Abstract
Background/Aims
We retrospectively compared the effect of endoscopic variceal obturation (EVO) and retrograde transvenous obliteration (RTO) in acute cardiofundal variceal bleeding.
Methods
Patients with acute cardiofundal variceal bleeding treated with EVO or RTO at two hospitals were included.
Results
Ninety patients treated with EVO and 86 treated with RTO were analyzed. The mean model for end-stage liver disease score was significantly higher in EVO group than in RTO group (13.5 vs. 11.7, P = 0.016). The bleeding control rates were high (97.8% vs. 96.5%), and the treatment-related complication rates were low in both EVO and RTO groups (2.2% vs. 3.5%). During the median follow-up of 18.0 months, gastric variceal (GV) and esophageal variceal rebleeding occurred in 34 (19.3%) and 7 (4.0%) patients, respectively. The all-variceal rebleeding rates were comparable between EVO and RTO groups (32.4% vs. 20.8% at 2-year, P = 0.150), while the GV rebleeding rate was significantly higher in EVO group than in RTO group (32.4% vs. 12.8% at 2-year, P = 0.003). On propensity score-matched analysis (71 patients in EVO vs. 71 patients in RTO group), both all-variceal and GV rebleeding rates were significantly higher in EVO group than in RTO group (all P < 0.05). In Cox regression analysis, EVO (vs. RTO) was the only significant predictor of higher GV rebleeding risk (hazard ratio 3.132, P = 0.005). The mortality rates were similar between two groups (P = 0.597).
Conclusions
Both EVO and RTO effectively controlled acute cardiofundal variceal bleeding. RTO was superior to EVO in preventing all-variceal and GV rebleeding after treatment, with similar survival outcomes.
Similar content being viewed by others
Introduction
Gastric varices (GVs) are enlarged submucosal veins of the stomach that are present in approximately 20% of patients with liver cirrhosis [1]. Bleeding from GVs is less frequent than from esophageal varices (EVs), with a bleeding rate of 25% over 2 years [1]. However, GVs that bleed are mostly large and have high blood flow, which can result in severe bleeding [1,2,3,4]. Moreover, rebleeding and mortality rates are also higher in GVs than in EVs [1, 5, 6].
According to their location, gastroesophageal varices (GOV) 2 and isolated GV (IGV) 1 varices are usually classified as cardiofundal varices [7]. Treatment of cardiofundal variceal bleeding can be difficult, since cardiofundal varices are larger and have more complicated blood circulation than GOV1s [8,9,10]. Accompanied collateral shunts are other barriers to achieving a complete cure of cardiofundal varices [11].
Current guidelines recommend endoscopic variceal obturation (EVO) as one of the treatment options for acute GV bleeding [7, 12, 13]. The rate of hemostasis after EVO has been reported to be as high as 91–100%; however, the rebleeding rate from GVs after EVO remains at 3.6–41.0% [14,15,16,17,18].
Recently, retrograde transvenous obliteration (RTO), including balloon-occluded (BRTO) and vascular plug-assisted RTO (PARTO), have been considered as the treatment options for acute cardiofundal variceal bleeding. High hemostasis rates (> 90%) and low rebleeding rate (0–7.43%) have been reported in patients treated with BRTO in acute GV bleeding [19,20,21]. Further, PARTO showed high technical and clinical success rates and no rebleeding events in patients with GV bleeding [22,23,24].
However, to date, an optimal treatment modality for acute cardiofundal variceal bleeding has not been confirmed. Accordingly, we compared the efficacy and safety of EVO and RTO for acute cardiofundal variceal bleeding in patients with cirrhosis.
Materials and methods
Study population
Patients with acute cardiofundal variceal bleeding who were treated with EVO or RTO between March 2006 and November 2018 at the Korea University Anam Hospital and Yonsei University Severance Hospital were retrospectively included (Fig. 1). The exclusion criteria were as follows: (a) age < 18 years, (b) insufficient follow-up period (less than 6 months), (c) previous treatment with EVs or GVs, (d) non-cirrhotic portal hypertension, (e) portal vein thrombosis, (f) advanced malignancy including hepatocellular carcinoma (HCC), and (g) history of organ transplant.
Definition
Liver cirrhosis was diagnosed either clinically or histologically when typical ultrasonographic findings were present and consistent with a low platelet count (< 100,000/μL) or overt complications of liver cirrhosis [25]. Acute cardiofundal variceal bleeding was diagnosed if the following were present on esophagastroduodenoscopy (EGD) [26, 27]: (a) active blood spurting or oozing from cardiofundal varices; (b) blood clots or white nipples on the surfaces of cardiofundal varices; (c) blood in the stomach without a potential bleeding cause other than cardiofundal varices.
Treatments
When acute cardiofundal variceal bleeding was suspected, vasoactive drugs such as terlipressin or somatostatin were administered, followed by diagnostic EGD within 12 h. When acute cardiofundal variceal bleeding was detected on EGD, EVO or RTO was performed within 6 h, depending on the presence of a gastrorenal shunt, availability of resources or expertise for RTO, and the clinician’s decision. When the clinician decided to perform RTO, endoscopists did not perform any endoscopic treatment. Patients who underwent EVO were classified into the EVO group, and those who underwent RTO, including BRTO or PARTO, were classified into the RTO group. Detailed procedures of EVO, BRTO, and PARTO are described in Additional file 1.
Outcomes
The primary outcomes were all-variceal and GV rebleeding. Rebleeding was defined as recurrent bleeding after an absence of bleeding for at least 5 days following resolution of acute GV bleeding [28]. The diagnosis of variceal rebleeding was the same as that for acute variceal bleeding. The secondary outcomes were bleeding control, treatment-related complications, and mortality. Patients were followed up until death, liver transplantation, or loss to follow-up.
Statistical analysis
Demographic and laboratory data are presented as mean ± standard deviation for continuous variables and numbers with percentages for categorical variables. Categorical and quantitative variables of the groups were compared using the chi-square test and Student's t-test, respectively.
To minimize the potential bias according to the different baseline characteristics between the EVO and RTO groups, propensity score matching (PSM) was calculated by fitting a logistic regression model that included the following variables in both the EVO and RTO cohorts: age, sex, diabetes, HCC, type of varices, size of EVs, hemoglobin, platelet count, INR, serum levels of albumin, total bilirubin and ALT, and model for end-stage liver disease (MELD) score. A 1:1 ratio PSM was performed using the nearest neighbor method.
Variceal rebleeding and mortality rates were estimated using the Kaplan–Meier method and compared using the log-rank test. The data of patients that died, received a liver transplantation, or were lost to follow-up were censored. Independent predictors for variceal rebleeding and mortality were evaluated using the Cox proportional hazard regression analysis. All statistical analyses were performed using the Statistical Package for the Social Sciences version 25.0 software (International Business Machines Corp.).
Results
Patient characteristics
Among the 307 eligible patients, a total of 176 patients were finally selected for statistical analyses (90 [51.1%] in the EVO group and 86 [48.9%] in the RTO group) (Additional file 2: Fig. S1). In the RTO group, 45 (52.3%) and 41 (47.7%) patients were treated with BRTO and PARTO, respectively. The baseline characteristics of the study population are shown in Table 1. Ninety-nine (56.3%) patients had GOV2, and 77 (43.7%) patients had IGV1. The mean MELD score was 12.6. Beta-blockers were administered to 52 (29.5%) patients after bleeding control was achieved.
Comparison between the EVO and RTO group
Baseline characteristics were statistically similar between the EVO and RTO groups (all P > 0.05), except for a significantly higher MELD score in the EVO group than in the RTO group (mean 13.5 vs. 11.7, P = 0.016) (Table 1). The proportions of GOV2 (58.9% vs. 53.5%) and IGV1 (41.1% vs. 46.5%) were statistically similar between the EVO and RTO groups (P = 0.470). Seventy patients (77.8%) in EVO group had a gastrorenal shunt feasible for RTO procedure.
The proportion of patients who were treated with beta-blockers after bleeding control was significantly higher in the RTO group than in the EVO group (47.7% vs. 12.2%, P < 0.001). The proportion of patients treated with propranolol and carvedilol was 75.0% and 25.0% in the EVO group and 73.2% and 26.8% in the RTO group, respectively (P = 0.735). The mean doses of both propranolol (48.9 mg vs. 51.7 mg, P = 0.807) and carvedilol (12.5 mg vs. 14.7 mg, P = 0.567) were statistically similar between the two groups.
Treatment outcomes
Bleeding was successfully controlled in 171 patients (97.2%). The bleeding control rate was similar between the two groups (97.8% in the EVO group vs. 96.5% in the RTO group, P = 0.613) (Additional file 2: Table S1). In 5 patients who failed to achieve bleeding control, transjugular intrahepatic portosystemic shunt were performed. Technical success was achieved in all patients in the EVO and RTO groups. Among patients in the EVO group, 48 patients achieved obliteration of the GV with one session. The other 42 patients underwent additional endoscopic intervention within 1 week of the initial treatment. The mean number of performed EVO sessions was 1.5 ± 1.0, and the mean volume of cyanoacrylate mixture used in each patient was 4.4 ± 2.7 mL.
Treatment-related complications were investigated. Two patients in the EVO group and one patient in the RTO group had worsening ascites, and two patients in the RTO group developed hepatic encephalopathy. No systemic embolization or thrombus developed in either group.
Change of esophageal varices after the treatment
After the treatment for acute cardiofundal variceal bleeding, worsening of EVs was found in 12 (14.8%) patients in the EVO group and 24 (27.9%) patients in the RTO group (P < 0.001). Among patients with F2–F3 EVs after the treatment for acute cardiofundal variceal bleeding, 25 of 36 (69.4%) in the EVO group and 25 of 32 (78.1%) in the RTO group underwent endoscopic variceal ligation (EVL) as a secondary prevention of EV bleeding.
All-variceal rebleeding
During the median follow-up period of 18.0 (interquartile range, 7.0–38.9) months, all-variceal rebleeding occurred in 41 (23.3%) patients (26 in the EVO group and 15 in the RTO group). The most common type of variceal rebleeding was GV bleeding (n = 34), followed by EV bleeding (n = 7). All EV rebleeding developed after RTO, and most cases (6 out of 7) did not receive EVL after RTO.
All-variceal rebleeding rates at 6, 12, 18, and 24 months after treatment were 6.1%, 11.1%, 17.9%, and 26.3%, respectively (Additional file 2: Table S1). The corresponding rates in the EVO and RTO groups were statistically similar (6.1%, 11.2%, 23.4%, and 32.4% vs. 6.1%, 11.1%, 12.9%, and 20.8%, respectively, P = 0.150 by log-rank test) (Fig. 1A). There was no significant difference in all-variceal rebleeding rates between the BRTO and PARTO groups (P = 0.891 by log-rank test). In the Cox regression analysis, no significant predictor of all-variceal rebleeding was found (Table 2).
We additionally evaluated whether this result was reproducible after PSM, and the clinical characteristics of patients balanced by PSM (71 patients in EVO group vs. 71 patients in RTO group) are presented in Additional file 2: Table S2. On PSM analysis, all-variceal rebleeding rate was significantly higher in the EVO group than in the RTO group (6.0%, 12.1%, 26.4%, and 37.3% vs. 4.5%, 8.3%, 10.5%, and 20.0%, respectively, P = 0.032 by log-rank test) (Fig. 1B, Additional file 2: Table S3).
GV rebleeding
GV rebleeding was analyzed separately. GV rebleeding rates at 6, 12, 18, and 24 months after treatment were 4.9%, 8.3%, 15.2%, and 22.5%, respectively (Additional file 2: Table S1). The corresponding rates in the EVO group were significantly higher than those in the RTO group (6.1%, 11.2%, 23.4%, and 32.4% vs. 3.7%, 5.4%, 7.2%, and 12.8%, respectively, P = 0.003 by log-rank test) (Fig. 2A). No significant difference in GV rebleeding rate was observed between the BRTO and PARTO groups (P = 0.838 by log-rank test). In the Cox regression analysis, EVO treatment (vs. RTO) was the only significant predictor of higher risk of GV rebleeding (hazard ratio [HR] = 3.132, 95% confidence interval [CI] 1.408–6.970, P = 0.005) (Table 2).
On PSM analysis, GV rebleeding rate was significantly higher in the EVO group than in the RTO group (6.0%, 12.1%, 26.4%, and 37.3% vs. 1.6%, 3.6%, 5.8%, and 12.5%, respectively, P < 0.001 by log-rank test) (Fig. 2B, Additional file 2: Table S3).
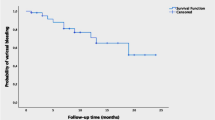
Mortality
During the follow-up period, 40 patients died (21 in the EVO group and 19 in the RTO group). The causes of death were variceal bleeding (27.5%), infection (30.0%), or liver failure (42.5%). Six patients received liver transplantation (three patients in the EVO group and three patients in the RTO group). The cumulative transplantation-free survival rates at 6, 12, 18, and 24 months after treatment were 87.5%, 84.8%, 82.2%, and 79.1%, respectively (Additional file 2: Table S1). No significant difference in transplantation-free survival rates was observed between the EVO group (86.7%, 83.9%, 80.4%, and 78.4%) and the RTO group (88.4%, 85.8%, 84.1%, and 79.9%, P = 0.597 by log-rank test) (Fig. 3A). In the Cox regression analysis, higher MELD score was the only independent predictor for higher risk of mortality (HR = 1.089, 95% CI 1.030–1.151, P = 0.002), whereas EVO (vs. RTO) was not (P = 0.598) (Table 3).
On PSM analysis, no significant difference in transplantation-free survival rates was observed between the EVO group (86.7%, 83.9%, 80.4%, and 78.4%) and the RTO group (88.4%, 85.8%, 84.1%, and 79.9%, P = 0.119 by log-rank test) (Fig. 3B, Additional file 2: Table S3).
Discussion
Currently, an optimal treatment for acute cardiofundal variceal bleeding has not been confirmed. In this study, we directly compared EVO with RTO for acute cardiofundal variceal bleeding in patients with cirrhosis and found that all-variceal rebleeding rates at 2 years were statistically similar between the two groups (P = 0.150). However, the GV rebleeding rate at 2 years was significantly higher in the EVO group than in the RTO group (P = 0.003), and EVO (vs. RTO) was the only predictor of higher risk of GV rebleeding. On PSM analysis, both all-variceal and GV rebleeding rates were significantly higher in the EVO group than in the RTO group (all P < 0.05). Finally, we found that both EVO and RTO were effective for bleeding control (> 96.5%) and had low complication rates (< 3.5%). No difference was observed in the mortality between the two groups.
This study has several important clinical implications. In the present study, 1- and 2-year all-variceal rebleeding rates were statistically similar between the two groups. However, when patients were analyzed for GV rebleeding, the EVO group had significantly higher 1- and 2-year GV rebleeding rates than those in the RTO group. The difference between all-variceal and GV rebleeding rates could be explained by the high EV rebleeding rate after RTO. Rebleeding from EVs developed in seven patients treated with RTO; 6 out of 7 did not receive EVL after RTO. In the present study, 14.8% of patients in the EVO group and 27.9% of patients in the RTO group developed worsening of EVs after bleeding control (P < 0.001). A recent randomized controlled study reported an EV worsening rate of 30% and 43.5% in the EVO and BRTO groups, respectively [29], and similar results have been frequently reported in previous studies [9, 30,31,32,33]. Because RTO completely obliterates the portosystemic shunts that supply GVs, worsening of portal hypertension and its complications have been widely observed [34, 35]. Thus, screening endoscopy and appropriate prophylaxis with EVL could decrease EV rebleeding after RTO [29].
To minimize the potential bias according to the differences in baseline characteristics between the EVO and RTO groups, particularly in MELD scores, PSM analysis was performed. On PSM analysis, both 1- and 2-year all-variceal and GV rebleeding rates were significantly higher in EVO group than in RTO group. To our knowledge, three studies directly compared EVO and BRTO in terms of GV bleeding, and all studies demonstrated the superiority of BRTO over EVO in preventing variceal rebleeding [27, 29, 36]. A retrospective study of cardiofundal variceal bleeding found lower rates of rebleeding following BRTO compared to EVO; however, 16/71 patients who underwent BRTO had simultaneous transjugular intrahepatic portosystemic shunts, which could improve portal hypertension and further decrease GV rebleeding [36]. Recently, a randomized controlled study compared EVO with BRTO for secondary prophylaxis of cardiofundal GV bleeding [29]. However, the number of patients was small (32 patients in EVO group vs. 32 patients in BRTO group). Additionally, 67.2% of patients were transferred patients who had recovered from a previous GV bleeding within 4 weeks. A prospective study also found a higher variceal rebleeding rate for EVO than for BRTO (71.4% vs. 15.4%); however, BRTO was performed only in patients without active bleeding [27].
The rates of recurrence and rebleeding of GVs after successful RTO are low, possibly because the injected sclerosing agent completely destroys the venous endothelium. [30, 31]. The higher rebleeding rate in patients treated with EVO may be related to incomplete impaction of cyanoacrylate, leading to less or delayed obturation of GVs and their feeding vessels. Additionally, the results of EVO vary according to the clinician’s experience. Therefore, clinicians should seek the best option for each patient based on the patient’s general condition and access to appropriate medical resources and expertise in clinical practice.
The one of most common causes of death after acute cardiofundal variceal bleeding was variceal rebleeding (27.5%), emphasizing the need for proper prevention of variceal rebleeding after bleeding control is achieved. There was no significant difference in transplantation-free survival between the EVO and RTO groups, and a higher MELD score was the only predictor of increased mortality, consistent with the results of previous studies [27, 29].
The major limitation of our study is its retrospective design, which could have resulted in selection bias. Apparantly, patients in the EVO group had significantly worse liver function than those in the RTO group. Therefore, we conducted robust PSM analysis with large number of variables to minimize potential bias. In addition, due to the small number of patients who received beta-blockers, whether adding beta-blockers, known to have beneficial effects in the prognosis of patients with liver cirrhosis, can reduce rebleeding or mortality has not been elucidated by the current results. Finally, this study included both BRTO and PARTO, which are different treatment modalities that use different sclerosing agents. Although no differences were observed in all-variceal and GV rebleeding rates between the two groups, these results are not conclusive due to the small number of patients in each group. Further randomized controlled studies with larger numbers of patients are needed to confirm the optimal treatment strategy for patients with acute cardiofundal variceal bleeding.
In conclusion, our study shows that both RTO and EVO are effective and safe methods, however, RTO is more effective than EVO in preventing all-variceal and GV rebleeding, with similar survival outcomes. The worsening of EVs after BRTO should be screened and managed appropriately. EVO could be another effective option for acute cardiofundal variceal bleeding, especially in a clinical setting that lacks resources or expertise for RTO.
Availability of data and materials
The datasets are available from the corresponding author on reasonable request.
Abbreviations
- GVs:
-
Gastric varices
- EVs:
-
Esophageal varices
- GOV:
-
Gastroesophageal varices
- IGV:
-
Isolated gastric varices
- EVO:
-
Endoscopic variceal obturation
- RTO:
-
Retrograde transvenous obliteration
- BRTO:
-
Balloon-occluded retrograde transvenous obliteration
- PARTO:
-
Vascular plug-assisted retrograde transvenous obliteration
- HCC:
-
Hepatocellular carcinoma
- EGD:
-
Esophagastroduodenoscopy
- PSM:
-
Propensity score matching
- MELD:
-
Model for end-stage liver disease
- EVL:
-
Endoscopic variceal ligation
- HR:
-
Hazard ratio
- CI:
-
Confidence interval
References
Sarin SK, Lahoti D, Saxena SP, et al. Prevalence, classification and natural history of gastric varices: a long-term follow-up study in 568 portal hypertension patients. Hepatology. 1992;16:1343–9.
Ryan BM, Stockbrugger RW, Ryan JM. A pathophysiologic, gastroenterologic, and radiologic approach to the management of gastric varices. Gastroenterology. 2004;126:1175–89.
Thakeb F, Salem SA, Abdallah M, et al. Endoscopic diagnosis of gastric varices. Endoscopy. 1994;26:287–91.
Lesmana CRA, Raharjo M, Gani RA. Managing liver cirrhotic complications: overview of esophageal and gastric varices. Clin Mol Hepatol. 2020;26:444–60.
de Franchis R, Primignani M. Natural history of portal hypertension in patients with cirrhosis. Clin Liver Dis. 2001;5:645–63.
Sarin SK. Long-term follow-up of gastric variceal sclerotherapy: an eleven-year experience. Gastrointest Endosc. 1997;46:8–14.
Korean Association for the Study of the Liver. KASL clinical practice guidelines for liver cirrhosis: varices, hepatic encephalopathy, and related complications. Clin Mol Hepatol. 2020;26:83–127.
Watanabe K, Kimura K, Matsutani S, et al. Portal hemodynamics in patients with gastric varices. A study in 230 patients with esophageal and/or gastric varices using portal vein catheterization. Gastroenterology. 1988;95:434–40.
Saad WE. Vascular anatomy and the morphologic and hemodynamic classifications of gastric varices and spontaneous portosystemic shunts relevant to the BRTO procedure. Tech Vasc Interv Radiol. 2013;16:60–100.
Lee HA, Goh HG, Seo YS, et al. Evaluation of treatment response after endoscopic variceal obturation with abdominal computed tomography. Gut Liver. 2020;14:117–24.
Maruyama H, Okugawa H, Yoshizumi H, et al. Hemodynamic features of gastrorenal shunt: a Doppler study in cirrhotic patients with gastric fundal varices. Acad Radiol. 2008;15:1148–54.
Garcia-Tsao G, Abraldes JG, Berzigotti A, et al. Portal hypertensive bleeding in cirrhosis: risk stratification, diagnosis, and management—2016 practice guidance by the American Association for the study of liver diseases. Hepatology. 2017;65:310–35.
European Association for The Study of the Liver. EASL clinical practice guidelines for the management of patients with decompensated cirrhosis. J Hepatol. 2018;69:406–60.
Park SJ, Seo YS, Lee HA, et al. Cyanoacrylate injection versus band ligation for bleeding from cardiac varices along the lesser curvature of the stomach. Clin Mol Hepatol. 2016;22:487–94.
Qiao W, Ren Y, Bai Y, et al. Cyanoacrylate injection versus band ligation in the endoscopic management of acute gastric variceal bleeding: meta-analysis of randomized, controlled studies based on the PRISMA statement. Medicine (Baltimore). 2015;94:e1725.
Caldwell SH, Hespenheide EE, Greenwald BD, et al. Enbucrilate for gastric varices: extended experience in 92 patients. Aliment Pharmacol Ther. 2007;26:49–59.
Hou MC, Lin HC, Lee HS, et al. A randomized trial of endoscopic cyanoacrylate injection for acute gastric variceal bleeding: 0.5 mL versus 1.0 mL. Gastrointest Endosc. 2009;70:668–75.
Marques P, Maluf-Filho F, Kumar A, et al. Long-term outcomes of acute gastric variceal bleeding in 48 patients following treatment with cyanoacrylate. Dig Dis Sci. 2008;53:544–50.
Choi YH, Yoon CJ, Park JH, et al. Balloon-occluded retrograde transvenous obliteration for gastric variceal bleeding: its feasibility compared with transjugular intrahepatic portosystemic shunt. Korean J Radiol. 2003;4:109–16.
Sabri SS, Abi-Jaoudeh N, Swee W, et al. Short-term rebleeding rates for isolated gastric varices managed by transjugular intrahepatic portosystemic shunt versus balloon-occluded retrograde transvenous obliteration. J Vasc Interv Radiol. 2014;25:355–61.
Wang YB, Zhang JY, Gong JP, et al. Balloon-occluded retrograde transvenous obliteration versus transjugular intrahepatic portosystemic shunt for treatment of gastric varices due to portal hypertension: a meta-analysis. J Gastroenterol Hepatol. 2016;31:727–33.
Kim T, Yang H, Lee CK, et al. Vascular plug assisted retrograde transvenous obliteration (PARTO) for gastric varix bleeding patients in the emergent clinical setting. Yonsei Med J. 2016;57:973–9.
Gwon DI, Ko GY, Kwon YB, et al. Plug-assisted retrograde transvenous obliteration for the treatment of gastric varices: the role of intra-procedural cone-beam computed tomography. Korean J Radiol. 2018;19:223–9.
Chang MY, Kim MD, Kim T, et al. Plug-assisted retrograde transvenous obliteration for the treatment of gastric variceal hemorrhage. Korean J Radiol. 2016;17:230–8.
Seo YS, Shah VH. Pathophysiology of portal hypertension and its clinical links. J Clin Exp Hepatol. 2011;1:87–93.
Seo YS. Prevention and management of gastroesophageal varices. Clin Mol Hepatol. 2018;24:20–42.
Hong CH, Kim HJ, Park JH, et al. Treatment of patients with gastric variceal hemorrhage: endoscopic N-butyl-2-cyanoacrylate injection versus balloon-occluded retrograde transvenous obliteration. J Gastroenterol Hepatol. 2009;24:372–8.
de Franchis R. Revising consensus in portal hypertension: report of the Baveno V consensus workshop on methodology of diagnosis and therapy in portal hypertension. J Hepatol. 2010;53:762–8.
Luo X, Xiang T, Wu J, et al. Endoscopic cyanoacrylate injection versus balloon-occluded retrograde transvenous obliteration for prevention of gastric variceal bleeding: a randomized controlled trial. Hepatology. 2021;74(4):2074–84.
Garcia-Pagán JC, Barrufet M, Cardenas A, et al. Management of gastric varices. Clin Gastroenterol Hepatol. 2014;12:919-928.e911.
Lee EW, Shahrouki P, Alanis L, et al. Management options for gastric variceal hemorrhage. JAMA Surg. 2019;154:540–8.
Imai Y, Nakazawa M, Ando S, et al. Long-term outcome of 154 patients receiving balloon-occluded retrograde transvenous obliteration for gastric fundal varices. J Gastroenterol Hepatol. 2016;31:1844–50.
Jang SY, Kim GH, Park SY, et al. Clinical outcomes of balloon-occluded retrograde transvenous obliteration for the treatment of gastric variceal hemorrhage in Korean patients with liver cirrhosis: a retrospective multicenter study. Clin Mol Hepatol. 2012;18:368–74.
Miyamoto Y, Oho K, Kumamoto M, et al. Balloon-occluded retrograde transvenous obliteration improves liver function in patients with cirrhosis and portal hypertension. J Gastroenterol Hepatol. 2003;18:934–42.
Uehara H, Akahoshi T, Tomikawa M, et al. Prediction of improved liver function after balloon-occluded retrograde transvenous obliteration: relation to hepatic vein pressure gradient. J Gastroenterol Hepatol. 2012;27:137–41.
Stein DJ, Salinas C, Sabri S, et al. Balloon retrograde transvenous obliteration versus endoscopic cyanoacrylate in bleeding gastric varices: comparison of rebleeding and mortality with extended follow-up. J Vasc Interv Radiol. 2019;30:187–94.
Acknowledgements
We would like to thank Editage (www.editage.co.kr) for English language editing.
Funding
None.
Author information
Authors and Affiliations
Contributions
Conception and design: SUK and YSS; Development of methodology: SUK and YSS; Acquisition, analysis, and interpretation of data: HAL, JK, SBC, YL, YKJ, JHK, HA, HJY, YTJ, JEY, and KSB; Writing, review, and/or revision of the manuscript: HAL, JK, SUK and YSS; Administrative, technical, or material support: SUK and YSS; Study supervision: SUK and YSS. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study protocol conformed with the ethical guidelines of the 1975 Declaration of Helsinki and was approved by the human ethics committee of each hospital (Institutional Review Board of Korea University College of Medicine, Institutional Review Board of Yonsei University College of Medicine). The requirement for informed consent was waived due to the retrospective design of the study by the Institutional Review Board of Korea University College of Medicine, Institutional Review Board of Yonsei University College of Medicine.
Consent for publication
Not applicable.
Competing interests
Seung Up Kim served as an advisory committee member, Gilead Sciences, GSK, Bayer, and Eisai. He is a speaker for Gilead Sciences, GSK, Bayer, Eisai, Abbive, EchoSens, MSD, and Bristol–Myers Squibb. He also received a research grant from Abbive, Bristol–Myers Squibb. The other authors declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Supplementary Note.
Additional file 2.
Supplementary Figure 1. Flowchart of patients.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lee, H.A., Kwak, J., Cho, S.B. et al. Endoscopic variceal obturation and retrograde transvenous obliteration for acute gastric cardiofundal variceal bleeding in liver cirrhosis. BMC Gastroenterol 22, 355 (2022). https://doi.org/10.1186/s12876-022-02428-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12876-022-02428-1