Abstract
Background
Most children have a successful outcome after a pull-through for Hirschsprung’s disease. Some may have persisting symptoms after the pull-through. They could be managed conservatively, need minor surgical procedures, or a redo pull-through will be required. In this study, we presented our results in the management of the obstructive complications after pull-through for Hirschsprung’s disease.
Results
During the specified time period from January 2011 to December 2015, 21 patients presented to our department with persistent constipation or recurrent enterocolitis after a pull-through for Hirschsprung’s disease. Their age ranged between 4 months and 5 years (mean 2 years, median 2.5 years). They were 13 males and 8 females. Eleven patients underwent initial trans-anal endorectal pull-through, 4 underwent Duhamel procedure, and 6 underwent abdominal Soave technique. Three of the 11 patients with initial trans-anal endorectal pull-through had a tight anastomotic stricture which responded well to dilatation, 2 had a long muscular cuff which was incised laparoscopically, 4 had spasm of the internal anal sphincter which was relieved by sphincterotomy, and 2 had residual aganglionosis which required a redo pull-through. Two of the 4 patients who underwent initial Duhamel procedure had a long spur which was divided using a stapler, and the other 2 patients had residual aganglionosis which required a redo pull-through. One of the 6 patients who underwent abdominal Soave technique developed a long tight stricture and required a redo pull-through; in 1 patient, biopsy confirmed hypoganglionosis of the whole colon and was managed medically, and 4 patients had spasm of the internal anal sphincter which was relieved in 1 of them by sphincterotomy and in 2 by botulinum toxin injection while the remaining patient did not improve by either sphincterotomy or botulinum toxin injection.
Conclusion
Persistent constipation or recurrent enterocolitis after pull-through for Hirschsprung’s disease should be managed according to the cause; they could be managed medically by simple surgical procedures, or a redo pull-through may be required.
Similar content being viewed by others
Background
Operations done for the management of Hirschsprung’s disease have generally a good outcome. About 32% of children have complications after a pull-through for Hirschsprung’s disease [1]. These complications may be persistent constipation, recurrent enterocolitis, or stool incontinence [2].
The cause of these complications may be a functional problem in the whole colon, anastomotic stricture, long obstructing seromuscular cuff, long spur after a Duhamel procedure, twisted pull-through, spasm of the internal anal sphincter, or residual aganglionosis [3].
These complications can be managed medically using drugs which improve the intestinal motility, by simple surgical procedures like dilatation of a stricture, splitting of a long obstructing seromuscular cuff, division of a spur, sphincterotomy, botulinum toxin injection, or a redo pull-through procedure may be the only option to relieve the child complaint [4, 5].
In this study, we presented our results in the management of the obstructive complications after pull-through for Hirschsprung’s disease.
Methods
During the period from January 2011 to December 2015, and after approval of the institutional review board, patients presented with persistent constipation or recurrent enterocolitis after a pull-through for Hirschsprung’s disease were collected from the Pediatric Surgery Department, Faculty of Medicine, Ain Shams University.
Type of the primary pull-through, ability to pass stool spontaneously after the operation, and the frequency of enterocolitis were recorded. The patients were evaluated by clinical examination, per-rectal (P/R) examination, gastrografin enema, and rectal or colonic biopsy if needed.
The patients were followed up for 2 years to ensure the resolution of constipation and enterocolitis after the intervention is done.
Results
During the specified time period, 21 patients presented to our department with persistent constipation or recurrent enterocolitis after a pull-through for Hirschsprung’s disease. Their age ranged between 4 months and 5 years (mean 2 years, median 2.5 years). They were 13 males and 8 females. Eleven patients underwent initial trans-anal endorectal pull-through, 4 underwent Duhamel procedure, and 6 underwent abdominal Soave technique.
Three of the 11 patients with initial trans-anal endorectal pull-through had a tight anastomotic stricture which responded well to dilatation, 2 had a long muscular cuff (Fig. 1) which was incised laparoscopically, 4 had spasm of the internal anal sphincter which did not respond well to botulinum toxin injection and was relieved by lateral sphincterotomy, and 2 had residual aganglionosis which required a redo pull-through (trans-anal endorectal pull-through).
Two of the four patients who underwent initial Duhamel procedure had a long spur (Fig. 2) which was divided using a gastrointestinal anastomosis (GIA) stapler, and the other two patients had residual aganglionosis which required a redo pull-through (abdominal assisted pull-through).
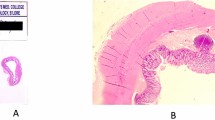
One of the six patients who underwent abdominal Soave technique developed a tight long stricture (Fig. 3) and required a redo pull-through (abdominal assisted pull-through); in one patient, biopsy confirmed hypoganglionosis of the whole colon and was managed medically by pyridostigmine, and four patients had spasm of the internal anal sphincter which was relieved in two of them by botulinum toxin injection and in one by lateral sphincterotomy after no response to botulinum toxin injection and in two by botulinum toxin injection while the remaining patient did not improve by either sphincterotomy or botulinum toxin injection and is still on enemas.
During the follow-up period, 20/21 patients (95%) were not of the patients was on laxatives or enemas and they did not have constipation or enterocolitis.
Discussion
Postoperative complications after pull-through for Hirschsprung’s disease can occur in a considerable number of patients. The incidence of these complications varied between 0 and 80% [6]. The most common complications after pull-through are anastomotic stricture, long obstructing seromuscular cuff, long spur after a Duhamel procedure, twisted pull-through, or retained aganglionosis. The clinical manifestations of these complications are persistent constipation, recurrent enterocolitis, or stool incontinence [7].
Management of these complications varied between medical treatment, simple surgical procedures, and redo pull-through. Strictures could be managed initially by serial dilatations. They responded to this simple technique if they were short strictures. However, long strictures could not be managed by dilatation and required redo pull-through [8]. In our series, four patients developed anastomotic stricture after an endorectal trans-anal pull-through. Three of whom responded well to the repeated dilatation, while one patient with a long anastomotic stricture did not respond to the dilatation and a redo pull-through was done.
Long obstructing seromuscular cuff after a pull-through could be managed by a simple division of this cuff. Laparoscopy offered the advantage of being a minimally invasive technique with good results in this aspect [9, 10]. In our series, two patients had this complication after a trans-anal endorectal pull-through and, both were managed successfully by laparoscopic division of the obstructing cuff.
The long spur after Duhamel procedure is a frequently encountered complication. This long spur leads to obstructive symptoms and subsequent recurrent enterocolitis. It could be managed effectively by simple division of this spur, and the gastrointestinal anastomosis (GIA) stapler could be used for this purpose with good results [11]. In our series, two patients had this complication and were successfully managed by this technique.
Retained aganglionosis is an absolute indication for redo pull-through. It represented the most common cause of redo procedures in most series. Soave, Swenson, or Duhamel could be done in the reoperation [12, 13]. In our series, four patients had retained aganglionosis and redo pull-through was required in all of them. The redo procedure was trans-anal endorectal pull-through in the two who underwent initial trans-anal endorectal pull-through and abdominal assisted pull-through in the two who underwent initial Duhamel procedure.
Pyridostigmine is a cholinesterase inhibitor which improves intestinal motility by increasing the availability of acetylcholine. A lot of articles proved its efficacy in the treatment of severe constipation and pseudo-obstruction [14, 15]. In our series, the patient with persistent constipation after abdominal Soave procedure and colonic hypoganglionosis on biopsy improved markedly after treatment with pyridostigmine.
Spasm of the internal anal sphincter may occur after a pull-through for Hirschsprung’s disease. The lines of its management are botulinum toxin injection, nitroglycerine paste, or sphincterotomy. Botulinum toxin inhibits the release of acetylcholine which leads to the relaxation of the sphincter. Sphincterotomy was first described for the treatment of short-segment Hirschsprung’s disease, but it had been also of benefit in the treatment of stooling problem after pull-through for Hirschsprung’s disease [8]. In our series, botulinum toxin injection was effective in managing persistent constipation after pull-through in two patients (they were under the age of 1 year), while five patients did not respond to injection and the constipation was relieved only after lateral sphincterotomy (they were above the age of 1 year); the remaining patient did not respond to either lines of treatment and is still on enemas. In those patients, no abnormality was found in the per-rectal examination, gastrografin enema, or biopsy.
However, the study is limited by the small number of patients involved, and further studies are required to evaluate the effect of the minimally invasive techniques in the management of complicated cases of Hirschsprung’s disease.
Conclusion
Persistent constipation or recurrent enterocolitis after pull-through for Hirschsprung’s disease should be managed according to the cause; they could be managed medically, by simple surgical procedures, or a redo pull-through may be required.
Availability of data and materials
The datasets used and/or analyzed during this study are available from the corresponding author on reasonable request.
Abbreviations
- GIA:
-
Gastrointestinal anastomosis
References
Menezes M, Corbally M, Puri P. Long-term results of bowel function after treatment for Hirschsprung’s disease: a 29-year review. Pediatr Surg Int. 2006;22(12):987–90. https://doi.org/10.1007/s00383-006-1783-8 PMID: 17006709.
Obermayr F, Hacker HW, Bornemann A, Stern M, Fuchs J. Redo-endorectal pull through following various pull through procedures in Hirschsprung’s disease. Langenbeck’s Arch Surg. 2008;393(4):493–9. https://doi.org/10.1007/s00423-007-0259-1 PMID: 18172678.
Ralls MW, Freeman JJ, Rabah R, Coran AG, Ehrlich PF, Hirschl RB, Teitelbaum DH. Redo pullthrough for Hirschsprung disease: a single surgical group’s experience. J Pediatr Surg. 2014;49(9):1394–9. https://doi.org/10.1016/j.jpedsurg.2014.04.009 PMID: 25148745.
Sheng Q, Lv Z, Xiao X. Re-operation for Hirschsprung’s disease: experience in 24 patients from China. Pediatr Surg Int. 2012;28(5):501–6. https://doi.org/10.1007/s00383-012-3062-1 PMID: 22358253.
Hassan H, Hashish A, Fayad H, Elian A, Elatar A, Afify M, Elhalaby E. Redo surgery for Hirschsprung’s disease. Ann Pediatr Surg. 2008;4(1):42–50.
Hadidi A, Bartoli F, Waag KL. Role of transanal endorectal pull-through in complicated Hirschsprung’s disease: experience in 18 patients. J Pediatr Surg. 2007;42(3):544–8. https://doi.org/10.1016/j.jpedsurg.2006.10.047 PMID: 17336196.
Peña A, Elicevik M, Levitt MA. Reoperations in Hirschsprung disease. J Pediatr Surg. 2007;42(6):1008–13. https://doi.org/10.1016/j.jpedsurg.2007.01.035 PMID: 17560211.
Ralls MW, Coran AG, Teitelbaum DH. Reoperative surgery for Hirschsprung disease. Semin Pediatr Surg. 2012;21(4):354–63. https://doi.org/10.1053/j.sempedsurg.2012.07.011 PMID: 22985841.
Abdel Hay S, El Shafei I, El Debeky M, Bassiouny A. Release of obstructing rectal cuff following transanal endorectal pullthrough for Hirschsprung’s disease: a laparoscopic approach. Ann Pediatr Surg. 2012;8(3):90–2. https://doi.org/10.1097/01.XPS.0000414815.73698.43.
Temple SJ, Shawyer A, Langer JC. Is daily dilatation by parents necessary after surgery for Hirschsprung disease and anorectal malformations? J Pediatr Surg. 2012;47(1):209–12. https://doi.org/10.1016/j.jpedsurg.2011.10.048 PMID: 22244419.
Langer JC, Rollins MD, Levitt M, Gosain A, Torre L, Kapur RP, Cowles RA, Horton J, Rothstein DH, Goldstein AM, American Pediatric Surgical Association Hirschsprung Disease Interest Group. Guidelines for the management of postoperative obstructive symptoms in children with Hirschsprung disease. Pediatr Surg Int. 2017;33(5):523–6. https://doi.org/10.1007/s00383-017-4066-7 PMID: 28180937.
Aggarwal SK, Yadav S, Goel D, Sengar M. Combined abdominal and posterior sagittal approach for redo pull-through operation in Hirschsprung’s disease. J Pediatr Surg. 2002;37(8):1156–9 PMID: 12149692.
Pini-Prato A, Mattioli G, Giunta C, Avanzini S, Magillo P, Bisio GM, Jasonni V. Redo surgery in Hirschsprung disease: what did we learn? Unicentric experience on 70 patients. J Pediatr Surg. 2010;45(4):747–54. https://doi.org/10.1016/j.jpedsurg.2009.08.001 PMID: 20385282.
O’Dea CJ, Brookes JH, Wattchow DA. The efficacy of treatment of patients with severe constipation or recurrent pseudo-obstruction with pyridostigmine. Color Dis. 2010;12(6):540–8. https://doi.org/10.1111/j.1463-1318.2009.01838.x PMID: 19508545.
Bharucha AE, Low PA, Camilleri M, Burton D, Gehrking TL, Zinsmeister AR. Pilot study of pyridostigmine in constipated patients with autonomic neuropathy. Clin Auton Res. 2008;18(4):194–202. https://doi.org/10.1007/s10286-008-0476-x PMID: 18622640. PMCID: PMC2536749.
Acknowledgements
Not applicable.
Funding
This study had no funding from any source.
Author information
Authors and Affiliations
Contributions
ME gave the idea and collected the patients’ data and analyzed them and wrote the paper with revisions. SA put the study design and followed the patients postoperatively. Both authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the research ethics committee of the Faculty of Medicine at Ain Shams University in Egypt on 25 December 2010. Written informed consent for participation in the study was given by the patients’ parents or their legal guardians.
Consent for publication
Written informed consent for the publication of this data was given by the patients’ parents or their legal guardians.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Elsherbeny, M., Abdelhay, S. Obstructive complications after pull-through for Hirschsprung’s disease: different causes and tailored management. Ann Pediatr Surg 15, 2 (2019). https://doi.org/10.1186/s43159-019-0003-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43159-019-0003-y