Abstract
Background
Non-alcoholic fatty liver disease (NAFLD) is a liver pathology. NAFLD’s prevalence is increasing in the world and because of the increase non-invasive methods are gaining importance in diagnosis. The Fibrosis 4 (FIB-4) score is one of the most commonly used non-invasive scoring methods for diagnosing NAFLD today. Acute pancreatitis is a disease with inflammation and high morbidity. There are studies indicating that acute pancreatitis progresses more severely in patients with NAFLD. In our study, it was aimed to define the possible relationship between the FIB-4 score and the severity of acute pancreatitis, which has not been investigated before and contribute to the literature.
Methods
Our study was conducted by retrospectively scanning 124 patients diagnosed with acute pancreatitis between 2018 and 2020. The patients were compared with the presence of NAFLD and the FIB-4 score results in those with NAFLD.
Results
The 48th-hour Ranson score was found to be statistically significantly higher in patients with NAFLD compared to those without NAFLD. In patients with NAFLD, the total billurbin, direct billurbin, AST, ALT, ALP, GGT, and Ranson scores were found to be statistically significantly higher in those with FIB-4 score ≥ 2.67.
Conclusıon
As liver fibrosis increases in patients with NAFLD, it is suggested that liver damage accompanying acute pancreatitis increases, and the prognosis of acute pancreatitis worsens. There is a need for further studies to be conducted while centering more on this subject, which has not been investigated before in the literature.
Similar content being viewed by others
Introduction
Acute pancreatitis is an inflammatory disease of the pancreatic gland and multiple causes play a role in its etiology [1]. Although biliary stones and alcohol use are among the most common causes for this disease, there are publications stating that a more severe clinical course is observed in patients with non-alcoholic fatty liver disease (NAFLD) [2, 3]. NAFLD is a disease in which more than 5% of the weight of the liver is made up of fat, and it is diagnosed by exclusion of causes such as alcohol, drugs, and genetics [4]. It affects 25% of the world, and its frequency is expected to increase gradually in the coming years [5]. Fibrosis-4 (FIB-4) score is one of the scoring systems produced in recent years to predict the presence of fibrosis in the liver by non-invasive methods. Studies investigating the relationship between NAFLD and FIB-4 have reported that the FIB-4 score is more strongly associated with fibrosis than other scores, and it is more successful in identifying patients with higher risk for liver-related comorbidities [6]. If the FIB-4 score is above 2.67 in NAFLD patients, it is considered risky, and further examination is recommended.
The aim of our study is to compare the results of scoring systems in NAFLD patients and to examine the differences in results between NAFLD patients, and those without NAFLD, to evaluate the usability of the FIB-4 score in NAFLD patients, to predict the severity of acute pancreatitis, and to shed light on further research that can be done on this subject, which has not been studied before in the literature.
Materials and methods
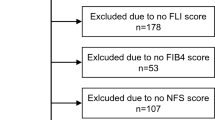
Our study was conducted by retrospectively scanning 124 patients who applied to hospital between 2018 and 2020 and were diagnosed with AP. All patients included in the study examined and recorded by gender, age, presence of NAFLD, length of stay, amylase, lipase, leukocyte count, glomerular filtration value, INR, total billurbin, direct billurbin, aspartate aminotransferase (AST), alanine aminotransferase (ALT), gamma-glutamyl transferase (GGT), alkaline phosphatase (ALP), c-reactive protein (CRP), FIB-4, Acute Physiology and Chronic Health Evaluation II (APACHE 2) score, BALTAZAR score, BISAP score, and RANSON score from 0 to 48 h.
The diagnosis of AP was made by the presence of at least 2 of 3 criteria: These criterias are typical abdominal pain, amylase and lipase levels 3 times higher than the upper limit, and inflammation demonstrated by abdominal imaging (computerized tomography). The diagnosis of NAFLD was made by abdominal imaging (computerized tomography or ultrasonography). Ten patients were diagnosed by ultrasonography, and 114 patients were diagnosed by computerized tomography. There was no known liver disease other than NAFLD in the study population. Therefore, liver biopsy was not considered.
Criterıa for exclusion to the study
For this study, those younger than 18 years of age, people who developed pancreatitis after ERCP, people who use alcohol (140 g/week for men, 70 g/week for women), those with viral hepatitis, hypertriglyceridemia, drug-induced hepatitis, autoimmune liver disease, and other liver disease are not included in this study. Also, people with insufficient clinical data are not included.
NAFLD diagnostıc criteria
Ultrasonography and computerized tomography were used for the diagnosis of NAFLD. A diagnosis of NAFLD was made with an increase in liver echogenicity and a distinct brightening compared to the kidney parenchyma on ultrasonography. A diagnosis of NAFLD was made because the attenuation value in the liver parenchyma was significantly lower than the spleen parenchyma in computerized tomography.
Statistical analysis
Data were evaluated using the SPSS 23.0 (Statistical Program for Social Sciences) statistical program.
Descriptive statistics (number, percentage, mean ± standard deviation, median (minimum–maximum) were used for this research. Mann–Whitney U test was used for univariate continuous data, and chi-square test was used for categorical data. Type 1 error values of p < 0.05 were considered significant in all statistical analyses.
Results
Demographic data of the patients included in the evaluation are presented in Table 1. NAFLD was detected in 43 patients (34%), and 56% of the total patients were women. Female patients were not using oral contraceptives.
When the patients were compared according to the presence of NAFLD, no significant difference was found in other data, except for the 48th-hour Ranson score, as seen in Table 2. The 48th-hour Ranson score was found to be statistically significantly higher in patients with NAFLD compared to the other group.
When the patients with NAFLD were compared to each other, according to the FIB-4 scoring values, the total billurbin, direct billurbin, AST, ALT, ALP, GGT, and Ranson scores of the patients with FIB-4 ≥ 2.67 were found to be statistically significantly higher than the other group, as indicated in Table 3.
Discussion
Acute pancreatitis is a disease that occurs as a result of inflammation of the pancreas due to causes such as gallstones, alcohol use, and hyperlipidemia. Although it usually has a good prognosis, it can cause serious morbidity and mortality when complications develop. For this reason, early diagnosis of complications that may develop in the course of acute pancreatitis and taking precautions against these complications gain importance. There are many scoring systems produced to estimate the severity and mortality rate of acute pancreatitis, but there is no scoring system that provides precise information about the prognosis [7]. In a study comparing scoring systems, similar results were found between BISAP, Ranson, APACHE 2, and Balthazar scores, and it was reported that the scores were not superior to each other [8].
NAFLD is a liver disease that occurs as a result of excessive accumulation of fat in the liver independent of alcohol use, and it is estimated to be present in 25% of the population [9]. Fibrosis, which occurs as a result of fatty liver, may lead to cirrhosis and hepatocellular cancer in the following years. Early diagnosis of fibrosis is important for clinicians to avoid frightening complications. The gold standard diagnostic method for diagnosing fibrosis is liver biopsy, but since this procedure is invasive and cannot be performed everywhere, studies on non-invasive diagnostic methods have started. The FIB-4 score is the most widely used non-invasive diagnostic method today. It is stated that the FIB-4 score is more successful than other scores because it has a higher diagnostic rate and can predict more successfully for risky patients [6]. It is stated that a FIB-4 score higher than 2.67 in NAFLD patients is a harbinger of fibrosis formation [10].
In studies on the relationship between NAFLD and acute pancreatitis, it is stated that acute pancreatitis progresses more severely in patients with NAFLD, and NAFLD may be a risk factor for acute pancreatitis [11, 12]. No study was found in the literature in which the prognosis of acute pancreatitis could be predicted using the FIB-4 score in NAFLD patients. In our study, it was aimed to investigate the effect of NAFLD on acute pancreatitis prognosis, also to investigate the possible relationship between FIB-4 score and acute pancreatitis in NAFLD patients and to reveal the data of Turkey for the relationship between FIB-4 score for NAFLD.
When patients with NAFLD were compared with patients without NAFLD, the 48th-hour Ranson score was found to be statistically significantly higher, consistent with studies in the literature [12].
Among NAFLD patients, total billurbin, direct billurbin, AST, ALT, ALP, GGT, and Ranson scores were found to be statistically significantly higher in patients with FIB-4 score ≥ 2.67. Even if it is not reflected in the statistics, it is striking that the amylase and lipase values and the APACHE 2 scores are also high. The results suggest that as liver fibrosis increases, liver damage accompanying acute pancreatitis increases, and the prognosis of acute pancreatitis worsens. There is a need for further studies to be conducted in centers more on this subject, which has not been investigated before in the literature.
The limitations of our study are the following: it is retrospective, performed in a single center, liver biopsy is not used in the diagnosis, diabetes mellitus status and body mass index is not recorded.
Conclusion
In our study, it was found that as the FIB-4 score increased in patients with NAFLD, acute pancreatitis progressed more severely and increased cholestatic damage in the liver. In order to use the FIB-4 score to determine the prognosis of acute pancreatitis, research with a larger patient population is required. It is considered that the FIB-4 score may play a role in predicting morbidity and mortality in patients with acute pancreatitis in the coming years.
References
Stimac D, Mikolasevic I, Krznaric-Zrnic I, Radic M, and Milic S (2013) Epidemiology of acute pancreatitis in the North Adriatic region of Croatia during the last ten years. Gastroenterol Res Pract 2013. https://doi.org/10.1155/2013/956149
Xu C et al (2015) Influence of fatty liver on the severity and clinical outcome in acute pancreatitis. PLoS One 10(11):e0142278. https://doi.org/10.1371/JOURNAL.PONE.0142278
Yoon SB et al (2017) Impact of fatty liver on acute pancreatitis severity. Gastroenterol Res Pract 2017. https://doi.org/10.1155/2017/4532320
Brunt EM, Tiniakos DG (2010) Histopathology of nonalcoholic fatty liver disease. World J Gastroenterol: WJG 16(42):5286. https://doi.org/10.3748/WJG.V16.I42.5286
Younossi ZM et al (2020) Epidemiology of chronic liver diseases in the USA in the past three decades. Gut 69(3):564–568. https://doi.org/10.1136/GUTJNL-2019-318813
Angulo P et al (2013) Simple noninvasive systems predict long-term outcomes of patients with nonalcoholic fatty liver disease. Gastroenterology 145(4). https://doi.org/10.1053/J.GASTRO.2013.06.057
Chatila AT, Bilal M, Guturu P (2019) Evaluation and management of acute pancreatitis. World J Clin Cases 7(9):1006. https://doi.org/10.12998/WJCC.V7.I9.1006
Papachristou GI et al (2010) Comparison of BISAP, Ranson’s, APACHE-II, and CTSI scores in predicting organ failure, complications, and mortality in acute pancreatitis. Am J Gastroenterol 105(2):435–441. https://doi.org/10.1038/AJG.2009.622
Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M (2016) Global epidemiology of nonalcoholic fatty liver disease-meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology 64(1):73–84. https://doi.org/10.1002/HEP.28431
McPherson S et al (2017) Age as a confounding factor for the accurate non-ınvasive diagnosis of advanced NAFLD fibrosis. Am J Gastroenterol 112(5):740–751. https://doi.org/10.1038/AJG.2016.453
Mikolasevic I et al (2017) Nonalcoholic fatty liver and the severity of acute pancreatitis. Eur J Intern Med 38:73–78. https://doi.org/10.1016/J.EJIM.2016.10.019
Wu D et al (2019) Nonalcoholic fatty liver disease aggravated the severity of acute pancreatitis in patients. Biomed Res Int 2019. https://doi.org/10.1155/2019/9583790
Acknowledgements
We would like to thank Kıvanc Kirdok, a 3rd-year medical student at Celal Bayar University Hospital, for help during data collection.
Author information
Authors and Affiliations
Contributions
K.K., O.Y., T.B., and E.K. conceived and designed the study. K.K. and O.Y. collected the data. K.K., O.Y., and E.K. analyzed the data and interpreted the results. K.K. and E.K. drafted the manuscript. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Medical Faculty Clinical Research Ethics Committee approved this study (Approval no: 20.478.486/643). The study was conducted according to the World Medical Association Declaration of Helsinki.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kirdok, K., Yogurtcu, Ö., Buran, T. et al. Can the FIB-4 score predict the severity of acute pancreatitis in NAFLD?. Egypt Liver Journal 14, 8 (2024). https://doi.org/10.1186/s43066-024-00313-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43066-024-00313-y