Abstract
Purpose
To share our experience in the surgical management of patients with Hirschsprung disease (HD) using the trans-anal endorectal pull-through “Soave” technique.
Methods
The study included cases diagnosed as HD who were operated during the period 2008 through 2018. Cases of total colonic aganglionosis were excluded to be discussed in a separate report.
Results
The study included 67 consecutive cases of HD. All included cases underwent trans-anal endorectal pull-through which was purely trans-anal in 31 (46%), while abdominal-assisted trans-anal endorectal pull-through was applied in the remaining (54%). Early postoperative complications included 2 cases of partial dehiscence at the colo-anal anastomosis; 1 of them deteriorated after re-exploration and unfortunately died. Twenty-six cases were available to assess functional outcomes after corrective surgery. Their age at follow-up ranged between 44 months and 17 years (mean = 78.8 months; median = 72 months). All cases achieved voluntary defecation. However, fecal soiling was a common finding after surgery for HD (69%). Constipation was another common postoperative finding (73%). Lastly, a history of attacks of postoperative enterocolitis was prevalent in 19 cases (73%), which ranged between 1 and 7 attacks usually in the first 2 years after the operation.
Conclusion
The trans-anal endorectal pull-through provides an effective surgical treatment for Hirschsprung disease. The high prevalence of fecal soiling after surgery highlights the importance of long-term follow-up to provide the required support for these patients during adolescence and transition into adulthood.
Similar content being viewed by others
Background
Hirschsprung disease (HD) is a rare congenital disease with a reported incidence of about 1:5000 live births [1]. During fetal life, failure of migration of neural crest-derived cells along the gut results in distal intestinal aganglionosis essentially affecting the rectum and variable length of the distal colon. HD is classified according to the length of the aganglionic bowel segment into short-segment HD (recto-sigmoid, 75%), long-segment HD (extending proximal to the sigmoid colon, 15%), and other rare forms that may exist as total colonic or total intestinal aganglionosis (10%) [2, 3]. Dysfunction of the affected bowel segment involves motility, secretion, and barrier functions, which are under the control of the enteric nervous system [2]. Typically, the disease is manifested by constipation, abdominal distension, and intestinal obstruction. HD is considered a debilitating disease which can be fatal if untreated. However, advances in diagnosis and surgical treatment dramatically reduced morbidity and mortality [3].
The disease is named after Harald Hirschsprung who early reported on a case of constipation due to dilatation and hypertrophy of the colon in 1886 [4]. In 1948, Orvar Swenson described the narrowing of the distal colon (absent peristalsis) and suggested that removal of this colonic segment would provide a surgical cure for HD [5]; the disease then became of great interest to pediatric surgeons all over the world. Franco Soave (1964) introduced the idea of endorectal pull-through by dissecting the surgical plane between the mucosa and the muscle of the rectum in order to protect the nearby pelvic nerves and genitourinary structures [5]. Later in 1998, Luis de la Torre modified Soave’s procedure by performing a single-stage trans-anal endorectal pull-through [6].
In this retrospective study, we would like to share our experience in the surgical management of patients with HD applying the trans-anal endorectal pull-through (Soave’s procedure) whether as a purely trans-anal or abdominally assisted approach.
Methods
The study included cases diagnosed as HD who were operated during the period 2008 through 2018. Cases of total colonic aganglionosis were excluded to be discussed in a separate report. Data retained by the author were retrospectively analyzed and included demographic data (sex, age at operation), investigations, operative details, and short-term outcomes. The study was conducted after internal review board approval.
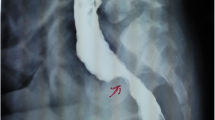
The typical presentation included delayed passage of meconium, constipation, and abdominal distension, while some cases presented with neonatal intestinal obstruction and bilious vomiting. The diagnosis was usually confirmed by the typical findings in contrast enema studies, which has the additional benefit of determining the extent of aganglionic (spastic) bowel segment (Fig. 1). However, there is almost a consensus on the necessity of obtaining pre-operative histopathological evidence of HD, which requires a rectal biopsy. The latter may be performed as a bedside suction biopsy; however, only full-thickness rectal biopsy was available at our facility. Few cases, who were not doing well (e.g., bowel perforation), underwent exploration and leveling colostomy as an initial step before corrective surgery.
Trans-anal endorectal pull-through (Soave’s procedure) [6]
Position
The procedure was performed either in the prone or supine lithotomy position (Fig. 2) [7]. The former position may be preferred for a pure trans-anal procedure. However, for patients with colostomy or when expected to need additional laparotomy for mobilization of the colon from above, the supine position was definitely advantageous.
Anal retraction
Early during the study period, we used simple stitches to retract/open the anus allowing for trans-anal (endo-rectal) dissection (Fig. 2). Later, we shifted to using the Lone-Star retractor (when it became available, Fig. 3), which provided better exposure for trans-anal dissection compared to simple stitches. The latter was noticed to evert the anus rather than providing optimal retraction.
Trans-anal excision of aganglionic rectum
We start by submucosal injection of adrenaline/saline solution (1/200,000) in different quadrants above the dentate line (Fig. 3). This has the dual benefit of inducing hydro-dissection and minimizing bleeding. A circular mucosal incision is made 2 cm above the dentate line via a needle monopolar diathermy. Multiple stay sutures help to distribute the tension on the anal mucosa during traction. The first few centimeters of the rectum (3–7 cm) are excised via submucosal dissection before we shift to full-thickness excision (Fig. 4). The retained muscular cuff of the rectum is incised posteriorly; sometimes, we excise a strip of this muscle cuff. We continue to excise the abnormal/spastic bowel till we reach a healthy segment of the colon 7–10 cm above the characteristic “funnel” of the transitional zone. The latter was usually obvious at operation and well-consistent with the pre-operative imaging findings (Fig. 5) [8]. Intra-operative histopathological analysis (frozen section) to determine the level of the healthy proximal colonic segment for the pull-through was not our routine practice; however, this was occasionally essential and helpful when there was no consensus on the level of the transitional zone in the pre-operative imaging.
Excised specimens in three different cases of Hirschsprung disease who underwent trans-anal endorectal pull-through (a–c). The first few centimeters of the rectum (3–7 cm) are excised via submucosal dissection before we shift to full-thickness excision. Note the variable length of submucosal dissection of the rectum (double arrowhead dotted line). Recently, there is a tendency to do less submucosal dissection in order to leave a shorter muscle cuff. d, e The contrast enema of cases a and c, respectively, are presented for comparing the operative findings with preoperative imaging. Note: contrast enema of case b was not available
Trans-anal endorectal pull-through (Soave’s procedure) in two different cases of Hirschsprung disease. a, c The preoperative contrast enema showing the level of the transitional zone in the two cases. b, d The operative findings in the two cases, which proved to be well consistent with the preoperative imaging findings
Before turning to the final step of the procedure (colo-anal anastomosis), we had to straighten the retained rectal muscular cuff (make sure it is not rolled upon itself) to avoid postoperative obstruction. Also, it may be useful to add a layer of interrupted seromuscular stitches fixing the pulled-through colon/neorectum to the retained muscle cuff at a deeper level to the final colo-anal anastomosis.
Cases with colostomy or abdominal-assisted trans-anal pull-through
In the supine lithotomy position, we start by taking down the colostomy and/or mobilization of the colon making sure to preserve the marginal vessels to ensure reliable blood supply to the pulled-through colon. In addition to cases with colostomy, assistance via laparotomy was indicated for cases with long aganglionic segment and/or severely distended colon (Fig. 1c). The laparotomy incision was usually a left lower transverse (muscle splitting) incision. Alternatively, a lower midline incision may be used which has the advantage of easy extension to the upper abdomen as needed (e.g., mobilization of splenic flexure). In all cases, the laparotomy incision was used to ensure adequate mobilization of the colon, while the trans-anal part of the procedure was completed as previously described.
Early postoperative care
Usually, enteral feeding is resumed gradually on the 2nd or 3rd postoperative day. With the progression of feeding, abdominal distension is not uncommon; this is managed by temporarily withholding oral intake and maybe gentle insertion of a soft rectal tube. Most patients will have reached full oral intake to be discharged on the 7th to 10th postoperative day. Rectal examination should be performed routinely at follow-up visits (starting 2–3 weeks postoperatively) to check for possible narrowing at the colo-anal anastomosis.
Intermediate and long-term follow-up
Parents of operated cases were contacted via their registered phone numbers. They were informed about the study and were encouraged to visit the outpatient clinic to assess functional outcomes following corrective surgery.
Results
The study included 67 consecutive cases of HD (excluding total colonic aganglionosis) that were operated during the period 2008 through 2018. Their age at the time of corrective surgery ranged between 1 and 72 months (mean = 11.8 months, median = 6 months). As already known [1], there was obvious male predominance (56 cases were males, 83%). In this series, only 2 cases were diagnosed as long-segment HD with an aganglionic segment extending proximal to the sigmoid colon (up to the splenic flexure and transverse colon), while the rest of the cases were rectosigmoid HD (97%) (Fig. 1). Nine cases (13.4%) underwent colostomy as an initial procedure before the corrective surgery. All included cases underwent trans-anal endorectal pull-through (Soave procedure) [6, 7] which was purely trans-anal in 31 (46%), while in the remaining (including 9 cases with colostomy), assistance through a laparotomy incision was required (abdominal assisted trans-anal Soave, 54%).
The early postoperative period went smoothly in all but two cases. The first case was a girl who had a leveling pelvic colostomy initially performed before the definitive surgery. Later at the age of 6 years, she underwent abdominal-assisted trans-anal endorectal pull-through, when she presented on the 11th postoperative day (3 days after discharge from the hospital) with a picture of pelvic infection: fever and abdominal distension with mild tenderness, while ultrasound examination showed mild pelvic collection. A decision was taken to explore the abdomen for fear of leakage at the anastomotic site. At exploration, the abdomen was clean with few flakes of pus in the pelvis. Under general anesthesia, the colo-anal anastomosis was inspected through the anus showing partial posterior dehiscence which was left uninterrupted. A diverting proximal transverse colostomy was performed with smooth postoperative recovery. Two months later, rectal examination and distal colon contrast studies confirmed complete/good healing at the colo-anal anastomosis when a decision was made to close the colostomy. Postoperative recovery went uneventful, and the patient showed good functional outcomes at follow-up (she had voluntary defecation without fecal soiling).
The second case was a 1-year-old boy (Down syndrome) diagnosed with rectosigmoid HD who underwent primary abdominal-assisted trans-anal Soave. The patient developed insidious abdominal distension; a decision was made on the fifth postoperative day to withhold oral intake which did not improve the condition. A rectal tube was inserted but failed to relieve the distension. Masked by the laxity of his abdomen (Down syndrome), the condition passed unnoticed for 2 days before we discovered that the rectal tube has perforated into the peritoneal cavity through partial dehiscence at the colo-anal anastomosis. A decision was made for fecal diversion. At exploration, there were scattered flakes of pus between the intestines. Peritoneal lavage and diverting transverse colostomy were performed; however, the patient’s general condition rapidly deteriorated and died 2 days later.
Functional outcome
Among the cases who were successfully contacted by phone, 26 cases responded and were available to assess the functional outcome after corrective surgery. Their age at follow-up ranged between 44 months and 17 years (mean = 78.8 months; median = 72 months).
Fecal continence was evaluated according to the Krickenbeck postoperative assessment protocol (Table 1) [9]. Obstructive symptoms were evaluated by asking about attacks of postoperative enterocolitis (abdominal distension, loose offensive stools, vomiting). The severity of the latter was judged by the necessity of hospital admission. Table 2 summarizes the data of the 26 patients who were available at follow-up. Although all cases achieved voluntary defecation as older children, yet fecal soiling was a common finding after surgery for HD (69%). We could differentiate between 2 types of fecal soiling. The first was during the daytime when the child was awake, and this was graded according to the Krickenbeck system. Most cases with daytime soiling (14/16; 87.5%) had mild (grade 1, occasional) soiling. The second type of fecal soiling was nocturnal when the child was asleep, which was reported in 8 cases. Constipation was another common postoperative finding (73%). Lastly, a history of attacks of postoperative enterocolitis was prevalent in 19 cases (73%), which ranged between 1 and 7 attacks usually in the first 2 years after the operation (Table 2).
Discussion
Hirschsprung disease is one important cause of lower intestinal obstruction and constipation in the pediatric age group. Usually, the disease can be cured by surgery with reported fair outcomes especially among those with typical rectosigmoid disease [10]. Successive efforts of scientists and researchers in the field have caused major advances in the diagnosis and surgical treatment. Transplantation of enteric neuronal stem cells into the aganglionic gut is still under investigation in animal models, which may open a new era for the potential cure of HD without invasive surgery [2].
The trans-anal approach for resection of the distal aganglionic bowel segment represented a breakthrough in the surgical management of HD [6, 7]. While applying Soave’s principle of submucosal (endorectal) resection of the rectum, the trans-anal approach rapidly gained widespread acceptance to become the most popular choice whether as pure trans-anal or abdominal assisted. The latter has been advocated to avoid the limitations associating the pure trans-anal approach, which in certain situations can hinder the effective mobilization of the colon and affect the judgment on the level of the dilated segment and transitional zone before the start of dissection. More recently, some authors encourage adding laparoscopy routinely to the trans-anal approach in all cases of HD [11]. Moreover, some authors shifted to Swenson’s principle (full-thickness resection of the rectum from the start) through the same trans-anal approach to avoid potential complications of the retained rectal muscle cuff [7, 12].
The transformation to minimally invasive techniques (trans-anal resection/laparoscopy) has contributed to improving outcomes and decreasing surgical morbidity. More attention has been directed to the preservation of continence and improving quality of life. As the rectum is essentially excised in the corrective surgery for HD, preservation of the anal canal becomes of utmost importance. Regardless of the age at operation, some experts recommend preserving at least 1.5–2 cm of the anal canal above the dentate line. Others highlight the benefit of advancing the hooks of the Lone-Star retractor to protect the anal canal during the early beginning of dissection [13]. While these recommendations appear to improve the potential for fecal continence, we may expect more patients to present with postoperative obstructive symptoms and enterocolitis [14]. Postoperative Botox injection of the anal sphincters has been used more liberally in recent literature with promising results in controlling such postoperative obstructive symptoms [15].
In this case series, the trans-anal endorectal pull-through was an effective technique to treat patients with HD, which was associated with a low incidence of complications and a fair functional outcome. The postoperative complications were restricted to partial dehiscence at the colo-anal anastomosis in two cases (3%). Despite the uncommon occurrence of complications, still a high index of suspicion and prompt active surgical management remain the only way to avoid rapid deterioration and losing the child. Patients with HD appear to be more vulnerable pediatric surgical patients that can deteriorate rapidly due to associated defective intestinal functions; the condition may be even worse with the association of Down syndrome and HD, which has been reported to be associated with higher morbidity and mortality [16].
Fecal soiling is a common functional problem after operations for HD [10, 13, 17, 18]. Variable rates have been reported in the literature ranging between 1.5 and 55% [18, 19]. In their review article, Ahmed et al. reported approximately 40% rate of fecal incontinence among children after HD pull-through [17]. In our study, all cases who were available at follow-up achieved voluntary defecation as older children; however, postoperative fecal soiling was still very common (69%). Although this percentage appears higher than what has been reported in the literature, fecal soiling was mostly mild (occasional) and did not cause major social problems; almost all cases were regularly attending their schools without restrictions. There are several causes for fecal soiling after pull-through operations for HD that are broadly categorized by experts as abnormalities in sensation, abnormalities in sphincter control, and pseudo-incontinence (due to fecal impaction or hypermotility) [20]. Nocturnal fecal soiling appears to be a peculiar symptom with HD that needs deeper analysis searching for practical solutions. In their report, Saadai et al. [20] suggested an algorithm for the diagnosis and management of a child with soiling after a pull-through for HD. The high prevalence of fecal soiling after operations for HD highlights the importance of long-term follow-up to provide the required support for these patients during adolescence and transition into adulthood [10]. Another important issue after operations for HD is the obstructive symptoms and Hirschsprung-associated enterocolitis [21]. It is important to educate parents about this serious problem. Prompt deflation of the colon (soft rectal tubes), antibiotic treatment, the alarming signs, and when there is a need for hospital admission are important issues to be discussed with the parents before discharge from the hospital.
The study is limited by its retrospective nature lacking planned follow-up details and being restricted to a single center. Although digital storing of data was helpful in collecting a relatively good number of consecutive cases that were operated by the same technique over a long period of time, some diagnostic investigations were missing at the time of writing this report. Some of the cases were contacted by phone and were available to assess functional outcomes several years after the corrective surgery; however, these represented only 38% of operated cases. Lastly, more focus should be directed to long-term follow-up that can help to provide counseling regarding the high prevalence of fecal soiling.
Conclusion
The trans-anal endorectal pull-through provides an effective surgical treatment for Hirschsprung disease. Despite the uncommon occurrence of postoperative complications, a high index of suspicion and prompt surgical management is crucial to deal successfully with such complications when it occurs. The high prevalence of fecal soiling after surgery highlights the importance of long-term follow-up to provide the required support for these patients during adolescence and transition into adulthood.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Puri P, Nakamura H (2019) Epidemiology and clinical characteristics of Hirschsprung’s disease. In: Puri P (editor). Hirschsprung’s disease and allied disorders. Springer Nature Switzerland AG 167–174. https://doi.org/10.1007/978-3-030-15647-3_10
Mueller JL, Goldstein AM (2022) The science of Hirschsprung disease: what we know and where we are headed. Semin Pediatr Surg 31:151157. https://doi.org/10.1016/j.sempedsurg.2022.151157
Heuckeroth RO (2022) Hirschsprung disease. In: Faure C, Thapar N, Lorenzo CD. Pediatric Neurogastroenterology. Gastrointestinal motility disorders and disorders of gut brain interaction in children. Springer Nature Switzerland AG 355–370. https://doi.org/10.1007/978-3-031-15229-0_26
Höllwarth ME, Grosfeld JL (2019) Hirschsprung’s disease: a historical perspective – 1691–2018. In: Puri P (editor). Hirschsprung’s disease and allied disorders. Springer Nature Switzerland AG 1–18. https://doi.org/10.1007/978-3-030-15647-3_1
Jensen AR, Frischer JS (2022) Surgical history of Hirschsprung disease. Semin Pediatr Surg 31:151174. https://doi.org/10.1016/j.sempedsurg.2022.151174
De la Torre-Mondragon L, Ortega-Salgado JA (1998) Transanal endorectal pull-through for Hirschsprung’s disease. J Pediatr Surg 33:1283–1286
Langer JC (2022) Surgical approach to Hirschsprung disease. Semin Pediatr Surg 31:151156. https://doi.org/10.1016/j.sempedsurg.2022.151156
Proctor ML, Traubici J, Langer JC et al (2003) Correlation between radiographic transition zone and level of aganglionosis in Hirschsprung’s disease: implications for surgical approach. J Pediatr Surg 38:775–778
Holschneider A, Hutson J, Pena A et al (2005) Preliminary report on the international conference for the development of standards for the treatment of anorectal malformations. J Pediatr Surg 40:1521–1526
Short SS, Durham MM, Rollins MD (2022) Hirschsprung disease outcomes. Semin Pediatr Surg 31:151160. https://doi.org/10.1016/j.sempedsurg.2022.151160
Nasr A, Haricharan RN, Gamarnik J, Langer JC (2014) Transanal pullthrough for Hirschsprung disease: matched case-control comparison of Soave and Swenson techniques. J Pediatr Surg 49(5):774–776
Feng J, Li T, Li N (2019) Laparoscopically assisted pull-through operation for Hirschsprung’s disease. In: Puri P (editor). Hirschsprung’s disease and allied disorders. Springer Nature Switzerland AG 357–372. https://doi.org/10.1007/978-3-030-15647-3_24
Rentea RM, Snyder CL (2019) Early and late complications following pull-through operation for Hirschsprung’s disease. In: Puri P (editor). Hirschsprung’s disease and allied disorders. Springer Nature Switzerland AG 383–402. https://doi.org/10.1007/978-3-030-15647-3_26
Yamataka A, Takeda M, Yazaki Y (2019) Transanal pull-through with or without laparoscopic assistance for rectosigmoid Hirschsprung’s disease. In: Puri P (editor). Hirschsprung’s disease and allied disorders. Springer Nature Switzerland AG 345–356. https://doi.org/10.1007/978-3-030-15647-3_23
Svetanoff WJ, Lim-Beut IP, Wood R et al (2022) The utilization of botulinum toxin for Hirschsprung disease. Semin Pediatr Surg 31:151161. https://doi.org/10.1016/j.sempedsurg.2022.151161
Caniano DA, Teitelbaum DH, Qualman SJ (1990) Management of Hirschsprung’s disease in children with trisomy 21. Am J Surg 159:402–404
Ahmed H, Yacob D, Halleran DR et al (2022) Evaluation and treatment of the post pull-through Hirschsprung patient who is not doing well; update for 2022. Semin Pediatr Surg 31:151164. https://doi.org/10.1016/j.sempedsurg.2022.151164
Westfal ML, Okiemy O, Chung PHY et al (2022) Optimal timing for soave primary pull-through in short-segment Hirschsprung disease: a meta-analysis. J Pediatr Surg 57:719–725
Karlsen RA, Hoel AT, Fosby MV et al (2022) Comparison of clinical outcomes after total transanal and laparoscopic assisted endorectal pull-through in patients with rectosigmoid Hirschsprung disease. J Pediatr Surg 57:69–74
Saadai P, Trappey AF, Goldstein AM et al (2019) Guidelines for the management of postoperative soiling in children with Hirschsprung disease. Pediatr Surg Int 35:829–834
El-Sawaf M, Siddiqui S, Mahmoud M, Drongowski R, Teitelbaum DH (2013) Probiotic prophylaxis after pullthrough for Hirschsprung disease to reduce incidence of enterocolitis: a prospective, randomized, double-blind, placebo-controlled, multicenter trial. J Pediatr Surg 48:111–117
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
Data acquisition, analysis, and interpretation were performed by both authors. AA (first author) made the drafting of the manuscript. Both authors (AA, AA) have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All methods were carried out in accordance with relevant guidelines and regulations. An informed parental consent was taken before operation in all cases. The study was conducted after internal review board approval (General Surgery Department, Ain-Shams University).
Consent for publication
Not applicable. Patient identity did not appear in any part of the manuscript; therefore, consent for publication was not required.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
AbouZeid, A.A., AbdelMalek, A.A. Outcomes following endorectal pull-through for Hirschsprung disease: a retrospective study. Egypt Pediatric Association Gaz 72, 48 (2024). https://doi.org/10.1186/s43054-024-00286-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43054-024-00286-y