Abstract
Introduction
To date, alpha-feto protein (AFP) remains the most widely used serum biomarker for hepatocellular carcinoma (HCC) diagnosis and prognosis. However, its role has become controversial as close to 30% of early stage HCC patients are AFP negative. Different studies on the diagnostic performance of novel AFP-negative HCC biomarkers have shown inconsistent results of sensitivity, specificity, and area under the receiver operating curve (AUROC). Here, we conducted a systematic review and meta-analysis to resolve this inconsistency.
Methods
Relevant studies were systematically searched from PubMed, Embase, Cochrane library, Scopus, and the China National Knowledge Infrastructure (chkd-cnki) databases up to the 20th October 2022. The Newcastle–Ottawa Scale was used to assess the methodological quality of included studies. Sensitivity, specificity, and area under the curve were pooled using the random effect model.
Results
Five studies, with a total of 286 patients, were included. Serum Midkine was assessed using enzyme-linked immunosorbent assay (ELISA) in all the studies, at diagnostic thresholds varying from 0.387 to 5.1 ng/ml. The summary estimates for serum Midkine were 76% (95% CI 70–81%) sensitivity, 85% (95% CI 82–87%) specificity, and 91% area under the receiver operating characteristic curve (AUC), while the pooled diagnostic odds ratio (DOR) was 27.64 (95% CI 4.95–154.17).
Conclusion
Based on these findings, serum Midkine is a very promising diagnostic biomarker for AFP-negative HCC and should be validated further in large cohort studies.
Similar content being viewed by others
Introduction
Liver cancer is the 6th most common human malignancy (4.7% of total cases), and the 3rd most deadly (8.3% of all cancer deaths) globally [1]. Hepatocellular carcinoma (HCC) is its most frequent and aggressive form, accounting for over 90% of all cases, and causing an estimated 782, 000 deaths annually [1]. Its 5-year survival rate is less than 20% world over [2], and just over 12% in China [3], but can go beyond 70% when diagnosed early [4]. Thus, early diagnosis is crucial for timely, optimal, and effective therapy. Major HCC risk factors include hepatitis B and hepatitis C virus (HCV) infection, excessive alcohol consumption, liver cirrhosis, and other associated metabolic diseases [5, 6]. To date, alpha-feto protein remains the most widely used serum biomarker for HCC diagnosis, recommended alongside routine 6 months ultrasound examination for HCC screening in China [7]. However, this role of AFP in HCC screening remains controversial. A recent study demonstrated that AFP sensitivity for HCC diagnosis was as low as 60% at the usual cutoff value of < 20 ng/ml [8], while another reported that only 33–65% of HCC patients with tumor diameter < 3 cm had elevated serum AFP level (> 20 ng/mL) [9]. Moreover, up to 30% of all early stage HCC patients are AFP negative [10, 11]. For these reasons, AFP is not recommended in the European and American guidelines for HCC diagnosis and prognosis [12, 13]. However, since it is still widely used in other parts of the world, especially south East Asia, it is crucial that new biomarkers are sought for, especially for AFP-negative HCC (ANHC) patients.
According to a recent study [14], serum Midkine exhibited impressive diagnostic performance for early stage HCC and AFP-negative HCC. Midkine is a low molecular weight protein that is highly expressed during fetal development, but is low to undetectable in adulthood [15]. Recent findings about its role in HCC, such as promoting tumor proliferation, and anti-apoptosis tendencies [16], coupled with its upregulated expression in HCC relative to normal individuals [16,17,18,19], have made it the most promising biomarker for early stage HCC. Most importantly, secondary analyses of these HCC early diagnosis studies for its potential diagnostic significance in AFP-negative patients have shown remarkable results. A subgroup analysis in the meta-analysis by Lu et al. [20] combined three studies of Midkine and showed that it had a combined AUC of 91%, with sensitivity and specificity of 88.5% and 83.9%, respectively. However, a thorough literature search revealed that a few more eligible studies were not included in the meta-analysis, and since then, other new studies have come out [18, 21, 22]. Therefore, an updated meta-analysis is warranted. Midkine expression continues to draw scientific enthusiasm because it is detectable in pre-clinical tumor samples [18], which makes it a possible candidate for early stage HCC diagnosis, and its expression shows strong correlations with key features of HCC progression, such as vascular invasion and multiple nodule development, which are pre-metastatic characteristics [21]. A recent study by Vongsuvanh et al. [18] further revealed that Midkine is particularly superior to AFP in detecting NASH-associated HCC.
Other potential AFP-negative HCC biomarkers that have been explored include Osteopontin, DKK1, and a host of genetic and clinical biomarkers such as circular RNAs, microRNAs, and blood cell indices [23]. Although the pathways that drive HCC pathogenesis are complex in nature and may require profiling a combination of biomarkers as opposed to a single biomarker, AFP-negative HCC is an emergent subset that is still largely unknown and requires further studies to unravel. In this subgroup of HCC, Midkine has shown superior diagnostic promise and should be assessed further for its possible role in clinical practice. Since the results were inconsistent across different studies, to resolve the controversy, we sought to systematically explore these studies and pooled their effect sizes to determine Midkine’s diagnostic capacity in AFP-negative HCC patients. We further explored its combined sensitivity, specificity, diagnostic odds ratio, and positive and negative likelihood ratios in diagnosing AFP-negative HCC.
Materials and methods
Literature search strategy
The updated Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guideline [24] was followed to conduct this meta-analysis. PubMed, Embase, Cochrane Library, Scopus, and the China National Knowledge Infrastructure (chkd-cnki) databases were systematically searched for all eligible studies published until the 20th of October 2022. All studies that assessed Midkine expression in AFP-negative HCC were searched and retrieved. Studies on early HCC diagnosis were retrieved, and thoroughly read, and if they had data on AFP-negative HCC, such data were extracted. The search terms were (‘Midkine’ or ‘MDK’ or ‘MK’) and (‘Carcinoma, Hepatocellular’ or ‘Liver Neoplasms’ or ‘hepatocarcinoma*’ or ‘hepatoma*’or ‘HCC’ or ((‘Hepatocellular’ or ‘liver cell’ or ‘hepatic cell’ or ‘liver’) and (‘carcinoma*’or ‘tumor’))). Since AFP-negative HCC lacks specific studies, literature on novel HCC biomarkers and early HCC diagnosis were thoroughly read to retrieve any usable information on Midkine in AFP-negative HCC. References of the relevant studies were also thoroughly searched for any additional papers.
Inclusion and exclusion criteria
Studies were included in the analysis if they met the following criteria: (1) directly assessed the diagnostic ability of Midkine in AFP-negative HCC patients vs. controls. (Controls were considered to be healthy subjects, hepatitis B patients, or liver cirrhosis patients). (2) Had enough data to construct a 2 × 2 table having true positives (TPs), false positives (FPs), true negatives (TNs), and false negatives (FNs). (3) Only serological samples were used to determine the levels of the biomarker in AFP-negative HCC patients. (4) HCC diagnosis was confirmed by histology or an appropriate imaging technique as defined by accepted guidelines. Studies were excluded if they had the following characteristics: (1) were abstracts only, or conference papers, editorials, letters, guidelines, reviews, and case reports; (2) were conducted in animals or cellular experiments; and (3) were irrelevant to AFP-negative HCC.
Definition of key terms
HCC was defined as diagnosis based on microscopic pathology or CT and MRI as defined in the diagnosis guidelines [25]. Hepatitis virus-related HCC was defined as HCC that originated from a previous chronic hepatitis virus infection and subsequent cirrhosis, while early-stage HCC and AFP-negative HCC were defined according to the BCLC 0-A (Barcelona Clinic Liver Cancer) classification and AFP < 20 ng/ml, respectively.
Data extraction and quality assessment
Data was extracted using a pre-defined data extraction sheet. The extraction was conducted by two reviewers; one extracting and the other proofreading to confirm that no errors were made. Data extracted were on the study authors, year of publication, country of study, study type, sample type used, sample size, AFP status, control subjects used, method of biomarker detection, cutoff values, and the performance indices TP, FP, FN, and TN. Quality assessment for the included studies were conducted using the Newcastle–Ottawa scale [26]. Data extraction and quality assessment were conducted by two independent authors. Any disagreements between the reviewers were resolved through dialog.
Statistical analyses
The Cochrane Collaboration Software Review Manger version 5.4.1 (Cochrane Collaboration, UK) and the Meta-Disc software version 1.4 (Hospital Ramón y Cajal, Spain) were used for statistical analyses. Pooled sensitivity (Se), specificity (Sp), positive likelihood ratio (PLR), negative likelihood ratio (NLR), and diagnostic odds ratio (DOR) were calculated and the summary receiver operating characteristic (SROC) curve drawn, with its corresponding AUC using the DerSimonian–Laird random effect model. A perfect diagnostic tool is one with an AUC of 1.00, and 0.90 is considered excellent, 0.80 good, and < 0.80 moderate [27].
Study heterogeneity and publication bias
Here, heterogeneity meant the degree of variations among the individual studies’ effect sizes (AUCs). The chi-square test and the Higgins and Thompson I2 test [28] were used to assess heterogeneity. I2 < 25% was considered low heterogeneity, 25–75%, moderate, and > 75% high. The Spearman’s correlation coefficient was used to verify potential threshold effects where applicable, a strong positive correlation proves that threshold effect exists. Funnel plots and Egger’s test for publication bias were not conducted since in the studies were less than ten in number [29]. A two sided p value < 0.05 was considered statistically significant.
Results
Characteristics of included studies
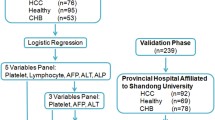
A total of 621 studies were initially retrieved, 603 were excluded due to duplication, abstract only papers, lack of enough data to construct 2 × 2 tables, and non-relevance to AFP-negative HCC. As a result, 5 studies were recruited [14, 16, 18, 19, 22]. When combined, the studies evaluated 286 AFP-negative patients. The study flow diagram is presented in Fig. 1. Included studies were published between 2013 and 2021. Three were from Egypt, 1 from Australia, and 1 from China. In all studies, serum Midkine level was determined by enzyme-linked immunosorbent assay (ELISA). Information about the studies is presented in Table 1. The Newcastle–Ottawa Scale was used for study quality assessment, and the results are presented in Supplementary table S1. Generally, the studies were of average quality as none was randomized, some retrospective, and all of them assessed AFP-negative HCC patients secondary to early diagnosis of HCC, hence had design flaws.
Systematic review
The study by Zhu et al. [14] was the earliest and had the most number of AFP-negative HCC patients evaluated (n = 181). This study evaluated Midkine as a diagnostic serum biomarker in hepatocellular carcinoma and recruited 388 HCC patients, 181 of whom were AFP negative. They found that Midkine had an outstanding performance in distinguishing AFP-negative patients from healthy control subjects, with an AUC as high as 92.6% (95% CI 90.3–94.9%). Furthermore, it satisfactorily distinguished AFP-negative HCC from liver cirrhosis patients, with an AUC of 93.1% (95% CI 89.8–96.4%). The diagnostic threshold was 0.654 ng/ml; however, sensitivity, specificity, and other diagnostic characteristics associated with threshold were not explicitly stated. Vongsuvanh et al. [18] evaluated Midkine in AFP-negative and NASH-associated HCC patients and found that Midkine expression is significantly associated with both HCC characteristics. Specifically, Midkine was elevated in 59.18% (n = 29/49) of the AFP-negative HCC patients at a diagnostic threshold of 0.44 ng/ml. A Spearman’s rank correlation analysis to determine the relationship between Midkine and AFP releveled a rho value of 0.257 (P = 0.017), suggesting no association between the two biomarkers in HCC development. The authors further evaluated Midkine expression longitudinally for 6 months in 14 AFP-negative patients and discovered that 50% of them had elevated Midkine level at HCC diagnosis, while 33% had elevated Midkine 6 months prior. These findings are strongly suggestive of a role for Midkine in pre-clinical and early diagnosis of HCC, hence should be validated in a larger study.
Mashaly et al. [16], Shaheen et al. [19], and El-Shayeb et al. [22] evaluated serum Midkine in Egyptian patients. These studies combined had a total of just 56 AFP-negative HCC patients. Mashaly et al. assessed the diagnostic and prognostic value of serum Talin-1 and Midkine as markers of HCC in Egyptian patients. Of the 44 HCC cases, 21 (47.7%) were AFP-negative, and serum Midkine was positive in 80.9% (17/21) of them, at a diagnostic threshold of 1.683 ng/ml. Shaheen et al. on the other hand analyzed serum Midkine in 15 AFP-negative HCC patients, 93.3% (14/15) of whom had elevated Midkine at a diagnostic threshold of 0.387 ng/ml. In this study, liver cirrhosis was the control group. El-Shayeb et al., meanwhile, compared the sensitivity of serum Midkine and Dickkopf-1 and alpha-L-fucosidase as predictors of hepatocellular carcinoma in cirrhotic HCV patients. They concluded that serum Midkine had superior diagnostic qualities to the other biomarkers. Most importantly, 19 of the patients were AFP negative, and serum Midkine was elevated in all of them (19/19) at a diagnostic threshold of 5.1 ng/ml, giving it a 100% sensitivity to distinguish HCC and HCV-associated cirrhosis patients, despite the significantly higher diagnostic threshold compared to the other studies. Whether this is a coincidence or Midkine is positively associated with HCV infection needs to be investigated further.
Meta-analysis
All the five studies had adequate information to calculate the true positive (TP), false positive (FP), false negative (FN), and true negative (TN) values required to construct a 2 × 2 table and pool the study effect sizes. Consequently, a diagnostic meta-analysis was conducted using the Meta-Disc software version 1.4. DerSimonian–Laird random effect model was adopted, and the sensitivity, specificity, diagnostic odds ratio, and area under the receiver operating characteristic curve were pooled. As advised in the Effective Health Care Program, Agency for Healthcare Research and Quality guide on diagnostic meta-analysis [30], the positive likelihood ratio and negative likelihood ratios were further calculated from the pooled sensitivity and specificity values.
The pooled sensitivity and specificity, and AUC were 76% (95% CI 70–81%), 85% (95% CI 82–87%), and 91%, respectively (Fig. 2), while the pooled diagnostic odds ratio (DOR) was 27.64 (95% CI 4.95–154.17) (Fig. 3). Positive likelihood ratio (PL +) was calculated from the pooled sensitivity and specificity values as PL + = sensitivity/1-specifty, = 5.1 (Fig. 4). Similarly, negative likelihood ratio (LR-) was calculated as 1-sensitivity/specificity, = 0.47 (Fig. 5). A perfect diagnostic tool is one with an AUC of 1.00, and 0.90 is considered excellent, 0.80 good, and < 0.80 moderate [27]. Accordingly, serum Midkine is an excellent diagnostic biomarker for AFP-negative HCC, although the total study population was small and so the results need validation in a larger well-designed cohort.
Heterogeneity
Study heterogeneity was assessed by eyeballing the forest plots, and statistically using the Q statistics, and the inconsistency index (I2). The effect sizes had relatively high heterogeneity as captured in the forest plots. Heterogeneity results from various factors, among which is the use of different diagnostic thresholds by different studies to diagnose a positive case. Among the included studies, one was an outlier with a diagnostic threshold significantly higher than the others. To rule out threshold effect, Spearman correlation analysis was conducted. The correlation coefficients was − 0.100 (p = 0.873), suggesting that threshold effect did not exist. Therefore, heterogeneity was most likely due to other factors other than threshold effect.
Discussion
The need for a reproducible diagnostic biomarker to be deployed in the surveillance of HCC, especially AFP-negative HCC is evident [25]. Currently, no biomarker has been approved for detecting AFP-negative HCC, making the diagnostic process cumbersome, delayed, and costly for these patients. This meta-analysis thus assessed the diagnostic potential of serum Midkine for AFP-negative hepatocellular carcinoma (ANHC). While numerous biomarkers have been evaluated, serum Midkine seems to be the most promising of all based on its diagnostic performance in the different studies. Given the inconsistencies among the available studies, we decided to resolve this with a meta-analysis. As demonstrated by the pooled results, serum Midkine (pooled AUC 0.91, sensitivity 76%, and specificity 85%) is an excellent biomarker for AFP-negative HCC diagnosis. MDK is a small heparin-binding protein that is highly secreted during fetal development. It is involved in promoting cellular proliferation, migration, and differentiation [31]. It is highly secreted in HCC, making it readily available for detection in either plasma or serum [32]. Using serum Midkine as a biomarker also has the advantage of being a less invasive test, that is well suited for mass surveillance and screening of AFP-negative HCC patients who usually tend to have better prognosis than their AFP-positive counterparts [33]. Economically, it is also much cheaper than the conventional radiology and pathology exams and will require less technical skills to perform.
In cancer surveillance and mass screening where serum biomarkers are well suited, Fiala et al. [34] argue that accuracy (AUC) may not be the best intention of a diagnostic test. Instead, higher sensitivity should be the priority as there are already more specific diagnostic tests such as radiology and pathology that can confirm cases picked up by the sensitive screening test. To this effect, the 76% pooled diagnostic sensitivity of Midkine although good is still low if Midkine is to be considered the best biomarker. Sensitivity is based on the diagnostic threshold, and different thresholds (threshold effect) could affect the pooled sensitivity in a diagnostic meta-analysis. However, we performed a Spearman correlation test for threshold effect and confirmed that there was no threshold effect in this study. In recent years, there has been a paradigm shift in exploring biomarkers for HCC and other cancers. Profiling a panel of biomarkers that complement each other as opposed to a single marker has been embraced as a method of improving diagnostic sensitivity, specificity, and accuracy of potential biomarkers, given the complex pathogenesis pathways exhibited by HCC and other cancers. In the same way, the other promising AFP-negative HCC biomarkers such as serum Osteopontin, DKK1, and other molecular markers could be assessed for synergy with Midkine to improve its sensitivity.
This systematic review and meta-analysis was a comprehensive update on the one done by Lu et al. [20] as a subgroup analysis in their study comparing the diagnostic accuracy of Midkine and AFP for detecting hepatocellular carcinoma. While the AUC remained almost the same, addition of more studies significantly reduced the sensitivity (88.5 vs 76%) and increased specificity (83.9 vs 85%) compared to what they reported. We believe that this update is a more accurate representation of the diagnostic performance of Midkine in AFP-negative HCC patients. The major limitation in this study was the average quality of the included studies which lowered the quality of the pooled evidence. Second, majority of the studies had significant design flaws as they were not originally designed for AFP-negative HCC diagnosis. Third, the overall sample size though powered just enough to meaningfully detect AFP-negative HCC was still low and so our result needs to be validated in a much larger cohort of AFP-negative HCC patients.
Conclusion
In summary, this meta-analysis assessed the diagnostic values of serum Midkine in AFP-negative HCC patients and demonstrated that serum Midkine is an excellent diagnostic biomarker for this subgroup of HCC, with a 76% sensitivity, 85% specificity, and 91% AUC. This result offer a strong basis for considering and validating serum Midkine as MDK as a diagnostic biomarker for AFP-negative HCC.
Availability of data and materials
All the data related to this work are in the manuscript.
References
Sia D, Villanueva A, Friedman SL, Llovet JM (2017) Liver cancer cell of origin, molecular class, and effects on patient prognosis. Gastroenterology 152(4):745–761
Siegel RL, Miller KD, Jemal A (2018) Cancer statistics, 2018. CA Cancer J Clin 68(1):7–30
Liu X, Li M, Wang X, Dang Z, Yu L, Wang X et al (2019) Effects of adjuvant traditional Chinese medicine therapy on long-term survival in patients with hepatocellular carcinoma. Phytomedicine 62:152930
Tsuchiya N, Sawada Y, Endo I, Saito K, Uemura Y, Nakatsura T. Biomarkers for the early diagnosis of hepatocellular carcinoma. World J Gastroenterol. 2015;21(37):10573–83. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4588079/. [Cited 2022 Sep 27]
Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V et al (2012) Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380(9859):2095–128. Available from: https://www.thelancet.com/article/S0140-6736(12)61728-0/fulltext. [Cited 2022 Sep 27]
Tanaka M, Katayama F, Kato H, Tanaka H, Wang J, Qiao YL et al (2011) Hepatitis B and C virus infection and hepatocellular carcinoma in China: a review of epidemiology and control measures. J Epidemiol 21(6):401–416
Yilmaz N, Yilmaz UE, Suer K, Goral V, Cakir N. Screening for hepatocellular carcinoma: summary of current guidelines up to 2018. Hepatoma Research. 2018;4:46. Available from: https://hrjournal.net/article/view/2745. [Cited 2022 Sep 27]
Gurakar A, Garonzik-Wang MMJ, Kim A, Anders RA, Oshima K, Georgiades C, et al. Clinicopathological distinction of low-AFP-secreting vs. high-AFP-secreting hepatocellular carcinomas. Ann Hepatol. 2019;17(6):1052–66. Available from: https://www.medigraphic.com/cgi-bin/new/resumenI.cgi?IDARTICULO=84257. [Cited 2022 Sep 27]
Liu Z, Pu Y, Bao Y, He S. Investigation of potential molecular biomarkers for diagnosis and prognosis of AFP-negative HCC. Int J Gen Med. 2021;14:4369–80. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8364386/. [Cited 2022 Sep 27]
Lu LH, Zhang YF, Wei W, Shi M, Guo RP (2017) Preoperative carbohydrate antigen 19–9: its neglected role in alpha-fetoprotein-negative hepatocellular carcinoma patients. J Gastrointest Surg 21(12):2025–2032
Jiang Y, Tie C, Wang Y, Bian D, Liu M, Wang T et al (2020) Upregulation of serum sphingosine (d18:1)-1-P potentially contributes to distinguish HCC including AFP-negative HCC from cirrhosis. Front Oncol 10:1759
European Association For The Study Of The Liver, European Organisation For Research And Treatment Of Cancer (2012) EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol 56(4):908–943
Bruix J, Sherman M, American Association for the Study of Liver Diseases (2011) Management of hepatocellular carcinoma: an update. Hepatology 53(3):1020–2
Zhu WW, Guo JJ, Guo L, Jia HL, Zhu M, Zhang JB et al (2013) Evaluation of midkine as a diagnostic serum biomarker in hepatocellular carcinoma. Clin Cancer Res 19(14):3944–3954
Muramatsu T, Kadomatsu K (2014) Midkine: an emerging target of drug development for treatment of multiple diseases. Br J Pharmacol 171(4):811–813
Mashaly AH, Anwar R, Ebrahim MA, Eissa LA, Shishtawy MME. Diagnostic and prognostic value of Talin-1 and Midkine as tumor markers in hepatocellular carcinoma in Egyptian patients. Asian Pac J Cancer Prev. 2018;19(6):1503–8. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6103586/. [Cited 2022 Sep 26]
Hodeib H, ELshora O, Selim A, Sabry NM, El Ashry HM (2017) Serum Midkine and osteopontin levels as diagnostic biomarkers of hepatocellular carcinoma. Electron Physician 9(1):3492–8
Vongsuvanh R, van der Poorten D, Iseli T, Strasser SI, McCaughan GW, George J (2016) Midkine increases diagnostic yield in AFP negative and NASH-related hepatocellular carcinoma. PLoS ONE 11(5):e0155800
Shaheen KYA, Abdel-Mageed AI, Safwat E, AlBreedy AM (2015) The value of serum midkine level in diagnosis of hepatocellular carcinoma. Int J Hepatol 2015:146389
Lu Q, Li J, Cao H, Lv C, Wang X, Cao S (2020) Comparison of diagnostic accuracy of Midkine and AFP for detecting hepatocellular carcinoma: a systematic review and meta-analysis. Biosci Rep 40(3):BSR20192424
Zheng L, Li H, Huang J, Shin J, Luo S, Guo C, et al. Serum midkine levels for the diagnosis and assessment of response to interventional therapy in patients with hepatocellular carcinoma. J Interv Med. 2020;4(1):39–45. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8562295/. [Cited 2022 Oct 21]
El-Shayeb AF, El-Habachi NM, Mansour AR, Zaghloul MS (2021) Serum midkine is a more sensitive predictor for hepatocellular carcinoma than Dickkopf-1 and alpha-L-fucosidase in cirrhotic HCV patients. Medicine (Baltimore) 100(17):e25112
Wang T, Zhang KH. New blood biomarkers for the diagnosis of AFP-negative hepatocellular carcinoma. Front Oncol. 2020;10:1316. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7456927/. [Cited 2022 Sep 27]
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;n71. Available from: https://www.bmj.com/lookup/doi/10.1136/bmj.n71. [Cited 2022 Apr 25]
Forner A, Reig M, Bruix J (2018) Hepatocellular carcinoma. Lancet 391(10127):1301–1314
Lo CKL, Mertz D, Loeb M (2014) Newcastle-Ottawa Scale: comparing reviewers’ to authors’ assessments. BMC Med Res Methodol 14(1):45. https://doi.org/10.1186/1471-2288-14-45. [Cited 2022 Sep 26]
Swets JA (1988) Measuring the accuracy of diagnostic systems. Science 240(4857):1285–93
Böhning D, Holling H, Böhning W, Sangnawakij P (2021) Investigating heterogeneity in meta-analysis of studies with rare events. Metron 79(3):259–72. https://doi.org/10.1007/s40300-021-00211-y. [Cited 2022 Aug 26]
Dalton JE, Bolen SD, Mascha EJ. Publication bias: the elephant in the review. Anesth Analg. 2016;123(4):812–3. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5482177/. [Cited 2022 Sep 26]
Chapter 8: meta-analysis of test performance when there is a “gold standard” | Effective Health Care (EHC) program. Available from: https://effectivehealthcare.ahrq.gov/products/methods-guidance-tests-metaanalysis/methods. [Cited 2022 Oct 21]
Ross-Munro E, Kwa F, Kreiner J, Khore M, Miller SL, Tolcos M, et al. Midkine: the who, what, where, and when of a promising neurotrophic therapy for perinatal brain injury. Frontiers in Neurology. 2020;11. Available from: https://www.frontiersin.org/articles/10.3389/fneur.2020.568814 [Cited 2022 Oct 6]
Gowhari Shabgah A, Ezzatifar F, Aravindhan S, Olegovna Zekiy A, Ahmadi M, Gheibihayat SM, et al. Shedding more light on the role of Midkine in hepatocellular carcinoma: new perspectives on diagnosis and therapy. IUBMB Life. 2021;73(4):659–69. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1002/iub.2458. [Cited 2022 Oct 6]
Wang X, Wang Q (2018) Alpha-fetoprotein and hepatocellular carcinoma immunity. Can J Gastroenterol Hepatol 2018:9049252
Fiala C, Diamandis EP. A multi-cancer detection test: focus on the positive predictive value. Annals of Oncology. 2020;31(9):1267–8. Available from: https://www.annalsofoncology.org/article/S0923-7534(20)39870-7/fulltext [Cited 2022 Oct 6]
Acknowledgements
Not applicable.
Funding
This study was supported by grants from Zhongnan Hospital of Wuhan University Science and Technology Innovation and Education Fund (Project cxpy2018067) and National Basic Research Program of China (973 program) (2012CB720605).
Author information
Authors and Affiliations
Contributions
Conception: Erick Thokerunga and Peter Kisembo. Interpretation or analysis of the data: Erick Thokerunga, Peter Kisembo, Huang FangFang. Preparation of the manuscript: Erick Thokerunga. Revision for important intellectual content: Kisembo Peter, Huang FangFang, Wang Zi, Zhang Yu, Christian Cedric Bongolo. Supervision: Jiancheng Tu. The authors read and approved the final manuscript.
Authors’ information
Not applicable.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Supplementary Table S1. Quality assessment of the included studies.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Thokerunga, E., Kisembo, P., FangFang, H. et al. Serum Midkine for AFP-negative hepatocellular carcinoma diagnosis: a systematic review and meta-analysis. Egypt Liver Journal 13, 25 (2023). https://doi.org/10.1186/s43066-023-00259-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43066-023-00259-7