Abstract
Background
Epidermal growth factor receptor (EGFR) tyrosine kinase inhibitors (TKIs) have significantly improved survival outcomes of advanced non-small cell lung cancer (NSCLC). Nonetheless, usage of TKIs is not without adverse effects, as it has been reported to cause irreversible sensorineural hearing loss (SNHL).
Case presentation
We describe a 72-year-old man who experienced hearing loss after taking osimertinib for 6 months. Later, his hearing further declined over a period of 1 year. Hearing rehabilitation with high-powered behind-the-ear (BTE) hearing aid has helped to improve his quality of life to some degree. There were no other known causative factors leading to the hearing deterioration. To date, there is no case report on osimertinib-induced SNHL.
Conclusion
Physicians ought to counsel patients on osimertinib of this rare side effect and monitor for early signs of hearing loss. Treatment protocol should be in place taking into account that they have either failed or likely to fail the first- or second-line treatments and have advanced stage disease.
Similar content being viewed by others
Background
Lung cancer is the second most common cancer with non-small cell lung cancer (NSCLC) constituting about 85% of cases. Epidermal growth factor receptor (EGFR) mutations are the main oncogenic drivers in up to 50% of NSCLC among the Asian populations and approximately 15% of Caucasians [1]. This discovery has shifted the treatment paradigm into utilizing EGFR tyrosine kinase inhibitors (TKI) as the standard first-line therapy. Osimertinib is a third-generation EGFR-TKI used in the treatment of central nervous system (CNS) metastases and in patients with acquired resistance to previous EGFR-TKI with superior safety profile and tolerability. We report a patient with NSCLC and brain metastasis who showed good response to osimertinib but developed possibly the antecedent case of drug induced sensorineural hearing loss.
Case presentation
A 72-year-old man with no known medical illness presented with a 6-month history of chronic cough, hoarseness, and headache. Computed tomography (CT) and positron emission tomography (PET) imaging showed lesions over the middle lobe of right lung and perihilar region measuring 1.5×1.5×1.5cm with a standardized uptake value (SUV) of 5.6. There were also four enhancing nodules in the midbrain, right superior cerebellum, left lateral wall of the fourth ventricle, and anterior interhemispheric cistern measuring 1.0×1.3cm, 0.7×0.6cm, 0.7×0.7cm, and 0.8×0.6cm, respectively. CT guided lung biopsy was performed and he was diagnosed with stage IV lung adenocarcinoma bearing the EGFR Exon 19 deletion. Treatment with oral osimertinib (Tagrisso) 80mg once a day was commenced. CT thorax performed at 1 month and 4 months post-therapy showed reducing perihilar mass and stable subcentimeter lung nodules. Magnetic resonance imaging (MRI) brain 4 months after commencement of osimertinib showed resolved intracranial lesions.
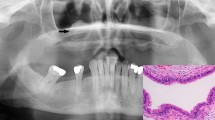
At 6 months following osimertinib treatment, he was referred to the otolaryngologist for worsening hearing and tinnitus in both ears. Otoscopy was unremarkable. Pure tone audiometry (PTA) revealed moderate to severe bilateral sensorineural hearing loss (SNHL) (Fig. 1). A repeat MRI brain ruled out any recurrent metastatic lesion. He decided to continue his usual drug regime despite being advised the possible risk of hearing deterioration, fearing the risk of tumour recurrence. Unfortunately, his hearing declined further over 1 year showing a severe to profound bilateral SNHL (Fig. 2). The relevant blood investigations including lipid and coagulation profiles were normal. Hearing rehabilitation with high-powered behind-the ear (BTE) hearing aid has helped to improve his quality of life to some degree.
Audiogram 1 year after the audiogram in Fig. 1, hearing loss progressed into bilateral severe to profound sensorineural hearing loss
Discussion
Osimertinib was first approved by the U.S. Food and Drug Administration in 2017 for the treatment of NSCLC after progression on older generation TKIs. Its usage has since then expanded to become the first-line treatment for NSCLC with EGFR T790M deletion or exon 21 L858R mutation and in patients with CNS metastases. Majority of patients who at first responded to first and second generation TKIs eventually develop disease progression. A secondary mutation in the EGFR T790M in the exon 20 is known to confer resistance in up to 50% of cases [2]. As for brain metastases, osimertinib demonstrated superior progression-free survival, duration of response, and lower toxicity in comparison to first generation TKIs. It also confers greater intracranial concentration versus the first and second generation TKIs and is more effective against leptomeningeal carcinomatosis [3]. Moreover, the use of osimertinib obviates the neurocognitive deficits and complications associated with surgery or brain irradiation in patients with CNS metastases without impending herniation.
Common side effects of TKIs are skin rashes, pruritus, fatigue, nausea, anemia, fever, diarrhea, and gastrointestinal intolerance. Ototoxicity is an uncommon adverse event attributed to TKIs. A few TKIs namely imatinib, nilotinib, regorafenib, sunitinib, and canertinib have reported cases of drug-induced SNHL. Imatinib and nilotinib (Bcr-Abl TKIs) can cause SNHL due to inhibition of c-kit resulting in possible neurotoxic effect on the auditory nerve [4]. On the other hand, regorafenib and sunitinib are vascular endothelial growth factor (VEGF) inhibitors which may induce SNHL by causing thrombotic microangiopathies and reduction of labyrinthine blood flow [5].
In relation to our case, erlotinib (1st generation EGFR-TKI) has been described to cause irreversible SNHL. The authors suggested that human epidermal growth factor receptor (HER) signaling in the inner ear was accountable. HER 2, 3, 4, and EGFR receptors are expressed in supporting cells, non-sensory cells, and hair cells involved in cochlear homeostasis, proliferation, and synaptic maintenance within the inner ear [6]. EGFR and transforming growth factor-alpha (TGF-a) were also shown to implicate auditory hair cell replacement and differentiation in the organ of Corti in response to ototoxic damage [7]. Osimertinib induced ototoxicity has not been documented in the literature. Its mechanism could be related to the role of EGFR and TGF ligands signaling in the inner ear.
Conclusion
Patients treated with EGFR TKIs should be monitored for early symptoms and signs of hearing loss. They should be promptly referred to an otolaryngologist to confirm the diagnosis of sensorineural hearing loss and the incidence appropriately reported to the relevant authority. With the increased usage of osimertinib, more adverse events related to the drug may be uncovered. The aim here is to offer the right treatment protocol taking into account that our patients have either failed or likely to fail first- or second-line treatments and have advanced stage disease.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- EGFR:
-
Epidermal growth factor receptor
- TKI:
-
Tyrosine kinase inhibitor
- NSCLC:
-
Non-small cell lung cancer
- SNHL:
-
Sensorineural hearing loss
- BTE:
-
Behind-the ear
- CT:
-
Computed tomography
- PET:
-
Positron emission tomography
- SUV:
-
Standardized uptake value
- MRI:
-
Magnetic resonance imaging
- PTA:
-
Pure tone audiometry
- CNS:
-
Central nervous system
- VEGF:
-
Vascular endothelial growth factor
- HER:
-
Human epidermal growth factor receptor
- TGF-a :
-
Transforming growth factor-alpha
References
LiLi C, Fang R, Sun Y et al (2011) Spectrum of oncogenic driver mutations in lung adenocarcinomas from East Asian never smokers. PLoS One. 6(11):e28204. https://doi.org/10.1371/journal.pone.0028204
Camidge DR, Pao W, Sequist LV (2014) Acquired resistance to TKIs in solid tumours: learning from lung cancer. Nat Rev Clin Oncol 11:473–481
Nanjo S, Hata A, Okuda C, Kaji R, Okada H, Tamura D et al (2018) Standard-dose osimertinib for refractory leptomeningeal metastases in T790M-positive EGFR-mutant non-small cell lung cancer. Br J Cancer 118:32–37
Petit C (1996) Genes responsible for human hereditary deafness: symphony of a thousand. Nat Genet. 14(4):385–391. https://doi.org/10.1038/ng1296-385
Dekeister K, Graillot E, Durbec M, Scoazec JY, Walter T (2016) Sunitinib-induced sudden hearing loss. Invest New Drugs. 34(6):792–793. https://doi.org/10.1007/s10637-016-0378-z
Koutras AK, Mastronikolis NS, Evans TR, Papadeas ES, Makatsoris T, Kalofonos HP (2008) Irreversible ototoxicity associated with the use of erlotinib in a patient with pancreatic cancer. Acta Oncol. 47(6):1171–1173. https://doi.org/10.1080/02841860802213328
Zine A, Nyffeler M, de Ribaupierre F (2000) Spatial expression patterns of epidermal growth factor receptor gene transcripts in the postnatal mammalian cochlea. Hear Res. 141(1-2):19–27. https://doi.org/10.1016/s0378-5955(99)00203-8
Acknowledgements
Not applicable.
Funding
No financial support was provided to this work.
Author information
Authors and Affiliations
Contributions
CCL did the conception, design, and writing of the manuscript. JLL performed the literature review and revision of the manuscript. JK followed up and collected the patient data, and edited the final edition of the manuscript. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lim, C.C., Lu, J.L. & Kulasegarah, J. Osimertinib-induced hearing loss: an uncommon aftereffect of a novel drug—a case report. Egypt J Otolaryngol 38, 64 (2022). https://doi.org/10.1186/s43163-022-00250-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43163-022-00250-w