vertebral fracture on vertebral fracture assessment imaging in a large cohort of patients with rheumatoid arthritis. Rheumatology (Oxford). 53(5):821–827
Coulson KA, Reed G, Gilliam BE, Kremer JM, Pepmueller PH (2009) Factors influencing fracture risk, T score, and management of osteoporosis in patients with rheumatoid arthritis in the Consortium of Rheumatology Researchers of North America (CORRONA) registry. J Clin Rheumatol. 15:155–160
Kearns AE, Khosla S, Kostenuik PJ (2008) Receptor activator of nuclear factor kappaB ligand and osteoprotegerin regulation of bone remodeling in health and disease. Endocr Rev 29:155–192
Ajeganova S, van Steenbergen HW, Verheul MK, Forslind K, Hafstrom I, Toes RE et al (2017) The association between anti-carbamylated protein (anti-CarP) antibodies and radiographic progression in early rheumatoid arthritis: a study exploring replication and the added value to ACPA and rheumatoid factor. Ann Rheum Dis 76:112–118
Aletaha D, Neogi T, Silman AJ et al (2010) The 2010 rheumatoid arthritis classification criteria: an American College of Rheumatology/European League against rheumatism collaborative initiative. Ann Rheum Dis 62(9):2569–2581
Prevoo ML, van ’t Hof MA, Kuper HH, van Leeuwen MA, van de Putte LB, van Riel PL (1995) Modified disease activity scores that include twenty-eight–joint counts: development and validation in a prospective longitudinal study of patients with rheumatoid arthritis. Arthritis Rheum 38:44–48
Fries JF, Spitz P, Kraines RG, Holman HR (1980) Measurement of patient outcome in arthritis. Arthritis Rheum 23:137–145
Rau R, Herborn G (1995) A modified version of Larsen’s scoring method to assess radiologic changes in rheumatoid arthritis. J Rheumatol 22(10):1976–1982
Dac ie JV, Lewis SM (1991) The erythrocyte sedimentation rate, practical haematology, 7th edn. Churchill Livingstone, Edinburgh, pp 521–534
Ver ma S, Kuliszewski MA, Li SH, Szmitko PE, Zucco L, Wang CH et al (2004) C-reactive protein attenuates endothelial progenitor cell survival, differentiation, and function: further evidence of a mechanistic link between C-reactive protein and cardiovascular disease. Circulation 109:2058–2067
Roberts-Thomson PJ, McEvoy R, Langhans T, Bradley J (1985) Routine quantification of rheumatoid factor by rate nephelometry. Ann Rheum Dis 44:379–383
Swarta A, Burlingameb RW, Gürtlera I, Mahlerb M (2012) Third generation anti-citrullinated peptide antibody assay is a sensitive marker in rheumatoid factor negative rheumatoid arthritis. Clinica Chimica Acta 14:266–272
Montes A, Regueiro C, Perez-Pampin E, Boveda MD, Gomez-Reino JJ, Gonzalez A (2016) Anti-carbamylated protein antibodies as a reproducible independent type of rheumatoid arthritis autoantibodies. PLoS One. 11:e0161141
Sheu A, Diamond T (2016) Diamond Bone mineral density: testing for osteoporosis. Australian Prescriber. 39(2):35–39
Vidal-Bralo L, Perez-Pampin E, Regueiro C, Montes A, Varela Z, Boveda MD, Gomez-Reino JJ, Gonzalez A (2017) Anti-carbamylated protein autoantibodies associated with mortality in Spanish rheumatoid arthritis patients. PLOS ONE 12:e0180144
Fluckiger R, Harmon W, Meier W, Loo S, Gabbay KH (1981) Hemoglobin carbamylation in uremia. N Engl J Med 304:823–827
Shi J, van de Stadt LA, Levarht EW, Huizinga TW, Toes RE, Trouw LA et al (2013) Anticarbamylated protein antibodies are present in arthralgia patients and predict the development of rheumatoid arthritis. Arthritis Rheum 65:911–915
Mohamed SR, Neseem NO, Metwally SS, El-Kady BA (2020) Diagnostic value and clinical significance of anti-carbamylated protein (anti-CarP) antibodies in Egyptian patients with rheumatoid arthritis. The Egypt Rheumatol 42(1):1–4 ISSN 1110-1164
Pecani A, Alessandri C, Spinelli FR, Priori R, Riccieri V, Di Franco M et al (2016) Prevalence, sensitivity and specificity of antibodies against carbamylated proteins in a monocentric cohort of patients with rheumatoid arthritis and other autoimmune rheumatic diseases. Arthritis Res Ther 18:276
Trouw LA, Mahler M (2012) Closing the serological gap: promising novel biomarkers for the early diagnosis of rheumatoid arthritis. Autoimmun Rev 12:318–322
Humphreys JH, Verheul MK, Barton A, MacGregor AJ, Lunt M, Toes RE et al (2016) Anticarbamylated protein antibodies are associated with long-term disability and increased disease activity in patients with early inflammatory arthritis: results from the Norfolk Arthritis Register. Ann Rheum Dis 75:1139–1144
Shi J, van de Stadt LA, Levarht EW, Huizinga TW, Hamann D, van Schaardenburg D et al (2014) Anti-carbamylated protein (anti-CarP) antibodies precede the onset of rheumatoid arthritis. Ann Rheum Dis. 73:780–783
Othman MA, Ghazali WS, Yahya NK (2017) Anti-carbamylated protein antibodies in rheumatoid arthritis patients and their association with rheumatoid. Saudi Med J 38(9):934–941
Shi J, Knevel R, Suwannalai P, van der Linden MP, Janssen GM, van Veelen PA et al (2011) Autoantibodies recognizing carbamylated proteins are present in sera of patients with rheumatoid arthritis and predict joint damage. Proc Natl Acad Sci U S A 108:17372–17377
Linda J, Arlestig L, Kokkonen H, Brink M, Rantapaa-Dahlqvist S (2017) An increased concentration of receptor activator of nuclear factor kappa-B ligand pre-dates the onset of rheumatoid arthritis. Rheumatology 56:2190–2196
Page G, Miossec P (2005) RANK and RANKL expression as markers of dendritic cell_T cell interactions in paired samples of rheumatoid synovium and lymph nodes. Arthritis Rheum 52:2307–2312
Khosla S (2001) Minireview: the OPG/RANKL/RANK system. Endocrinology 142:5050–5055
Carmona-Rivera PMC, Lingampalli EN, Uchtenhagen H, James E, Liu Y, Bicker KL, Wahamaa H, Hoffmann V, Catrena AI, Thompson P, Buckner JH, Robinson WH, Fox DA, Kaplan MJ (2017) Synovial fibroblast neutrophil interaction promote pathogenic adaptive immunity in rheumatoid arthritis. Sci.immunol. 2:3358
Hensvold AH, Joshua V, Li W et al (2015) Serum RANKL levels associate with anti-citrullinated protein antibodies in early untreated rheumatoid arthritis and are modulated following methotrexate. Arthritis Res Ther 17:239
HD VTL, Voskuyl AE, Boers M et al (2010) Baseline RANKL:OPG ratio and markers of bone and cartilage degradation predict annual radiological progression over 11 years in rheumatoid arthritis. Ann Rheum Dis 69:1623_8
Acknowledgements
Not applicable.
Funding
The study has no funding from any source.
Author information
Authors and Affiliations
Contributions
MH and ER authors had contributed to the conception, design of the work, the acquisition, analysis, interpretation of data, had drafted the work and substantively revised it, and finally, had agreed both to be personally accountable for their own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which they were not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature. HE contributed to collecting the patient’s data (history, clinical and investigation data), processed it in the patient excel sheet, and also contributed in statistical analysis and writing the manuscript. RG is a major contributor in methodology, analyzed and interpreted the patient’s data regarding the objectives and methods of research supervision of the steps of writing and results reviewing together with the final manuscript. All authors had read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Written informed consents were obtained from all the participants before entering the study.
The study was approved by the research ethics committee of the Tanta University, Faculty of Medicine (approval code (34206-10-19)).
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hussein, M.S., Gaber, R.A., Elsabagh, H.M. et al. Do anti-carbamylated protein antibodies in rheumatoid arthritis reflect local and systemic osteoporosis? A study of osteoprotegrin and receptor activator for nuclear factor kappa B ligand and radiological assessment. Egypt Rheumatol Rehabil 48, 18 (2021). https://doi.org/10.1186/s43166-021-00067-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43166-021-00067-0