Abstract
Background
Hepatic encephalopathy (HE) is a serious condition associated with high rates of mortality. Many scoring systems are used to predict the outcome of HE in patients admitted to the intensive care unit (ICU). The most used scores are Child-Turcotte-Pugh (CTP), Model for End-stage Liver Disease (MELD), Chronic Liver Failure-Sequential Organ Failure Assessment (CLIF-SOFA), and Acute Physiology and Chronic Health Evaluation II (APACHE II). These scores were thoroughly investigated in HE associated with acute liver failure (type A). In the present study, we aimed to evaluate the prognostic value of these scores in patients with HE on a background of liver cirrhosis (type C). Two hundred cirrhotic patients hospitalized with HE were included in the study. Diagnosis and classification of HE were based on the West Haven criteria. APACHE II, CLIF-SOFA, MELD, MELD-Na, and CTP scores were calculated for all patients within the first 24 h after admission. According to survival outcomes, patients were categorized into either improved or deceased. Demographic, clinical, and laboratory data as well as prognostic scores were compared in both deceased and improved groups. The receiver operating characteristic (ROC) curve was plotted, and the area under the ROC curve (AUROC) was calculated for each score. Backward logistic regression analysis was used to identify the predictors of mortality.
Results
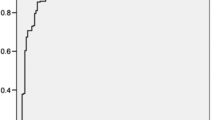
60.5% of patients were males. The mean age was 61.09 ± 8.94 years. The main precipitating factors of HE was infections predominantly spontaneous bacterial peritonitis (n = 108, 54.0%) followed by variceal bleeding (n = 39, 19.5%). All scores were significantly higher in the deceased patients. AUROC were 0.734 (CI95% 0.666–0.803), 0.717 (CI95% 0.647–0.787), 0.663 (CI95% 0.589–0.738), 0.626 (CI95% 0.549–0.704), and 0.609 (CI95% 0.531–0.686) for CLIF-SOFA, MELD-Na, MELD, APACHE II, and CTP scores, respectively. MELD, MELD-Na, and CLIF-SOFA scores were the independent predictors of mortality. Among these scores, CLIF-SOFA was the strongest independent predictor of mortality (OR = 1.142, CI95% = 0.888–1.467, p = 0.001).
Conclusions
CLIF-SOFA score was superior to other prognostic scores in predicting mortality in hospitalized patients with HE type C.
Similar content being viewed by others
Background
Hepatic encephalopathy (HE) is a brain dysfunction caused by impaired liver functions and/or portosystemic shunting [1]. It is one of the most serious complications of liver cirrhosis that leads to a significantly impaired quality of life and frequent hospitalizations [1]. The diagnosis of HE remains essentially clinical. HE is clinically manifested as disorientation, confusion, inappropriate behavior, agitation, somnolence, stupor, and/or frank coma. A wide range of motor dysfunctions has been described in HE, including asterixis, hypertonia, hyperreflexia, and/or extrapyramidal manifestations [2].
Although the clear pathogenesis of HE is not evident, some mechanisms caused by liver insufficiency are proposed. One of the suggested theories is that increased gamma amino butyric acid in the central nervous system leads to an increase in the neuronal inhibitory effect. Elevated arterial blood ammonia level is also considered an important underlying mechanism. It has been documented in about 90% of patients with HE. High arterial ammonia leads to impairment in mitochondrial functions with subsequent edema and swelling of the astrocytes. In addition, vasodilatation, caused principally by nitric oxide, could play a great part in the pathogenesis of HE as it leads to an increase in intracranial pressure, brain edema, and deterioration in cognitive functions [3].
HE is either associated with acute liver failure (type A), portosystemic bypass with no intrinsic hepatocellular disease (type B) or liver cirrhosis, and portal hypertension and/or portosystemic shunts (type C) [4].
HE is associated with a poor survival outcome and a high risk of in-hospital mortality [2]. This necessitated the development of a number of prognostic scoring systems to estimate the clinical outcome of HE in clinical practice. One of the most commonly used scores is the Child-Turcotte-Pugh score (CTP), a widely used system used to risk stratify cirrhotic patients [5]. The Acute Physiology and Chronic Health Evaluation (APACHE) II, a physiologically based prognostic system, is a widely used severity of illness scale used to predict hospital mortality in all ICU patients [5]. Sequential Organ Failure Assessment (SOFA) score has been developed and is basically used to assess and classify the variable degrees of organ dysfunction. It has been shown that a high SOFA score for any given organ is associated with significantly higher mortality [6]. The Model for End-Stage Liver Disease (MELD) is a widely used model for the risk stratification of short-term mortality in patients with cirrhosis [7]. These scores were thoroughly investigated in patients with HE associated with acute liver failure (type A HE). However, studies evaluating their prognostic yield in cirrhotic patients hospitalized with hepatic encephalopathy (type C HE) are lacking. In the present study, we aimed to evaluate the accuracy of different prognostic scoring systems in the prediction of in-hospital mortality of patients admitted to the ICU with HE on a previous background of liver cirrhosis.
Methods
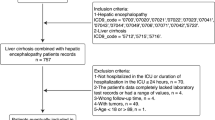
The current study was conducted on cirrhotic patients consecutively admitted to the ICU with hepatic encephalopathy at the National Liver Institute, Menoufia, Egypt, in the period between July 1 and December 31, 2020, after approval of the local ethical committee.
The diagnosis of cirrhosis was based on clinical, laboratory, and radiological findings. The West Haven criteria were used for the diagnosis and classification of HE [8]. Patients with acute hepatic failure and those with previous port-systemic shunt surgery or transjugular intrahepatic portosystemic shunt (TIPS) were ruled out. Patients with prior liver or other solid organ transplantation, end-stage renal disease and hepatocellular carcinoma (HCC), or other solid tumors were also excluded. Demographic data, baseline laboratory parameters, and duration of hospitalization were reported for all patients. The precipitating factors of HE were documented whenever they were identified. Patients were prospectively followed for in-hospital survival outcomes, whether they survived or died. A written informed consent was obtained from the patients’ relatives before inclusion.
Prognostic scores including CTP, MELD, MELD-Sodium (MELD-Na), APACHE II, and Chronic Liver Failure-SOFA (CLIF-SOFA) scores were calculated for all eligible patients within the first 24 h after admission to the ICU. Mortality was analyzed in view of each of these scores.
Statistical methods
Statistical analyses were performed using SPSS (Inc., Chicago, IL, version 20). Quantitative variables were expressed as mean and standard deviation (SD) while qualitative variables were expressed as frequency and percentage. The chi-square (χ2) test or Fisher exact test, when appropriate, were used for the comparison of qualitative variables between deceased patients and survivors. Continuous variables in both groups were compared using the paired t-test. In case of a skewed distribution, the Mann-Whitney U test was used for the comparison of continuous variables. The receiver operating characteristic (ROC) curve was plotted for each score, and the area under the ROC curve (AUROC) was calculated. High-risk variables that could be associated with mortality underwent backward logistic regression analysis. Variables that were statistically significant in the univariate analysis have been used in the multivariate analysis to estimate the independent predictors of mortality. Statistical significance was considered when the p value was lower than 0.05.
Results
A total of 200 patients out of 255 fulfilled the inclusion criteria and underwent the final analysis. Most of the patients were males (n = 121, 60.5%), with a mean age of 61.09 ± 8.94 years. The etiology of chronic liver disease was mainly hepatitis C virus (HCV) (n = 179, 89.5%). As regards the severity of liver cirrhosis, most of the patients were Child-Pugh class C (n = 161, 80.5%) while the rest of the patients were Child-Pugh class B (n = 39, 19.5%).
The precipitating factors of HE were infections and predominantly spontaneous bacterial peritonitis (SBP) (n = 108, 54.0%) followed by variceal bleeding (n = 39, 19.5%), excessive diuretics (n = 21, 10.5%), constipation (n = 18, 9.0%), and chest infection (n = 14, 7.0%).
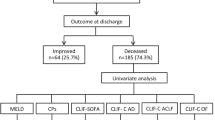
According to the West Haven grading system, 127 patients (63.5%) were hospitalized with HE grade II and 73 patients (36.5%) with HE grade III and IV. A total of 178 patients (89%) have experienced at least one previous episode of HE (recurrent HE) while 22 patients (11%) were admitted for the first episode of HE. The mortality rate was 49.5% (n = 99). The mean ICU stay was 6.53 ± 3.21 days. The basic patients’ demographic and laboratory data are summarized in Table 1.
Significantly lower values for all investigated scores have been demonstrated in improved patients as compared with deceased patients (Table 2). In comparison between both groups, the total ICU stay was significantly lower in improved than in deceased patients (p = 0.005).
After plotting the ROC curves (Fig. 1), the CLIF-SOFA score was the most accurate score in predicting mortality (AUROC = 0.734).
Comparison of ROC curves and AUROC values of CTP, MELD, APACHE II, and CLIF-SOFA scoring systems. ROC, receiver operating characteristic curve; AUROC, area under the ROC curve; CLIF-C, CTP, Child-Turcotte-Pugh; MELD, Model for End-stage Liver Disease; Na, sodium, CLIF-SOFA, Chronic Liver Failure-Sequential Organ Failure Assessment; APACHE II, Acute Physiology and Chronic Health Evaluation II
Factors associated with mortality in univariate analysis were higher INR, lower serum albumin, higher serum creatinine, lower serum sodium, longer ICU stay, higher grades of HE (grades III and IV), recurrent episodes of HE, and higher values of CTP, MELD, MELD-Na, APACHE II, and CLIF-SOFA scores (Table 4).
The independent predictors of mortality as indicated by multivariate analysis were lower serum sodium, higher grades of HE, and higher values of MELD, MELD-Na, and CLIF-SOFA scores. The strongest independent predictor of mortality was the CLIF-SOFA score (OR = 1.142, CI95% = 0.888–1.467, p = 0.001) (Table 4).
Discussion
Hepatic encephalopathy is one of the most common complications of cirrhosis, and it has been associated with a significant impact on patients’ health-related quality of life and survival, independent of the severity of cirrhosis [9].
In the current study, our aim was to verify the best scoring system for predicting survival outcomes in patients previously diagnosed with liver cirrhosis who were admitted to the ICU with hepatic encephalopathy, among various scoring systems used to evaluate the prognosis in acute liver failure.
Our results showed clearly that the CLIF-SOFA score is the most accurate scoring system in predicting prognosis, followed by MELD-Na, MELD, APACHE II, and CTP scores (Table 3 and Fig. 1). Furthermore, it has been shown that the CLIF-SOFA score is the strongest independent predictor of mortality among other scores (Table 4).
In the study by Elzouki et al., HCV was the most common cause of chronic liver disease (33.9%), while Zhang et al. found that hepatitis B virus (HBV) infection was the most common cause of chronic liver disease (54.5%) [10, 11]. Other authors, Moreau et al. and Dhiman et al., reported alcohol as the main cause of chronic liver disease (60% and 58%, respectively) [12, 13].
In the present study, the leading etiology of chronic liver disease was HCV (89.5%). This is because Egypt has the highest prevalence of HCV worldwide [14]. Also, the etiology of liver cirrhosis-related hepatic encephalopathy in these studies strongly followed the geographical prevalence of chronic liver disease in these countries. Alcoholic cirrhosis is the main underlying etiology in Western countries (50–70% of all causes), whereas viral hepatitis accounts for about 10–15% of all cases. In most Asian countries, HBV represents 70% and alcohol about 15% of all the etiologies [15,16,17,18].
All the investigated scores, including CLIF-SOFA, MELD, APACHE II, CTP, and MELD-Na, were significantly higher in the deceased patients as compared with the improved ones.
Essentially, these scores are widely used to predict prognosis in acute liver failure, and studies on their role in predicting mortality in HE type C are extremely limited. A recent study by Tas and colleagues includes 84 patients previously diagnosed with liver cirrhosis who were admitted to the ICU suffering from various grades of hepatic encephalopathy. After comparing CLIF-SOFA, APACHE II, CTP, and MELD scores as predictors of mortality, they found that the CLIF-SOFA score was superior to APACHE II, CTP, and MELD scores in predicting prognosis in such patients, AUROC values were 0.986 (0.970–1.003), 0.974 (0.945–1.003), 0.955 (0.915–0.996), and 0.880 (0.800–0.959), respectively. This is consistent with our results [19].
Elzouki et al. evaluated 109 patients diagnosed with decompensated liver cirrhosis and admitted to the ICU due to different etiologies; 24 patients (22%) were admitted with HE. Twenty-seven patients (25%) died, while 82 patients (75%) improved and were transferred to the ward. According to their findings, the SOFA score was the best prognostic model for predicting mortality in all age groups. Age above 60 years (p = 0.04), APACHE-II score (p = 0.001), and MELD score (p = 0.02) were the independent predicting factors for overall mortality. APACHE II and MELD scores accurately predicted mortality in patients over 60 years old (p = 0.001 and p = 0.02, respectively) [10].
Hemida et al. followed 60 patients with HCV-related liver cirrhosis who underwent non-liver surgery for 30 days after surgery. The MELD score was better than the CTP score in predicting 30-day mortality in these patients [20].
Dupont and colleagues studied the relationship between SOFA, MELD, and CTP scores and mortality in 281 cirrhotic patients admitted to the ICU. The mortality rate was 25.3%. SOFA, MELD, and CTP scores were significantly correlated with mortality. AUROC values for SOFA, MELD, and CTP were 0.82 (0.77–0.88), 0.81 (0.76–0.87), and 0.76 (0.70–0.82), respectively. SOFA and MELD scores were the strongest predictors of in-hospital mortality [21].
Pan and his colleagues [22] prospectively followed 250 critically ill cirrhotic patients admitted to the ICU and evaluated the 6-month mortality in those patients. They found that both CLIF-SOFA and APACHE III scores were excellent in predicting mortality in critically ill cirrhotic patients.
It has to be noted that CLIF-SOFA has the advantage of considering the functions of multiple vital organs, including liver (bilirubin and INR), brain (encephalopathy), kidney (creatinine), cardiovascular system (mean arterial blood pressure), and respiratory system (PaO2, FiO2). On the other hand, the conventional scores (MELD and CTP) neglect these functions that we believe are essential to be evaluated in critically ill patients admitted to the ICU. Our analysis confirmed this concept, where both MELD and CLIF-SOFA scores performed well and were independent predictors of mortality; however, CLIF-SOFA was superior to both MELD and MELD-Na scores. Meanwhile, the CTP score could not independently predict mortality in this context.
The main limitations of the current study were the relatively small sample size and the lack of comparator studies. However, the results obtained have important implications in clinical practice.
Conclusions
In conclusion, CLIF-SOFA has the highest performance among the studied scores in predicting mortality in cirrhotic patients hospitalized with HE.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ALP:
-
Alkaline phosphatase
- ALT:
-
Alanine aminotransferase
- APACHE II:
-
Acute Physiology and Chronic Health Evaluation
- AST:
-
Aspartate aminotransferase
- AUC:
-
Area under the ROC curve
- CLIF:
-
Chronic liver failure
- CTP:
-
Child-Turcotte-Pugh
- GGT:
-
Gamma glutamyl transferase
- HBV:
-
Hepatitis B virus
- HCC:
-
Hepatocellular carcinoma
- HCV:
-
Hepatitis C virus
- HE:
-
Hepatic encephalopathy
- ICU:
-
Intensive care unit
- INR:
-
International normalized ratio
- K:
-
Potassium
- MELD:
-
Model for End-Stage Liver Disease
- Na:
-
Sodium
- PLT:
-
Platelets
- ROC:
-
Receiver operating characteristic curve
- SBP:
-
Spontaneous bacterial peritonitis
- SOFA:
-
Sequential Organ Failure Assessment
- TIPS:
-
Transjugular intrahepatic portosystemic shunt
- WBCs:
-
White blood cells
References
European Association for the Study of the Liver (2014) Hepatic encephalopathy in chronic liver disease: 2014 practice guideline by the European Association for the Study of the liver and the American Association for the Study of Liver Diseases. J Hepatol 61(3):642–659
Kaplan PW, Rossetti AO (2011) EEG patterns and imaging correlations in encephalopathy: encephalopathy part II. J Clin Neurophysiol 28(3):233–251
Wijdicks EF (2016) Hepatic encephalopathy. N Engl J Med 375:1660–1670
Ferenci P, Lockwood A, Mullen K, Tarter R, Weissenborn K, Blei AT (2002) Hepatic encephalopathy—definition, nomenclature, diagnosis, and quantification: final report of the working party at the 11th world congresses of gastroenterology, Vienna, 1998. Hepatology 35:716–721
Knaus WA, Zimmerman JE, Wagner DP et al (1981) APACHE-acute physiology and chronic health evaluation: a physiologically based classification system. Crit Care Med 9:591–712
Vincent JL, Moreno R, Takala J et al (1996) The SOFA (sepsis-related organ failure assessment) score to describe organ dysfunction/failure. Intensive Care Med 22:707–710
Wiesner R, Edwards E, Freeman R et al (2003) Model for end-stage liver disease (MELD) and allocation of donor livers. Gastroenterology 124:91–96
Bajaj JS, Cordoba J, Mullen KD et al (2011) Review article: the design of clinical trials in hepatic encephalopathy - an International Society for Hepatic Encephalopathy and Nitrogen Metabolism (ISHEN) consensus statement. Aliment Pharmacol Ther 33:739–747
Patidar KR, Bajaj JS (2015) Covert and overt hepatic encephalopathy: diagnosis and management. Clin Gastroenterol Hepatol 13(12):2048–2061
Elzouki AN, Suliman S, Alhasan R, Abdullah A, Othman M, Badi A (2016) Predicting mortality of patients with cirrhosis admitted to medical intensive care unit: an experience of a single tertiary center. Arab J Gastroenterol 17:159–163
Zhang J, Ye L, Zhang J et al (2015) MELD scores and child-Pugh classifications predict the outcomes of ERCP in cirrhotic patients with choledocholitiasis: a retrospective cohort study. Medicine (Baltimore) 94:e433
Dhiman RK, Agrawal S, Gupta T, Duseja A, Chawla Y (2014) Chronic liver failure-sequential organ failure assessment is better than the Asia-Pacific Association for the Study of liver criteria for defining acute-on-chronic liver failure and predicting outcome. World J Gastroenterol: WJG 20(40):14934
Moreau R, Jalan R, Gines P et al (2013) Acute-on-chronic liver failure is a distinct syndrome that develops in patients with acute decompensation of cirrhosis. Gastroenterology 144:1426–1437
Gomaa A, Allam N, Elsharkawy A, El Kassas M, Waked I (2017) Hepatitis C infection in Egypt: prevalence, impact and management strategies. Hepat Med 9:17–25
Mann RE, Smart RG, Govoni R (2003) The epidemiology of alcoholic liver disease. Alcohol Res Health 27(3):209–219
Lucey MR, Mathurin P et al (2009) Alcoholic hepatitis. N Engl J Med 360:2758–2769
Louvet A, Mathurin P (2015) Alcoholic liver disease: mechanisms of injury and targeted treatment. Nat Rev Gastroenterol Hepatol 12:231–242
Custer B, Sullivan SD, Hazlet TK, Iloeje U, Veenstra DL, Kowdley KV (2004) Global epidemiology of hepatitis B virus. J Clin Gastroenterol 38(10 Suppl 3):S158–S168
Taş A, Yalçın MS, Sarıtaş B, Kara B (2018) Comparison of prognostic systems in cirrhotic patients with hepatic encephalopathy. Turk J Med Sci 48(3):543–547. https://doi.org/10.3906/sag-1709-32 PMID: 29914250
Hemida K, Al Swaff RE, Shabana SS, Said H, Ali-Eldin F (2016) Prediction of post-operative mortality in patients with HCV related cirrhosis undergoing non-hepatic surgeries. J Clin Diagn Res 10:OC18–OC21
Dupont B, Delvincourt M, Koné M et al (2015) Retrospective evaluation of prognostic score performances in cirrhotic patients admitted to an intermediate care unit. Dig Liver Dis 47:675–681
Pan HC, Jenq CC, Tsai MH et al (2014) Scoring systems for 6-month mortality in critically ill cirrhotic patients: a prospective analysis of chronic liver failure–sequential organ failure assessment score (CLIF-SOFA). Aliment Pharmacol Ther 40(9):1056–1065
Acknowledgements
The authors would like to acknowledge all individuals working in the ICU, National Liver Institute, Menoufia University, for their help and support in achieving this research.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
AM, ZH, and ZT put the conception and study design. RM and EM were assigned to the data collection and processing. ZH and AM contributed to the data analysis and interpretation. EM and RM prepared the literature review. ZT wrote the manuscript. ZH and AM revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the local Institutional Review Board of National Liver Institute, Menoufia University, Egypt. A signed written informed consent was obtained from all patients’ relatives before participation in the study.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Abbasy, M., Zaghla, H., Elhelbawy, M. et al. Predicting in-hospital mortality of cirrhotic patients hospitalized with hepatic encephalopathy. Egypt Liver Journal 12, 13 (2022). https://doi.org/10.1186/s43066-022-00178-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43066-022-00178-z