Abstract
Background
Implantable vascular access devices (IVADs) provide durable routes for administering long-term treatments in patients. However, their associated complications pose a problem. One technique variation that can influence complication rates is the method of securing the IVADs, which is either by ligation or a purse-string suture.
Objective
To compare the two port-a-cath securing techniques, ligation and purse string, in terms of complication rates and types.
Study design
We prospectively included 67 paediatric patients who had port-a-cath insertions secured either by ligation or a purse-string suture at Salmaniya Medical Complex in Bahrain from January 2018 to June 2021. We recorded demographics, diagnoses, port-a-cath site of insertion and securing technique, operative time, follow-up duration, and complications. Patients who had previous port-a-cath insertions or other chemotherapy lines were excluded.
Results
Port-a-caths were secured by ligation in 35 cases and by a purse-string suture in 32 cases. There were 58.9% males and 41.8% females; sex was not correlated with complications (P = 0.11). Patients’ ages ranged from 2 months to 13 years. The overall complication rate of port-a-cath insertions was 16.42%. Complications occurred in 25.7% of ligation-secured port-a-caths and 6.3% of purse-string-secured port-a-caths. In the ligation-secured IVADs, complications included malfunction, infections, removal difficulty and blockage, malposition, and haematoma. Meanwhile, only leakage occurred in the purse-string-secured IVADs.
Conclusion
The port-a-cath securing technique was significantly correlated with complication rates. The complication types and rates in purse-string-secured catheters were lower than those reported in the literature. Leakage was the only complication that occurred in purse-string-secured port-a-caths.
Similar content being viewed by others
Background
Implantable vascular access devices (IVADs) are a durable type of central venous access. In paediatric patients, port-a-caths are particularly useful in managing oncology patients who require prolonged intravenous treatment [1]. This eliminates the discomfort patients experience from frequent venepunctures [2]. The established port-a-cath may then serve as a route of administering chemotherapeutic agents, fluids, and parenteral nutrition as well as a route to sample blood for investigations [1]. In children, the internal jugular vein has been reported to be a more favourable site of cannulation due to fewer anatomical variations of the vein between individuals along with higher chances of it having a larger size [3, 4].
The introduction of IVADs has significantly reduced complication rates in comparison with using tunnelled central catheters [5,6,7]. However, complications still pose a problem even with the use of IVADs [8]. Intraoperative complications include risks of pneumothorax, haemorrhage, and mispositioning. Meanwhile, potential postoperative complications include infections, dislodgement, venous thrombosis, and stenosis.
The occurrence and rates of complications may be associated with disease-related factors, insertion technique, or the procedure [9, 10]. Hence, technique variations can influence complication rates. One factor related to technique variations is the IVAD anchoring strategy used to seal the port. IVADs may be secured using upper ligation of the venotomy or a purse string. The main advantage of using the purse-string technique is that it is vessel sparing, which allows the restoration of the patency of the neck vessels after removing the catheter [11, 12]. However, to our knowledge, there have been no studies comparing complication rates of the two sealing techniques: ligation and purse string.
Objective of the study
In this study, port-a-caths were surgically inserted using either the right internal or external jugular veins, and the two anchoring techniques, ligation and purse string, were compared in terms of complication rates and types.
Materials and methods
We prospectively included a total of 67 paediatric oncology patients who had a port-a-cath insertion at the Paediatric Surgery Unit at Salmaniya Medical Complex in Bahrain between January 2018 and June 2021. We included all paediatric oncology patients at or less than 14 years of age who underwent open port-a-cath insertion by paediatric surgeons except those with a history of previous port-a-cath insertion or those who had other types of chemotherapy lines. Port-a-caths were inserted by paediatric surgeons using the open technique, as per the hospital protocol, which had more experience using open insertions.
Choice of port-a-cath insertion site
Most patients had their port-a-caths inserted in the right internal jugular vein (IJV), while only older children underwent port-a-cath insertion through the right external jugular vein (EJV) due to the larger vein calibre in older children, which permits use of the EJV.
Technique selection method
Port-a-caths were secured using either the ligation or purse-string technique to compare and contrast rates and types of complications using each of the techniques. The technique used for patients was determined solely by the operating surgeon’s preference.
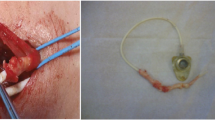
Operative technique
Open surgical insertion of the port-a-cath was conducted under general anaesthesia. A 2-cm-long horizontal incision was made 3.5 cm above the clavicle. Then, the subcutaneous tissue and the platysma were split, and the medial and lateral bodies of the sternocleidomastoid muscle were divided at the fossa supraclavicularis minor, where the internal jugular vein was exposed and two sutures for ligation were applied around the vein distal and proximal to the site of venotomy. These sutures were kept in place on standby (without performing the actual ligation) until the catheter was inserted at a later stage. Next, a small incision was made according to the size of the port chamber followed by blunt dissection to create a pouch for the port chamber 3.5 cm below the clavicle. The chamber was fixed at the pectoral fascia using absorbable sutures. Then, the catheter was tunnelled subcutaneously until it reached the cervical wound, the length of the catheter was measured, and the catheter was cut to a suitable length if needed. Then, the catheter was inserted through a venotomy and secured by ligation or purse string in cases where the port-a-cath was inserted in the internal jugular vein and ligation in cases where it was inserted in the external jugular vein. The position of the catheter was confirmed by X-ray. In cases where the external jugular vein was used, there was no need to expose the sternocleidomastoid muscle, as the vein is located in the subcutaneous layer just below the skin. Then, the catheter was tested by aspirating blood and flushing with 3–8 ml of heparinized saline solution (100 IU/ml). Finally, the wound was closed using an absorbable suture.
The data collection included patient age and sex, diagnosis, site of insertion of the port-a-cath (right internal jugular vein or right external jugular vein), technique used to seal the port-a-cath (ligation or purse string), operative time, follow-up duration, and complications. Complications were defined as early if they occurred before 30 days following port-a-cath insertion and late if they occurred at or 30 days after the insertion. The data were collected initially on an Excel spreadsheet.
Statistical analysis was conducted using SPSS statistics software, version 27 (IBM Corp., Chicago, IL, USA). With regard to descriptive analyses of categorical and continuous variables, frequency tables, means, and ranges were used. Correlations between variables were assessed using chi-square tests, and significance was deduced if p-values were 0.05 or less.
This study was granted ethical clearance by the responsible ethical committee: Ministry of Health’s Research Committee.
Results
Of the 67 patients, 35 underwent ligation distal and proximal to the venotomy site to secure the catheter, while 32 had the port-a-cath secured using a purse string. The sample consisted of 39 males (58.9%) and 28 females (41.8%). Children’s ages were a mean of 4.4 years, ranging from 2 months to 13 years of age (Table 1). No significant correlation was found between the occurrence of complications and age (P = 0.056) or sex (P = 0.11).
Patients’ diagnoses were either oncological or nononcological (indicated by pre-existing medical conditions) (Table 2). Diagnoses that indicated port-a-cath insertions were not associated with complication rates or types in paediatric patients (P = 0.76).
A total of 11 complications out of 67 port-a-cath insertion cases (16.42%) occurred following port-a-cath insertion using both securing techniques. Of these, 9 complications occurred at an early stage (less than 30 days following insertion), and only 2 complications (18.18%) occurred at a later stage (at or 30 days after the insertion). The late complications consisted of removal difficulty and blockage, which only presented during the removal of the port-a-caths. Reinsertion of the port-a-cath was performed for 7 of the complications, while conservative management was used in the case of 1 haematoma and 1 infection, and in the 2 cases with removal difficulty complications, port-a-caths were no longer needed. Of the 11 complications, 9 (25.7%) occurred using the ligation method of securing, while 2 (6.3%) occurred using the purse-string method of securing (Table 3). The technique of securing used (ligation or purse string) was significantly correlated with the occurrence of complications (P = 0.032). However, there was no correlation between the port-a-cath securing technique and the type of complication (P = 0.38).
Discussion
Vascular access is more challenging to achieve in paediatric patients because their vessels are smaller, more mobile, and have more anatomical variations [3, 4, 13]. In this study, the internal jugular vein was chosen because it has less anatomical variation and is larger in size [3, 4].
Numerous modifications over the years have been made to central line placement procedures. Tunnelled catheters with external exits were initially introduced by Broviac et al. [14] and revised by Hickman et al. [15]. The main revision consisted of increasing the diameter of the lumen from the 1-mm Broviac catheter to the 1.6-mm Hickman catheter. Moreover, implantable vascular access devices (IVADs) have been more recently introduced, characterized by being completely implantable with no exit sites [1]. The modifications made to the procedure have rendered improved outcomes and resulted in significant reductions in complications in addition to a reduced need for maintenance and increased freedom with activities [5,6,7]. However, although IVADs have been associated with lower complication rates than tunnelled catheters, they have given rise to new complications, such as reservoir damage and extravasation [5, 8, 16]. One dimension that has not been explored by the literature is whether there are implications of the different techniques of securing IVAD (ligation and purse string) on complication rates and types and the need for reinsertion of IVADs; this study compares ligation and purse-string-anchoring methods in terms of these outcomes.
Guidelines by the International Society of Paediatric Surgical Oncology (IPSO) present both ligation and the purse-string method as possible techniques of anchoring central venous catheters without recommending a single specific method [17]. Previously, one of the concerns associated with ligation was the potential cerebrovascular sequelae associated with internal jugular vein ligation. One randomized controlled trial on swine models demonstrated that there were no increases in jugular venous or intracranial pressure following ligation, despite increases in cerebral blood flow and oxygen consumption. The explanation proposed was the alternate decompression of the veinous system through outflow through the vertebral veins and left jugular veins [18]. Currently, the purse-string securing technique is preferred by some surgeons because it is vessel sparing, hence allowing for vein restoration once the catheter is removed [11, 12].
Complications were encountered in 16.42% of our study’s IVAD placements overall, which is within the range reported by the literature (15–48%) [7, 19, 20]. Meanwhile, looking at the port-a-cath securing techniques individually, 25.7% of IVADs secured by ligation had complications, while only 6.3% of those secured by a purse string had complications, which is below the rate reported by the literature. In our series, no association was found between the diagnoses and complications (P = 0.76).
Infections
Central venous line-related infection rates in studies range from 15 to 48% [7, 19, 20]. In our series, the infection rate in the group secured by ligation was only 5.7%, which is lower than the range in the literature; meanwhile, none of the cases secured by purse strings was complicated by infections.
Malfunction
Our series reports an 8.6% malfunction rate in the IVADs secured by ligation. Meanwhile, no cases of malfunction occurred in purse-string-anchored IVADs. The results in the ligation-secured port-a-caths are similar to rates reported by Bawazir et al. and Jawad et al., which were 7% and 5%, respectively [7, 16]. Meanwhile, the absence of malfunction complications in purse-string-secured port-a-caths in our series is lower than the other studies’ rates.
Dislodgement
Dislodgement occurs when the port and catheter become disconnected. Other series report dislodgement rates of port-a-caths ranging from 1.4 to 3.6% [8, 21]. This is similar to the dislodgement rate of 2.9% in ligation-secured port-a-caths in our study. However, no cases of dislodgement occurred in the purse-string-secured port-a-caths.
Removal difficulty and blockage
Prolonged use of central venous catheters makes catheters more difficult to remove due to higher risks of associated adhesions [22]. Moreover, catheters are at risk of being blocked. Our study reports difficult removal or blockage in 5.7% of ligation-secured port-a-caths. While the incidence of stuck catheters remains unknown, Jawad et al. and Babu et al. reported blockage rates of 4% and 7%, respectively [7, 8].
Haematoma
In our study, haematomas were considered a complication if following port-a-cath insertion; a swelling below the neck incision that was consistent with a haematoma was confirmed by ultrasound. We found a 2.9% occurrence of haematomas in ligation-anchored IVADs.
Leakage
Leakage occurs when the connecting apparatus loosens or the port dislodges [8, 19]. This can also result from inappropriate handling with inappropriate needle sizes or excessive force. In our series, no cases of leakage occurred in the ligation-secured port-a-caths. Meanwhile, this is the only complication that occurred using the purse-string-anchoring technique, whereby it occurred in 6.3% of port-a-caths secured by a purse string. This can be explained by the stronger seal formed using ligation.
The main limitations of this study are the single-centred setting and the small sample size. Moreover, the use of two different securing sites (internal jugular vein and external jugular vein) may have impacted the results. An additional influencing factor is the impact of the pre-existing condition and its severity on the results.
Conclusion
Complication rates were significantly lower in port-a-caths secured by purse string than in those secured by ligation. IVADs secured by ligation were complicated by infections, malfunction, dislodgement, removal difficulty and blockage; complication rates were similar to those reported in the literature. Meanwhile, leakage was the only complication that occurred in the purse-string-secured port-a-caths. The overall occurrence of complications in the purse-string group was lower than that reported in other series. Furthermore, there was no significant association between sex or the patients’ diagnoses and complication rates.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request
Abbreviations
- IVADs:
-
Implantable vascular access devices
- IJV:
-
Internal jugular vein
- EJV:
-
External jugular vein
- IPSO:
-
International Society of Paediatric Surgical Oncology (IPSO)
References
Scott-Warren VL, Morley RB. Paediatric vascular access. BJA Educ. 2015;15(4):199–206.
Rosovsky RP, Kuter DJ. Catheter-related thrombosis in cancer patients: pathophysiology, diagnosis, and management. Hematol Oncol Clin North Am. 2005;19(1):183–202.
Neto EPS, Grousson S, Duflo F, Tahon F, Mottolese C, Dailler F. Ultrasonographic anatomic variations of the major veins in paediatric patients. Br J Anaesth. 2014;112(5):879–84.
Breschan C, Platzer M, Jost R, Stettner H, Likar R. Size of internal jugular vs subclavian vein in small infants: an observational, anatomical evaluation with ultrasound. Br J Anaesth. 2010;105(2):179–84.
Ball AB, Duncan FR, Foster FJ, Davidson TI, Watkins RM, Hodson ME. Long term venous access using a totally implantable drug delivery system in patients with cystic fibrosis and bronchiectasis. Respir Med. 1989;83(5):429–31.
Harvey WH, Pick TE, Reed K, Solenberger RI. A prospective evaluation of the port-a-cath implantable venous access system in chronically ill adults and children. Surg Gynecol Obstet. 1989;169(6):495–500.
Jawad A, Alalayet Y, Alkasim F, Alhamidi S, Shoura M, Ghareeb E, et al. Totally implanted vascular access devices: a retrospective study of indications and complications in a single pediatric institute. J Appl Hematol. 2014;5:15.
Babu R, Spicer RD. Implanted vascular access devices (ports) in children: complications and their prevention. Pediatr Surg Int. 2002;18(1):50–3.
Machat S, Eisenhuber E, Pfarl G, Stübler J, Koelblinger C, Zacherl J, et al. Complications of central venous port systems: a pictorial review. Insights Into Imaging. 2019;10(1):86.
Whitman ED. Complications associated with the use of central venous access devices. Curr Probl Surg. 1996;33(4):309–78.
Ritz LA, Ley-Zaporozhan J, von Schweinitz D, Hubertus J. Long-term follow-up examination of the internal jugular vein after vessel-sparing implantation of a Hickman catheter or port catheter. Front Pediatr. 2019;7:58.
Kurkluoglu M, Badia S, Peer SM, Jonas R, Shankar V, Sinha P. Patency of common carotid artery and internal jugular vein after a simple vessel sparing cannulation for extracorporeal membrane oxygenation support. J Pediatr Surg. 2017;52(11):1806–9.
Janik JE, Conlon SJ, Janik JS. Percutaneous central access in patients younger than 5 years: size does matter. J Pediatr Surg. 2004;39(8):1252–6.
Broviac JW, Cole JJ, Scribner BH. A silicone rubber atrial catheter for prolonged parenteral alimentation. Surg Gynecol Obstet. 1973;136(4):602–6.
Hickman RO, Buckner CD, Clift RA, Sanders JE, Stewart P, Thomas ED. A modified right atrial catheter for access to the venous system in marrow transplant recipients. Surg Gynecol Obstet. 1979;148(6):871–5.
Bawazir O, Banoon E. Efficacy and clinical outcome of the port-a-cath in children: a tertiary care-center experience. World J Surg Oncol. 2020;18(1):134.
de Campos VAS, Chui CH, Cox S, Abdelhafeez AH, Fernandez-Pineda I, Elgendy A, Karpelowsky J, Lobos P, Wijnen M, Fuchs J, Hayes A, Gerstle JT. International Society of Paediatric Surgical Oncology (IPSO) Surgical Practice Guidelines ecancer. 2022;16:1356.
Chai PJ, Skaryak LA, Ungerleider RM, Greeley WJ, Kern FH, Schulman SR, et al. Jugular ligation does not increase intracranial pressure but does increase bihemispheric cerebral blood flow and metabolism. Crit Care Med. 1995;23(11):1864–71.
Bollard CM, Teague LR, Berry EW, Ockelford PA. The use of central venous catheters (portacaths) in children with haemophilia. Haemophilia. 2000;6(2):66–70.
Panthangkool W, Singhapakdi S, Teeraratkul S, Molagool S, Pakakasama S, Hathirat P, et al. Subcutaneous portacath utilization in pediatric oncology patients: Ramathibodi hospital experience. J Med Assoc Thailand=Chotmaihet Thangphaet. 1999;82:S77–81.
Dillon PA, Foglia RP. Complications associated with an implantable vascular access device. J Pediatr Surg. 2006;41(9):1582–7.
Chan BKY, Rupasinghe SN, Hennessey I, Peart I, Baillie CT. Retained central venous lines (CVLs) after attempted removal: an 11-year series and literature review. J Pediatr Surg. 2013;48(9):1887–91.
Acknowledgements
The authors have no further acknowledgements.
Funding
No funding was received for the conduct of this study.
Author information
Authors and Affiliations
Contributions
All authors have contributed to the conceptualization of the research, data collection or analysis, drafting, and approving the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was granted ethical approval by the responsible ethical committee.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Al Hindi, S., Khalaf, Z., Tan, A.K.L. et al. Complications of surgical port-a-cath implantation in paediatric patients: a single institution experience. Ann Pediatr Surg 18, 37 (2022). https://doi.org/10.1186/s43159-022-00179-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43159-022-00179-y