Abstract
Background
Pregnancy is not uncommon in patients with non-cirrhotic portal hypertension. Rupture of a splenic artery aneurysm remains a rare complication, associated with a very poor maternal–fetal prognosis. Our aim is to report a case of ruptured splenic aneurysm and to show the maternal–fetal over-risks during the association of pregnancy and portal hypertension, even in non-cirrhotic patients.
Case presentation
We report a case of a 34-year-old woman, pregnant at 24 weeks gestation, with non-cirrhotic portal hypertension due to hepatic schistosomiasis. She was hospitalized for variceal bleeding. Patient had undergone endoscopic variceal band ligation and no bleeding recurrence. An unexplained hypovolemic shock appeared during the hospitalization with the occurrence of an in utero fetal death. The fetus was delivered by vaginal delivery. Abdominal CT scan angiogram showed a splenic artery aneurysm rupture. The patient underwent an emergency laparotomy with ligation of the splenic artery associated with splenectomy. Postoperative course was simple. Management of portal hypertension was continued at discharge (diuretic, beta-blockers, and esophageal varices ligation).
Conclusion
The association of pregnancy and portal hypertension remains a serious situation with a high risk of maternal–fetal complications. Splenic artery aneurysm rupture is one of the rare complications of this association with a very poor maternal–fetal prognosis. Open repair is the surgical treatment of choice with a non-negligible morbi-mortality.
Similar content being viewed by others
Background
Schistosomiasis is the most common etiology of non-cirrhotic portal hypertension (NCPH) in Africa [1, 2]. Currently, the occurrence of pregnancy in a patient with portal hypertension is increasingly common [3]. Pregnancies during portal hypertension are considered high risk and likely to jeopardize the maternal–fetal prognosis [3, 4]. Pregnancy and portal hypertension are associated with a higher risk of spontaneous miscarriage, in utero fetal death, and prematurity [3,4,5,6,7,8,9,10]. Variceal bleeding is a serious complication [3,4,5,6,7,8,9,10]. However, splenic artery aneurysm (SAA) rupture is a rare complication with a very high maternal–fetal mortality rate [7, 10,11,12]. The exact prevalence of SAA remains unknown to this day [12]. SAA rupture occurs in the majority of cases during the 2nd or 3rd trimester of pregnancy [11, 12]. The management of complications of portal hypertension during pregnancy is complex and poorly codified, and data on the subject remains quite limited [3, 4]. The management of pregnant patients with portal hypertension discovered at the complication stage constitutes a real challenge in Madagascar, due to the absence of a standardized protocol and limited technical platforms. Moreover, data on the association of pregnancy and non-cirrhotic portal hypertension secondary to hepatic schistosomiasis are limited. Moreover, the splenic artery aneurysm rupture remains a rarely reported complication. Our aim is to report a case of ruptured splenic aneurysm and to show the maternal–fetal over-risks during the association of pregnancy and portal hypertension, even in non-cirrhotic patients.
Case presentation
A 34-year-old woman, a schoolteacher, with 24 weeks of pregnancy was admitted to the hospital with moderate hematemesis and 300 ml of blood loss. The patient lives in a region with a high endemicity of Schistosoma mansoni. In her obstetric history, we noted a pregnancy carried to term and a threatened miscarriage at 20 weeks of pregnancy. She did not consume alcohol. Follow-up of the patient prior to hospitalization revealed normal liver function. Ultrasound examination during the first full-term pregnancy revealed no abnormalities suggestive of portal hypertension or hepatic dysmorphia. The patient had reported no previous digestive bleeding episodes (hematemesis and melena). Clinical examination on admission reported a stable hemodynamic state, abundant volume ascites, collateral venous circulation, and significant splenomegaly. Obstetrical examination on admission showed a well audible fetal heart sound. Biological tests reported an anemia of 7.4 g/dL. Hepatitis B-C serology was negative. Schistosomiasis serology was positive. Parasitological examination of the stools revealed schistosome eggs. The results of the other biological tests are reported in Table 1. Abdominal ultrasound showed an enlarged liver, periportal fibrosis, a portal vein diameter of 18 mm, and significant splenomegaly. Obstetrical ultrasound reported a single intrauterine pregnancy with a biometry corresponding to 24 weeks of pregnancy. Upper gastrointestinal endoscopy showed grade III esophageal varices with red signs. We retained the diagnosis of a variceal bleeding in a pregnant woman of 24 weeks of pregnancy with hepato-splenic schistosomiasis. The patient had undergone a session of endoscopic variceal band ligation with placement of 4 elastics. She was put on carvedilol at an initial dose of 6.25 mg/day.
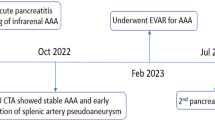
The evolution was marked on the fourth day at hospital (day 4) by a sudden appearance of an unexplained shock (blood pressure 70/40 mmHg, heart rate 125 beats/minute, respiratory rate 24 cycles/minute, oxygen saturation 92%) associated with sudden abdominal pain. Hypovolemic shock was stable under fluid resuscitation associated with vasopressors, but persistent, with the occurrence of an in utero fetal death on the sixth day at hospital (day 6). Delivery was induced. The fetus was delivered by vaginal delivery. On the seventh day of hospitalization, the patient had been transferred to a referral University Hospital in the capital to undergo a CT scan with angiography and receive better care. Chest and abdominal CT scan angiogram were ordered in view of the persistence of a shock on the eighth day at hospital (day 8) and showed a pseudo-aneurysmal dilatation of the splenic artery with multiple fluid collections (around the aneurysm, under the capsular of the superior pole of the spleen and peri-stomachic, in front of the hepatic caudate lobe) suggesting a high probability of a splenic artery aneurysm rupture (Fig. 1). The patient underwent an emergency laparotomy immediately after CT scan with ligation of the splenic artery associated with splenectomy. The postoperative course was simple. The patient was put on spironolactone 75 mg/day and carvedilol 12.5 mg/day at discharge. Endoscopic variceal band ligation sessions were scheduled every month.
Discussion and conclusion
The occurrence of pregnancy in a patient with portal hypertension remains to this day an unusual situation for clinicians [3, 4]. This association should be considered as a high-risk pregnancy because it may jeopardize the maternal–fetal prognosis [3,4,5,6,7,8,9,10]. The exact incidence of portal hypertension in pregnancy remains unknown in Madagascar. In India, in-hospital prevalence of NCPH and pregnancy was 0.09% [11]. The majority of pregnancies in patients with portal hypertension were reported in developed countries and were secondary to cirrhosis [5, 8]. However, in developing countries, this was due to non-cirrhotic causes [5], such as that observed in our patient where NCPH was due to hepatic schistosomiasis. Epidemiological data on the association between pregnancy and hepato-splenic schistosomiasis are very limited. In our literature review, we found only one case reported by Kopelman et al. (USA, 1990) [13].
In our observation, variceal bleeding was the revealing symptom of portal hypertension during pregnancy. This finding had been reported by several authors [3, 4, 6, 8, 9]. Variceal bleeding is reported in 18–32%, and up to 50% in case of known portal hypertension, especially during the second and third trimester of pregnancy when the increase in portal hypertension is significant due to the maximum increase in plasma volume and mechanical compression of the inferior vena cava by the pregnant uterus [3,4,5,6,7,8,9,10]. In addition, variceal bleeding during pregnancy is associated with a higher incidence of abortion (29.4%) and perinatal death (33.3%).
However, other serious complications have been reported, in particular the splenic artery aneurysm (SAA) rupture, burdening the maternal prognosis in the short term, with a maternal mortality rate of 70–75% and fetal mortality of 90–95% [7, 10,11,12, 14]. The exact prevalence of SAA remains unknown. Data in the general population are also variable, ranging from 0.1 to 0.2% in a large autopsy series [12]. SAA have been reported to be associated with several etiological factors, including portal hypertension associated with splenomegaly [12, 14, 15]. Two thirds of these aneurysms rupture during the 2nd and 3rd trimester of pregnancy [14]. The frequency of SAA rupture increases during pregnancy and in case of associated portal hypertension [12]. Recent data reported aneurysm rupture rates closer to 2–3% [16, 17]. Given the high maternal–fetal mortality rate associated with SAA rupture, clinicians should consider it in pregnant women with an acute abdomen, unexplained shock, and sudden maternal collapse [6]. Surgical treatment with aneurysmectomy or splenic artery ligation with or without splenectomy remains one of the gold standard treatment options [12, 14, 15], especially in low-income countries such as Madagascar. The SAA rupture was suspected in our patient in front of a persistent and unexplained shock, requiring an emergency laparotomy with ligation of the splenic artery associated with splenectomy with a favorable outcome.
In view of the multiple maternal–fetal complications, the management of portal hypertension in pregnant women must be multidisciplinary, involving various entities (hepato-gastroenterologists, obstetricians, pediatricians, surgeons, anesthesiologists) [3,4,5,6,7,8,9,10], as in our case. In several studies, the maternal–fetal prognosis of pregnancies with known portal hypertension receiving primary prophylaxis for variceal bleeding before conception was significantly better than that of pregnancies in which portal hypertension was discovered [3,4,5,6,7,8,9,10]. Therefore, portal hypertension should be routinely investigated before conception in high-risk pregnant women. In women with portal hypertension, pregnancy should be planned and portal hypertension managed before conception to decrease maternal–fetal morbidity.
In conclusion, the association of pregnancy and portal hypertension remains an unusual situation for clinicians. It is serious with a high risk of maternal–fetal complications. The splenic artery aneurysm rupture is a rare complication, but it is a major risk for the maternal–fetal prognosis in the short term. This complication should be highly sought after by clinicians in pregnant women with sudden maternal collapse with or without abdominal pain. The management of portal hypertension and pregnancy should be multidisciplinary, including obstetricians, hepato-gastroenterologists, pediatricians, surgeons, and anesthesiologists. Primary prevention of portal hypertension in pregnancy improves maternal–fetal prognosis.
Availability of data and materials
Not applicable.
References
Tamarozzi F, Fittipaldo VA, Orth HM, Richter J, Buonfrate D, Riccardi N et al (2021) Diagnosis and clinical management of hepatosplenic schistosomiasis: a scoping review of the literature. PLoS Negl Trop Dis 15(3):e0009191
Masi B, Perles-Barbacaru TA, Bernard M, Viola A (2020) Clinical and preclinical imaging of hepatosplenic schistosomiasis. Trends Parasitol 36(2):206–226
Beringer J, Nahon P, Carbillon L, Ganne-Carrié N, Nault JC (2018) Grossesse et hypertension portale Hépato Gastro 25:426–435
d’Alteroche L, Perarnau JM, Perrotin F, Bacq Y (2008) Portal hypertension and pregnancy. Gastroenterol Clin Biol 32:541–546
Pol MM, Chawla LU, Rathore YS, Goel R (2017) Combined caesarean with splenectomy in pregnancy with portal hypertension: defining plausibility. BMJ Case Rep. https://doi.org/10.1136/bcr-2017-220561
Keepanasseril A, Gupta A, Ramesh D, Kothandaraman K, Jeganathan YS, Maurya DK (2020) Maternal-fetal outcome in pregnancies complicated with non-cirrhotic portal hypertension: experience from a tertiary Centre in South India. Hepatol Int. 14:842–49
Gala AR, Surapaneni T, Aziz N, Kallur SD (2018) A review of outcomes in pregnant women with portal hypertension. J Obstet Gynaecol India 68(6):447–451
Aggarwal N, Sawhney H, Vasishta K, Dhiman RK, Chawla Y (2001) Non-cirrhotic portal hypertension in pregnancy. Int J Gynecol Obstet 72(1):1–7
Sumana G, Dadhwal V, Deka D, Mittal S (2008) Non-cirrhotic portal hypertension and pregnancy outcome. J Obstet Gynaecol Res 34(5):801–804
Aggarwal N, Negi N, Aggarwal A, Bodh V, Dhiman RK (2014) Pregnancy with portal hypertension. J Clin Exp Hepatol 4(2):163–171
Crocker A, Girling J, Cotzias C (2011) Massive bleeding in pregnancy from ruptured oesophageal varices complicating portal hypertension: a cautionary tale. Obstet Med 4(4):169–170
Sadat U, Dar O, Walsh S, Varty K (2008) Splenic artery aneurysms in pregnancy – a systematic review. Int J Surg 6(3):261–265
Kopelman J, Miyazawa K (1990) Hepatosplenic schistosomiasis in pregnancy: report of a case and review of the literature. Am J Perinatol 7(04):380–383
Arepally A, Dagli M, Hofmann LV, Kim HS, Cooper M, Klein A (2002) Treatment of splenic artery aneurysm with use of stent-graft. J Vasc Interv Radiol 13(6):631–633
Ha JF, Sieunarine K (2009) Laparoscopic splenic artery aneurysm resection: review of current trends in management. Surg Laparosc Endosc Percutan Tech 19(2):e67-70
Trastek VF, Pairolero PC, Joyce JW, Hollier LH, Bernatz PE (1982) Splenic artery aneurysms. Surgery 91(6):694–699
Stanley JC, Fry WJ (1974) Pathogenesis and clinical significance of splenic artery aneurysms. Surgery 76:898–909
Acknowledgements
We would like to thank the team at the University Hospital Andrainjato, Fianarantsoa, Madagascar, led by professor Soloniaina Hélio Razafimahefa for this case report.
Funding
This research was not supported by any specific grant from public, commercial, or nonprofit funding agencies.
Author information
Authors and Affiliations
Contributions
CIR, AFR, and BMR were responsible for the data collection, writing, literature reviews, and editing the manuscript and made substantial contributions to the design of the case report. SHR participated in the conception and design of the case report and article preparation and critically revised the article for intellectual content. HR, NHR, ASR, ALRR, THR, and RMR critically revised the article for intellectual content. All authors read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patient for the publication of her data discussed in this case report.
Competing interests
The authors declare that they have no competing interests regarding the publication of this case report.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Razafindrazoto, C.I., Randrianiaina, A.F., Ralaizanaka, B.M. et al. Splenic artery aneurysm rupture in a pregnant woman with hepatosplenic schistosomiasis: case report and literature review. Egypt Liver Journal 14, 9 (2024). https://doi.org/10.1186/s43066-024-00314-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43066-024-00314-x