Abstract
Introduction
Endoscopic variceal ligation (EVL) is a crucial procedure for the primary and secondary prevention of variceal bleeding. The objective of this study was to evaluate the efficacy and tolerability of EVL in the prevention of variceal bleeding.
Methods
This was a retrospective, single-center study over 8 years, from January 2013 to December 2020, including all patients who came for EVL in primary or secondary prevention.
Results
Fifty-seven patients (male/female: 39/18) were included. The mean age of the patients was 40.02 ± 12.32 years (range: 19–68). Portal hypertension was secondary to cirrhosis in 13 patients (22.8%) and to a non-cirrhotic cause in 44 patients (77.2%). EVL was indicated for primary and secondary prevention in 5.3% and 94.7%, respectively. All patients had received propranolol with a mean daily dose of 108.07 ± 38.52 mg (extremes: 80–160). Eradication of varices was achieved in 33 patients (57.9%) with an average of 3.06 ± 0.70 sessions (extremes: 1–5) and an average duration of 10.12 ± 6.21 months (extremes: 1–24). Ten patients (17.5%) had variceal bleeding, and one patient (1.8%) died. There was no significant difference between patients with cirrhotic and non-cirrhotic portal hypertension in terms of varices eradication, variceal bleeding, and mortality. Gender (HR: 37.18; CI: 0.14–18.4; p = 0.009) and the number of previous bleeds (HR: 1.34; CI: 1.01–1.80; p = 0.041) were independent predictors of variceal bleeding during EVL. Dysphagia (73.7%) and retrosternal pain (78.9%) were the main adverse events after ligation.
Conclusion
EVL is an efficient technique to eradicate varices. Its tolerance is good with post-ligation signs that are rapidly regressive.
Similar content being viewed by others
Introduction
Esophageal variceal bleeding is a major cause of morbidity and mortality in patients with cirrhotic and non-cirrhotic portal hypertension (PH) in developing countries [1, 2]. Endoscopic variceal ligation (EVL) is a crucial treatment for acute variceal bleeding [3]. The use of nonselective beta-blockers (NSBBs) or EVL is recommended for primary prevention of variceal bleeding in patients with large and medium esophageal varices [4, 5]. The combination of EVL and NSBBs (propranolol or nadolol, with carvedilol as an alternative) is a standard approach to rebleeding prevention [6]. EVL also plays an important role in the primary and secondary prevention of variceal bleeding [6]. In developed countries, this technique has been commonly used since the 1980s and reported in various guidelines [1, 6]. Some sub-Saharan data and a previous Malagasy study had found convincing results on the eradication of varices [1, 7, 8]. Few patients could benefit from this endoscopic technique because of its high cost. The aim of this study was to evaluate the efficacy and safety of EVL in Malagasy patients who had benefited from this procedure in primary and secondary prevention.
Patients and methods
Study design and participants
This was a retrospective and single-center study conducted in Gastroenterology Unit, University Hospital Joseph Raseta Befelatanana, Antananarivo, Madagascar, from January 2015 to December 2018. We included all patients treated EVL in primary or secondary prevention. Patients who had stopped after a single session of EVL without endoscopic control were excluded. The parameters studied were as follows: gender, age, comorbidities, previous bleeding, jaundice, ascites, splenomegaly, grade of varices, red signs, Child–Pugh class, propranolol dose, number of sessions, interval between sessions, follow-up time, varices eradication, bleeding rate during the procedure, mortality, and adverse events.
Endpoints
The primary endpoints were varices eradication rate, variceal bleeding rate, and mortality during the protocol. Safety was judged on the occurrence of immediate post-ligation adverse events.
Definitions
A diagnosis of cirrhosis was based on the results of noninvasive liver examination (clinical, biological, hepatobiliary ultrasound, and degree of fibrosis). Alcoholic etiology of cirrhosis was retained on the basis of an alcohol consumption of more than 20 g/day in women and 40 g/day in men for at least 10 years and without any other etiologies found. Viral and autoimmune etiology of cirrhosis was retained in view of the positivity of viral markers and anti-tissue autoantibodies.
Hepatosplenic schistosomiasis diagnostic criteria were as follows: the presence of splenomegaly, the presence of periportal fibrosis, the presence of radiological and/or endoscopic evidence of PH, and positive schistosomiasis serology.
The diagnosis of portal thrombosis was made by hepatic doppler ultrasound and/or abdominal CT scan.
Variceal bleeding was retained by the association of several criteria: evidence of PH and the presence of esophageal varices with red signs or recent bleeding (hematemesis and/or melena).
Eradication of varices was defined by the disappearance of esophageal varices or the existence of grade 1 fibrous varices.
Description of EVL and management of variceal bleeding
EVL consisted of the placement of rubber rings on variceal columns, which are sucked into a plastic hollow cylinder attached to the tip of the endoscope by an experienced senior endoscopist. Ligation was started at the lower end of the esophagus and proceeded upwards in a spiral fashion. The average number of rubber bands was five (extremes 2–5). Olympus® Q160 video endoscope and a rechargeable multiband system (Euroligator) were used. EVL sessions were performed under general anesthesia with propofol administered intravenously in a patient fasting for at least 6 h. Induction dose was 2.5 to 3 mg/kg. The maintenance dose was done by a bolus of propofol of 25, 50, or 100 mg, intermittently as judged by the anesthesiologist, depending on the clinical (hemodynamic parameters) and sedation level of the patient. After the ligation, the patients were kept in hospital for 24-h monitoring and systematically put on nefopam infusion and paracetamol every 8 h associated with a proton-pump inhibitor.
Patients with variceal hemorrhage between EVL sessions were hospitalized and supportively cared according to a standardized protocol of the gastroenterology unit. Propranolol was continued in all patients during hospitalization, maintaining the dose before bleeding. EVL was continued at discharge in all patients until eradication of esophageal varices.
Statistical analysis
Statistical analyses were performed using SPSS (Inc., Chicago, IL, USA version 25). Quantitative variables were expressed as mean and standard deviation (SD), while qualitative variables were expressed as frequency and percentage. The chi-square (χ2) test or Fisher’s exact test, when appropriate, was used for the comparison of for qualitative variables between cirrhotic PH and non-cirrhotic PH. Continuous variables in both groups were compared using the paired t-test. In case of a skewed distribution, the Mann-Whitney U-test was used for the comparison of continuous variables. The cumulative probability of patients who experienced bleeding was assessed by Kaplan-Meier curves. Multivariate Cox proportional hazard models were used to detect independent predictors of variceal bleeding. All p-values were two-sided, with values < 0.05 considered statistically significant.
Results
Clinical and endoscopic characteristics of our patients
Fifty-seven patients were included in this study. Portal hypertension was secondary to cirrhosis in 13 patients (22.8%) and a non-cirrhotic cause in 44 patients (77.2%). Thirty-nine patients (68.4%) were male. The overall mean age of the patients was 40.02 ± 12.32 years, with extremes from 19 to 68 years. The mean age was significantly lower in patients with non-cirrhotic PH compared with those with cirrhosis (30 vs 50.23, p < 0.001). Alcohol (38.46%) and hepatitis B virus (30.77%) were the main etiologies of cirrhosis. Hepatic schistosomiasis (90.91%) and portal thrombosis (9.09%) were the causes of non-cirrhotic PH. Grade III varices occupied the 96.49% of patients (n = 55), and 38.6% (n = 22) had red signs. For patients with cirrhosis, the mean Child–Pugh score was 8.38 ± 2.29. All patients were on beta-blocker (propranolol) before EVL (mean dose: 108.07 ± 38.52 mg/day) including 37 patients (64.91%) on 80 mg/day and 20 (35.09%) on 160 mg/day. EVL was indicated for primary prevention in 5.3% of patients and secondary prevention in 94.7% of cases. The overall mean number of EVL sessions was 2.40 ± 1.03 (range 1–5). The mean interval between EVL sessions and the mean duration of follow-up were 1.30 ± 0.46 months (range 1–2) and 6.28 ± 6.54 months (range 1–24), respectively. There was no significant difference between the characteristics of cirrhotic and non-cirrhotic patients, except for age, the presence of jaundice and splenomegaly, and daily dose of propranolol. The clinical and endoscopic characteristics of the patients are shown in Table 1.
Efficacy and safety of EVL
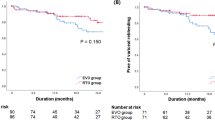
Eradication of esophageal varices was achieved in 33 patients (57.9%). The average number of sessions and the average duration to achieve eradication were 3.06 ± 0.70 sessions (extremes: 1–5) and 10.12 ± 6.21 months (extremes: 1–24), respectively. Ten patients (17.5%) had variceal bleeding during the follow-up period, and one patient (1.8%) died. There was no significant difference between cirrhotic and non-cirrhotic patients in terms of eradication rate, variceal bleeding rate, and mortality (Table 2). The number of EVL sessions was significantly higher in patients with variceal bleeding compared with those without bleeding (3.30 ± 0.82 vs 2.21 ± 0.98; p = 0.002). The probability of variceal bleeding was determined using Kaplan-Meier survival curves (Fig. 1). Male gender (HR: 37.18; CI: 0.14–18.4; p = 0.009) and number of previous bleeds (HR: 1.34; CI: 1.01–1.80; p = 0.041) were independent predictors of variceal bleeding during EVL (Table 3). Dysphagia (73.7%) and retrosternal pain (78.9%) were the main adverse events after ligation that resolved very quickly.
Discussion
Esophageal variceal bleeding is one of the most important causes of morbidity and mortality in patients with parenchymal liver disease and portal hypertension. Endoscopic treatment is one of the recommended therapeutic armamentariums for primary prevention of variceal bleeding in patients at high risk of bleeding and has become the gold standard for the management of bleeding esophageal varices. Once the initial bleeding episode is controlled by endoscopic treatment, there is a significant risk of rebleeding. Patients who survive the bleeding episode require repeated endoscopic treatments until the varices are obliterated to prevent recurrence [4,5,6, 9].
We conducted a retrospective study evaluating the efficacy of EVL in patients with cirrhotic or non-cirrhotic PH in primary and secondary prevention followed in Endoscopy Unit, University Hospital Joseph Raseta Befelatanana, Antananarivo, Madagascar. This study remains fundamental because it allowed us to determine the eradication rate, the number of sessions for varices eradication, and the rate of variceal bleeding in our center. Nevertheless, this study had several limitations. The retrospective, monocentric nature, and the relatively small size of our sample constituted these main limitations.
The study population consisted mainly of 90.91% non-cirrhotic PH patients. Madagascar is known to be an endemic area for Schistosoma mansoni bilharzia, which explains the high prevalence of PH secondary to schistosomiasis [1, 2, 10]. Our results are consistent with some African literature where schistosomiasis was the primary cause of PH [11, 12]. Age has been considered an important risk factor for varicose rebleeding [9]. In the present study, the overall mean age was 40.02 years. This mean age was significantly higher in the cirrhotic PH group compared to those in the non-cirrhotic PH group.
In our series, secondary prevention of variceal bleeding occupied the totality of the indication for EVL (94.7%). This finding can be explained by two reasons. The first reason was that the technical platform did not allow us to perform EVL in the context of acute variceal hemorrhage, unlike in other African countries [3, 7, 8, 13]. The second reason was that patients came to hospital in the majority of cases only after an episode of hemorrhage, and the diagnosis of PH is often made at this time.
Several studies had shown that EVL is effective and safe, requires few sessions to eradicate varicose veins, and significantly reduces the rate of recurrent bleeding. Varices eradication in this study was achieved in 57.9% of patients with an average of 3.06 endoscopy sessions. There was no significant difference in patients with cirrhotic and non-cirrhotic PH. Our eradication rate was similar to those reported in the sub-Saharan literature (50% in Senegal and 62.5% in Mali) [7, 8]. However, this eradication rate remains largely inferior to those of the Maghrebian and Western literature where eradication varies from 79 to 100 [3, 9, 13,14,15]. This difference can be explained by our technical platform. In our study and the other sub-Saharan African studies, the reusable ligation kit was used, allowing only a maximum of 5 elastics to be dropped, whereas in Western countries, they use precise and efficient kits (Multiple Band Ligator) allowing a maximum of 8 elastics to be dropped. In addition, the average number of elastic bands recommended is 5 to 8 bands per session, whereas it is 2 to 5 per session in our study [1, 16]. In our series, patients required an average of 3 endoscopy sessions with an interval of 4 to 8 weeks to achieve eradication of varicose veins. Several authors had reported the same result. Khattak et al. had observed that the majority of these patients obtained complete eradication after 3 sessions of ligation [17]. Lahbabi et al. had reported obliteration of varices in 89.6% of patients with 3 ± 1.99 sessions of ligation [3]. Lo et al. required an average of 3.3 sessions at 3–4-week intervals to achieve varices obliteration [18]. Patch et al. required a median of 2 sessions using 2-week intervals, while Sarin et al. required an average of 3.2 sessions with 1-week intervals [19, 20]. There are varying views regarding the timing of EVL sessions. We have followed a flexible 4- to 8-week interval for our EVL sessions, whereas some prefer a weekly or biweekly schedule and others a bimonthly schedule [21, 22].
In our study, 10 patients (17.5) had experienced variceal bleeding. The rate of bleeding was higher in patients with cirrhosis (30.8%) compared with patients with noncirrhotic PH (13.6%) but without a statically significant difference. The two population groups are probably not similar in terms of severity of portal hypertension because the mean number of previous bleeding episodes was higher in the cirrhosis group than in the noncirrhotic PH group (3.23 ± 2.00 vs. 2.77 ± 2.71). A Chinese study had reported a bleeding rate of 15%, similar to our study [23]. Nevertheless, the rate of variceal bleeding is variable in the literature, ranging from 5 to 29% [7, 8, 13, 21, 23,24,25,26,27,28]. Guo et al. had found that variceal rebleeding was significantly higher in patients who received endoscopic sessions > 3 times compared with those who received sessions ≤ 3 times (61.5% vs 17.5%, p < 0.001) [29]. This finding was verified in our patients where the number of EVL sessions was significantly higher in patients with variceal bleeding compared with those without bleeding (3.30 ± 0.82 vs 2.21 ± 0.98; p = 0.002). In our series, male gender (HR: 37.18; CI: 0.14–18.4; p = 0.009) and number of previous bleeding (HR: 1.34; CI: 1.01–1.80; p = 0.041) were independent predictors of variceal bleeding during EVL. We found that the predictive factors were different in each of the studies [29,30,31]. The population was different in each study explaining this finding. EVL is an effective treatment option for the prevention of recurrent variceal bleeding. However, the efficacy of elastic ligation is significantly increased by the addition of β-blocker therapy [5, 6]. Other treatment modalities such as splenectomy/EVL or EVL/sclerotherapy could also be considered in selected clinical scenarios [2, 9].
As in our study, other authors had also reported the adverse effects after ligation, such as dysphagia and retrosternal pain [1, 7, 8, 23].
Conclusion
This study demonstrates the feasibility and efficacy of EVL to eradicate esophageal varices and reduce variceal rebleeding. Its tolerance is good even if there are post-ligature signs which are rapidly regressive. The improvement of the technical platforms remains at least necessary to improve our results.
Availability of data and materials
Data supporting the conclusions of this study are available from the corresponding author on reasonable request.
References
Rabenjanahary TH, Rakotozafindrabe ALR, Rasolonjatovo AS et al (2019) Ligature des varices œsophagiennes: étude préliminaire à l’unité d’endoscopie digestive de l’hôpital Befelatanana. Med Afr Noire 66(4):187–192
Randriamalala JA, Razafindrazoto CI, Randriamifidy NH et al (2022) Splenectomy combined with endoscopic variceal ligation (EVL) versus EVL alone for secondary prophylaxis of variceal bleeding in hepatosplenic schistosomiasis: a retrospective case-control. Hepat Med 14:79–85
Lahbabi M, Mellouki I, Aqodad N et al (2013) Esophageal vareal ligation in the secondary prevention of variceal bleeding: result of long-term follow-up. Pan Afr Med J 15:3
Dwinata M, Putera DD, Adda’I MF, Hidayat PN, Hasan I (2019) Carvedilol versus endoscopic variceal igation for primary and secondary prevention of variceal bleeding: systematic review and meta-analysis. World J Hepatol 11(5):464–76
Garcia-Tsao G, Abraldes JG, Berzigotti A, Bosch J (2017) Portal hypertension bleeding in cirrhosis: risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the Study of Liver Diseases. Hepatology 65:310–335
de Franchis R, Bosch J, Garcia-Tsao G, Reiberger T, Ripoll C, on Behalf of the Baveno VII Faculty (2022) Baveno VII – renewing consensus in portal hypertension. J Hepatol 76(4):959–974
Bassène ML, Diouf ML, Dia D, Mbengue M, Amdil H, Le Moine O (2010) la ligature de varices oesphagiennes dans le centre d’endoscopie digestive du CHU Aristide-le-Dantec de dakar: étude préliminaire de 60 cas. J Afr Hepatol Gastroenterol 4:194–198
Diarra M, Konaté A, Souckho A et al (2015) La ligature dans la prévention des récidives hémorragiques par rupture des varices œsophagiennes au centre d’endoscopie digestive du CHU Gabriel Touré de Bamako (Mali): à propos de 40 cas. J Afr Hepatol Gastroenterol 9:35–38
Sakthivel H, Sahoo AK, Chinnakkulam Kandhasamy S, Amaranathan A, Goneppanavar M, Negalamangala Ramakrishnaiah VP (2018) Comparison of endoscopic variceal ligation with endoscopic sclerotherapy for secondary prophylaxis of variceal hemorrhage: a randomized trial. Cureus 10(7):e2977
Razafindrazoto CI, Razafindrabekoto LDE, Hasina Laingonirina DH et al (2022) Carvedilol versus propranolol in the prevention of variceal rebleeding in hepatosplenic schistosomiasis: efficacy and safety. JGH Open 6:213–218
Opio CK, Rejani L, Kazibwe F, Ocama P (2019) The diagnostic accuracy of routine clinical findings for detection of esophageal varices in rural sub-Saharan Africa where schistosomiasis is endemic. Afri Health Sci 19(4):3225–3234
Abdela SG, Hassen NG, Hussien FM, Yesuf AM, van Griensven J, van Henten S (2021) Hepatosplenic schistosomiasis, the ignored morbidity: experience from a referral hospital in Ethiopia. Trans R Soc Trop Med Hyg 115(1):57–62
Afredj N, Debi N, Nani A, Guessab N, Boucekkline T (2009) Prophylaxie secondaire de la rupture des varices œsophagiennes. Expérience algéroise. Endoscopy 33(3):384
Van Stiegman G (2000) Variceal bleeding prophylaxis: variceal banding or propranolol. HBP Surg 11(6):425–428
Lim EJ, Gow PJ, Angus PW (2009) Endoscopic variceal ligation for primary prophylaxis of esophageal variceal hemorrhage in pre-liver transplant patients. Liver Transpl 15(11):1508–1513
Lo GH (2010) The role of endoscopy in secondary prophylaxis of esophageal varices. Clin Lever Dis 32:230–233
Khattak AK, Manan F, Din RU (2013) Outcome of endoscopic band ligation for oesophageal variceal bleed in patients with chronic liver disease. Gomal J Med Sci 11(1):84–87
Lo GH, Chen WC, Chen MH et al (2002) Banding ligation versus nadolol and isosorbide mononitrate for the prevention of esophageal variceal rebleeding. Gastroenterology 123:728–734
Patch D, Sabin CA, Goulis J et al (2002) A randomized controlled trial of medical therapy versus endoscopic ligation for the prevention of variceal rebleeding patients with cirrhosis. Gastroenterology 123:1013–1019
Sarin SK, Lamba GS, Kumar M, Misra A, Marthy NS (1999) Comparison of endoscopic ligation and propranolol for the primary prevention of variceal bleeding. N Engl J Med 340:988–993
Sheibani S, Khemichian S, Kim JJ et al (2016) Randomized trial of 1-week versus 2-week intervals for endoscopic ligation in the treatment of patients with esophageal variceal bleeding. Hepatology 64(2):549–555
Yoshida H, Mamada Y, Taniai N et al (2005) A randomized control trial of bi-monthly versus bi-weekly endoscopic variceal ligation of esophageal varices. Am J Gastroenterol 100(9):2005–2009
Wang J, Chen S, Naga YM et al (2021) Esophageal variceal ligation monotherapy versus combined ligation and sclerotherapy for the treatment of esophageal varices. Can J Gastroenterol Hepatol 29:8856048
Luz GO, Maluf-Filho F, Matuguma SE, Hondo FY (2008) Comparison of endoscopic sclerosis with endoscopic band ligation for hemostasis of active hemorrhage elicited by rupture of esophageal varices. Gastrointest Endosc 67:AB189
Lo G-H, Chen W-C, Chen M-H, Tsai W-L (2004) The characteristics and the prognosis for patients presenting with actively bleeding esophageal varices at endoscopy. Gastrointest Endosc 60:714–720
Battagua G, Cowa F, Morbm T, Carta A, Paternello E (2000) Endoscopic band ligation of esophageal varices: long term results. Dig Liver Dis 32:A128
Chandrasekhara V, Yepuri J, Sreenarasimhaiah J (2007) Clinical predictors for recurrence of esophageal varices after obliteration by endoscopic band ligation. Gastrointest Endosc 65:AB148
Cheung J, Zeman M, van Zanten SV, Tandon P (2009) Systematic review: secondary prevention with band ligation, pharmacotherapy or combination therapy after bleeding from oesophageal varices. Aliment Pharmacol Ther 30:577–588
Guo H, Zhang M, Zhang N et al (2022) Number of endoscopic sessions to eradicate varices identifies high risk of rebleeding in cirrhotic patients. BMC Gastroenterol 22:213
Xu L, Ji F, Xu Q-W, Zhang M-Q (2011) Risk factors for predicting early variceal rebleeding after endoscopic variceal ligation. Word J Gastroenterol 17(28):3347–3352
Harewood GC, Baron TH, Kee Song LMW (2006) Factors predicting success of endoscopic variceal ligation for secondary prophylaxis of esophageal variceal bleeding. J Gastroenterol Hepatol 21(1 Pt 2):237–241
Acknowledgements
The authors would like to thank the teams of the Gastroenterology and Gastrointestinal Endoscopy Unit of the Joseph Raseta Befelatanana University Hospital, Antananarivo, Madagascar.
Funding
This research was not supported by any specific grant from public, commercial, or nonprofit funding agencies.
Author information
Authors and Affiliations
Contributions
All authors have contributed significantly to finish this work; all authors agree with the content of the article. RCI, NHR, and JAR designed the study, contributed to the acquisition of the data, interpreted the data, and drafted the article. SRR, BMR, HR, AFR, MR, DHL, SM, ASR, ALRR, THR, SHR, and RMR revised and approved the final version of the article. RCI submitted the article.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was ethically and scientifically approved by Ethic Committee of University Hospital Joseph Raseta Befelatanana, with a waiver for informed consent as all patients were de-identified. All study procedures were conducted in accordance with the Declaration of Helsinki. All authors had access to the study data and reviewed and approved the final manuscript before submission.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Razafindrazoto, C.I., Randriamifidy, N.H., Rakotomalala, J.A. et al. Endoscopic variceal ligation in primary and secondary prevention of variceal bleeding: a retrospective study in Digestive Endoscopy Unit, University Hospital Joseph Raseta Befelatanana, Antananarivo, Madagascar. Egypt Liver Journal 13, 60 (2023). https://doi.org/10.1186/s43066-023-00295-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43066-023-00295-3