Abstract
Background
Children with medical complexity and associated neurologic impairment frequently face difficulties with venous access. Intermittently they require urgent intravenous administration of fluids and medication.
Objective
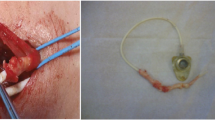
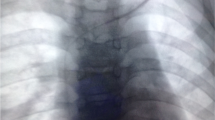
To analyze the use of implanted port-a-caths in children with medical complexity who have neurologic impairment and difficult venous access.
Materials and methods
We performed a single-center observational study of port-a-caths placed by interventional radiologists in children with medical complexity with neurologic impairment. We analyzed peripheral intravenous access attempts, peripheral intravenous starts, peripheral intravenous complications, alternative temporary central venous access devices, port-a-cath insertions, catheter days, access days, port-a-cath-related complications, hospital admissions and emergency department visits. We compared the year pre port-a-cath to the year post port-a-cath.
Results
Twenty-one children with medical complexity with neurologic impairment (10 boys, 11 girls; median age 4.1 years; median weight 13.7 kg) underwent 26 port-a-cath insertions (median catheter days 787). In the year post port-a-cath compared to pre port-a-cath there was a highly significant reduction (P<0.001) in numbers of peripheral intravenous attempts, peripheral intravenous starts and skin punctures; and a significant reduction (P<0.05) in need for other devices, number of emergency department visits, emergency department visits resulting in hospital admissions, and total admissions. Adverse events were graded as mild (n=18), moderate (n=6) and severe (n=0).
Conclusion
Port-a-cath placement in children with medical complexity with neurologic impairment significantly reduced all peripheral intravenous attempts, peripheral intravenous starts, skin punctures, total number of emergency department visits, visits culminating in admission, and total number of inpatient admissions. Advantages must be considered against potential port-a-cath-related adverse events.
Similar content being viewed by others
References
U.S. Congress Office of Technology Assessment (1987) Technology-dependent children: hospital v. home care — a technical memorandum. U.S. Government Printing Office, Washington, DC
McPherson M, Arango P, Fox H et al (1998) A new definition of children with special health care needs. Pediatrics 102:137–140
Cohen E, Kuo DZ, Agrawal R et al (2011) Children with medical complexity: an emerging population for clinical and research initiatives. Pediatrics 127:529–538
Cuper NJ, de Graaff JC, van Dijk AT et al (2012) Predictive factors for difficult intravenous cannulation in pediatric patients at a tertiary pediatric hospital. Paediatr Anaesth 22:223–229
Geremia C, De Ioris MA, Crocoli A et al (2017) Totally implantable venous access devices in children with medical complexity: preliminary data from a tertiary care hospital. J Vasc Access 18:426–429
Sparks LA, Setlik J, Luhman J (2007) Parental holding and positioning to decrease IV distress in young children: a randomized controlled trial. J Pediatr Nurs 22:440–447
Chait PG, Temple M, Connolly B et al (2002) Pediatric interventional venous access. Tech Vasc Interv Radiol 5:95–102
Vo JN, Hoffer FA, Shaw DW (2010) Techniques in vascular and interventional radiology: pediatric central venous access. Tech Vasc Interv Radiol 13:250–257
Lorenz JM, Funaki B, Van Ha T, Leef JA (2001) Radiologic placement of implantable chest ports in pediatric patients. AJR Am J Roentgenol 176:991–994
Radomski M, Zeh HJ, Edington HD et al (2016) Prolonged intralymphatic delivery of dendritic cells through implantable lymphatic ports in patients with advanced cancer. J Immunother Cancer 4:24
Tchirikov M, Zhumadilov ZS, Bapayeva G et al (2017) The effect of intraumbilical fetal nutrition via a subcutaneously implanted port system on amino acid concentration by severe IUGR human fetuses. J Perinat Med 45:227–236
Wang KW, Barnard A (2004) Technology-dependent children and their families: a review. J Adv Nurs 45:36–46
Feudtner C, Villareale NL, Morray B et al (2005) Technology-dependency among patients discharged from a children's hospital: a retrospective cohort study. BMC Pediatr 5(8)
Rauch D, Dowd D, Eldridge D et al (2009) Peripheral difficult venous access in children. Clin Pediatr 48:895–901
Khalilzadeh O, Baerlocher MO, Shyn PB et al (2017) Proposal of a new adverse event classification by the Society of Interventional Radiology Standards of practice committee. J Vasc Interv Radiol 28:1432–1437
Centers for Disease Control (2018) Bloodstream infection event (central line-associated bloodstream infection and non-central line associated bloodstream infection). https://www.cdc.gov/nhsn/pdfs/pscmanual/4psc_clabscurrent.pdf. Accessed 5 June 2019
Duesing LA, Fawley JA, Wagner AJ (2016) Central venous access in the pediatric population with emphasis on complications and prevention strategies. Nutr Clin Pract 31:490–501
Ashton D, Variyam D, Hernandez JA et al (2017) Single-incision versus conventional technique for tunneled central line placement in children. Cardiovasc Intervent Radiol 40:1552–1558
Yeste Sanchez L, Galbis Caravajal JM, Fuster Diana CA, Moledo Eiras E (2006) Protocol for the implantation of a venous access device (port-a-cath system). The complications and solutions found in 560 cases. Clin Transl Oncol 8:735–741
Tofani BF, Rineair SA, Gosdin CH et al (2012) Quality improvement project to reduce infiltration and extravasation events in a pediatric hospital. J Pediatr Nurs 27:682–689
Doellman D, Hadaway L, Bowe-Geddes LA et al (2009) Infiltration and extravasation: update on prevention and management. J Infus Nurs 32:203–211
Simona R (2012) A pediatric peripheral intravenous infiltration assessment tool. J Infus Nurs 35:243–248
Venturini E, Montagnani C, Benni A et al (2016) Central-line associated bloodstream infections in a tertiary care children's university hospital: a prospective study. BMC Infect Dis 16:725
Wagner M, Bonhoeffer J, Erb TO et al (2011) Prospective study on central venous line associated bloodstream infections. Arch Dis Child 96:827–831
Gilbert RE, Mok Q, Dwan K et al (2016) Impregnated central venous catheters for prevention of bloodstream infection in children (the CATCH trial): a randomised controlled trial. Lancet 387:1732–1742
Shim J, Seo TS, Song MG et al (2014) Incidence and risk factors of infectious complications related to implantable venous-access ports. Korean J Radiol 15:494–500
Wolf J, Curtis N, Worth LJ, Flynn PM (2013) Central line–associated bloodstream infection in children: an update on treatment. Pediatr Infect Dis J 32:905–910
Riker MW, Kennedy C, Winfrey BS et al (2011) Validation and refinement of the difficult intravenous access score: a clinical prediction rule for identifying children with difficult intravenous access. Acad Emerg Med 18:1129–1134
Hartman JH, Baker J, Bena JF et al (2018) Pediatric vascular access peripheral IV algorithm success rate. J Pediatr Nurs 39:1–6
Yen K, Riegert A, Gorelick M (2008) Derivation of the DIVA score: a clinical prediction rule for the identification of children with difficult intravenous access. Pediatr Emerg Care 24:143–147
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pezeshkpour, P., Armstrong, N.C., Mahant, S. et al. Evaluation of implanted venous port-a-caths in children with medical complexity and neurologic impairment. Pediatr Radiol 49, 1354–1361 (2019). https://doi.org/10.1007/s00247-019-04470-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-019-04470-w