Abstract
Background
Considerable disparities in chronic pain management have been identified. Persons in rural, lower income, and minoritized communities are less likely to receive evidence-based, nonpharmacologic care. Telehealth delivery of nonpharmacologic, evidence-based interventions for persons with chronic pain is a promising strategy to lessen disparities, but implementation comes with many challenges. The BeatPain Utah study is a hybrid type 1 effectiveness-implementation pragmatic clinical trial investigating telehealth strategies to provide nonpharmacologic care from physical therapists to persons with chronic back pain receiving care in ommunity health centers (CHCs). CHCs provide primary care to all persons regardless of ability to pay. This paper outlines the use of implementation mapping to develop a multifaceted implementation plan for the BeatPain study.
Methods
During a planning year for the BeatPain trial, we developed a comprehensive logic model including the five-step implementation mapping process informed by additional frameworks and theories. The five iterative implementation mapping steps were addressed in the planning year: (1) conduct needs assessments for involved groups; (2) identify implementation outcomes, performance objectives, and determinants; (3) select implementation strategies; (4) produce implementation protocols and materials; and (5) evaluate implementation outcomes.
Results
CHC leadership/providers, patients, and physical therapists were identified as involved groups. Barriers and assets were identified across groups which informed identification of performance objectives necessary to implement two key processes: (1) electronic referral of patients with back pain in CHC clinics to the BeatPain team and (2) connecting patients with physical therapists providing telehealth. Determinants of the performance objectives for each group informed our choice of implementation strategies which focused on training, education, clinician support, and tailoring physical therapy interventions for telehealth delivery and cultural competency. We selected implementation outcomes for the BeatPain trial to evaluate the success of our implementation strategies.
Conclusions
Implementation mapping provided a comprehensive and systematic approach to develop an implementation plan during the planning phase for our ongoing hybrid effectiveness-implementation trial. We will be able to evaluate the implementation strategies used in the BeatPain Utah study to inform future efforts to implement telehealth delivery of evidence-based pain care in CHCs and other settings.
Trial registration
ClinicalTrials.gov Identifier: NCT04923334. Registered June 11, 2021.
Similar content being viewed by others
Introduction
One in 5 Americans live with chronic pain [1]. Back pain is the most prevalent form of chronic pain [2]. Evidence-based interventions (EBIs) for chronic low back pain (LBP) include nonpharmacologic treatments provided by physical therapists (PTs) and others [3, 4]. Guidelines advise against opioids [5,6,7], yet evidence-practice gaps persist. Among persons with LBP, rates of opioid prescribing are about double rates of nonpharmacologic care [8,9,10,11,12,13,14].
Considerable disparities exist in chronic pain prevalence and management. Prevalence is higher among persons with less income or education and in rural communities [15, 16]. These individuals are more likely to receive opioids [17,18,19] and less likely to receive nonpharmacologic care [20, 21]. Many persons with these characteristics receive primary care in community health centers (CHCs) [22,23,24], yet geographic and other barriers limit access to nonpharmacologic care [23]. About a third of CHC patients are Latino/a, introducing additional barriers related to language and sociocultural fit [25, 26]. Collectively, these barriers contribute to pain disparities [27].
Telehealth delivery of nonpharmacologic care could lessen disparities [28], but application has been limited [29, 30]. Experiences during COVID support telehealth’s potential to increase access [31], but issues specific to implementation in underserved communities must be considered [32]. Implementation mapping (IM) is a systematic approach to iteratively develop scalable and sustainable EBI implementation strategies [33, 34]. This paper describes application of IM in the BeatPain Utah study examining telehealth EBIs for patients with chronic LBP in CHCs.
Methods
BeatPain Utah study
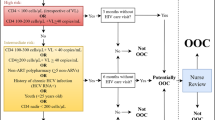
BeatPain Utah (Fig. 1) (ClinicalTrials.gov Identifier: NCT04923334) is a pragmatic clinical trial examining two PT-led telehealth EBIs, a brief consult and an extended PT program, delivered across two treatment phases. Further details are published [35]. BeatPain is a hybrid type 1 trial, primarily focusing on effectiveness and secondarily on implementation outcomes [36]. Implementation mapping occurred during a planning year before enrollment. The implementation strategies developed are being evaluated as part of the ongoing hybrid clinical trial. Planning activities, including community-member interviews, were approved by the University of Utah Institutional Review Board.
BeatPain Utah is being conducted in nine CHC organizations in Utah serving urban and rural communities. Among persons served by these clinics, approximately 49% identify as Hispanic/Latino/a, 37% are non-English speakers, 45% are uninsured, and 59% are below the federal poverty level [37]. Patients in CHC clinics are referred to BeatPain through standards-based, HIPAA-compliant electronic referral (e-referral) from a CHC EHR using phiMail® (EMR Direct, Inc., San Diego, CA, USA). Once an e-referral is received, a BeatPain team member contacts the patient. Patients opting to enroll provide oral consent. Those choosing not to participate or ineligible are offered care without study data collection.
Implementation logic model
Implementation mapping was informed by additional frameworks to develop a logic model (Fig. 2). The Consolidated Framework for Implementation Research (CFIR) helped identify contextual factors across five domains that could influence e-referral and telehealth implementation: the innovation being implemented, outer setting, inner setting, individuals involved, and the implementation process. Social-cognitive theory (SCT) emphasizes factors influencing behavior including the following: (1) environmental factors (e.g., social support, cultural context); (2) cognitive factors (e.g., knowledge, self-efficacy); and (3) behavioral factors (e.g., coping strategies, outcome expectancies) [38]. Proctor’s taxonomy of Outcomes for Implementation Research [39], informed IM step 5.
Implementation mapping
Implementation mapping was based on a five-step model [33] detailed below and depicted in Fig. 2.
Step 1 — Needs assessment
Step 1 identified barriers and facilitators using needs assessment for groups involved in implementation including patients, CHC leadership/providers, and PTs [40, 41]. For CHC leadership/providers, needs assessments were conducted using zoom due to COVID restrictions. Assessments focused on the existing and desired clinic workflows for identifying and treating individuals with LBP, and the type of feedback desired about referred patients. The goal was collection of data to inform e-referral implementation [42, 43]. For patients, we conducted individual, zoom interviews with individuals with LBP in communities served by CHC clinics identified by working with community organization and clinic representatives. Interviews used an ethnographic approach focused on persons’ lived experience including their understanding of LBP and healthcare experiences using questions described by Blumenthal and colleagues [44]. Participant responses were noted in a REDCap. Needs assessments for PTs about telehealth implementation were conducted in group zoom meetings.
Step 2 — Identify implementation outcomes, performance objectives, and determinants
Step 2 used step 1 findings to identify implementation outcomes and performance objectives for each group. Implementation outcomes identified behavior goals. Performance objectives identified tasks required to achieve an implementation outcome. Next, determinants were specified, informed by step 1 findings and the SCT framework [45]. Determinants are modifiable, internal factors helping explain why persons would achieve a performance objective [46]. For example, self -efficacy is an important determinant of behavior change and relates to one’s beliefs in their capacity to perform an action and persist despite barriers [38]. Another behavior change determinant is outcomes expectancy, i.e., is the belief that performing an action will lead to a particular outcome, and is another behavior change determinant [47].
Step 3 — Select implementation strategies
In step 3, methods or processes that can change a determinant based on evidence or theory (e.g., increase knowledge, change attitudes) [48] were selected. Methods informed the choice of implementation strategies. Strategies [49] were then operationalized as practical applications that fit within the context described by CFIR and the needs assessments [46].
Step 4 — Create implementation protocols
Step 4 operationalized implementation strategies by producing protocols and materials for training and delivery.
Step 5 — Evaluate implementation outcomes
Step 5 developed a plan to evaluate outcomes of the implementation processes during the BeatPain study. Outcomes were based on Proctor’s taxonomy [39] and included acceptability, adoption, feasibility, and fidelity.
Results
Step 1 — Needs assessment
Needs assessment outcomes are described in Table 1. Assessments were conducted with CHC leaders/providers from seven organizations. Participants expressed receptivity to PT-led telehealth. Facilitators included the ability to accommodate patients in Spanish or English, without cost, and receiving feedback about referred patients. Potential barriers centered on EHR capabilities for making e-referrals, time constraints and competing demands, and integrating a new workflow, particularly in light of COVID impacts on clinic operations.
We interviewed five female patients with LBP, each of whom identified as Hispanic/Latina. Three preferred communications in Spanish and two in English. Facilitators identified included positive experiences and trust in CHCs and availability of cell phones for telehealth. Barriers included lack of reliable Internet and technology for video telehealth sessions. There was a general lack of awareness that PT could be provided by telehealth, and that it may be beneficial. Some interviewees expressed preferences for passive pain coping, including medication or rest, which are not EBIs.
Facilitators for PTs included commitment to providing care to persons in historically marginalized communities. Most were bilingual, and some had experience providing PT with Spanish-speaking patients. Barriers included lack of telehealth experience, the need to adapt treatments for phone-only and video telehealth delivery, and ability to engage and motivate patients using telehealth.
Step 2 — Identify implementation outcomes, performance objectives, and determinants
We identified implementation outcomes as participating in BeatPain and referring persons with LBP for CHC leadership/providers, engaging in telehealth for patients, and providing telehealth with fidelity to intervention core components for PTs. Performance objectives derived from these outcomes, and associated determinants are outlined in Table 2.
Determinants informed our choice of implementation strategies to help each group achieve their performance objectives. For CHC leadership/providers, we identified knowledge of nonpharmacologic pain care and expectations for telehealth PT as determinants of agreeing to participate and place e-referrals. The ability to provide technical support for the implementation of e-referrals within clinic EHRs and avoid workflow disruptions was determinants of sustainment of e-referrals. For patients, we considered knowledge and outcomes expectancy for telehealth PT as determinants for engaging in BeatPain. Determinants for PTs included knowledge of how to deliver the BeatPain intervention core components using telehealth and self-efficacy to engage patients who may have different cultural backgrounds.
Step 3 — Select implementation strategies
Implementation methods relevant across groups included increasing knowledge, changing awareness, changing attitudes and beliefs, and developing skills, capabilities and self-efficacy, and outcome expectations [48]. We matched these methods to implementation strategies (Table 2).
Implementation strategies for CHC leadership/providers included education about nonpharmacologic LBP care and the BeatPain program and training on how to explain BeatPain to patients to increase self-efficacy for referring patients. Additional implementation strategies included hands-on technical support to implement e-referrals within each clinic’s EHR (three different EHR products are used across organizations) and provide ongoing technical support. We used a secure, EHR-based process designed to be minimally disruptive to existing workflows. We chose secure messaging based on the direct standard protocol using phiMail because this approach was HIPAA compliant, standards-based, inexpensive, and bidirectional. Since the Direct Protocol is required for EHR certification, it was supported by all EHR systems used in Utah CHC clinics [50]. This strategy also provided the infrastructure for PTs to return feedback to providers on patients’ status, helping to build positive expectations about BeatPain.
Although in-clinic e-referrals are minimally disruptive, they require clinician recall during a visit. We therefore included a second implementation strategy using text messaging to capture individuals for whom a referral may have been unaddressed during the visit. We used a population health management system (Azara Healthcare, Burlington, MA, USA) that interfaces with clinic EHRs and identifies eligible patients (recent appointment for LBP) and then automatically sends a bidirectional text message introducing the BeatPain project and offering a connection to telehealth. Patients who respond positively are noted on an electronic dashboard, and clinic staff can place an e-referral.
Implementation strategies for patients focused on engagement to build positive expectancies for telehealth PT. Explanations used by BeatPain personnel to describe the program to patients and patient-facing materials such as the project’s webpage were tailored to provide information on what telehealth PT involves and its potential benefits. Additionally, a strategy of adapting and tailoring telehealth PT interventions addressed the determinant of building patient self-efficacy for active pain coping. Telehealth PT interventions were adapted to include a motivation-and-problem-solving (MAPS) approach found effective for chronic care management and substance use treatment [51]. The MAPS approach is appropriate for persons irrespective of their readiness to change and explicitly targets motivation and self-efficacy as behavior change mechanisms [52, 53].
Physical therapist implementation strategies included training and education on providing care using telehealth, especially when communication is audio-only. Training included didactic information, role-playing, ongoing weekly discussions, and peer practice. Integration of mHealth resources including app-based exercise and education platforms helped support patients’ self-management. Physical therapists were trained in MAPS using didactic and interactive strategies to build self-efficacy for delivering the BeatPain core components. MAPS includes motivational interviewing and cognitive behavioral techniques that help patients set personalized goals and manage barriers towards achieving these goals [51]. To further build self-efficacy, the MAPS expert on the BeatPain team provided coaching through role-playing a PT session and providing feedback. Physical therapists were also trained on culturally competent care to meet patients’ sociocultural and linguistic needs [54].
Step 4 — Create implementation protocols
Step 4 operationalized implementation strategies. For CHC leadership/providers, we developed brief (10–15 min) presentations, and for in-person or remote delivery, focused on evidence supporting nonpharmacologic care and the BeatPain program. Detailed instructions for placing e-referrals in the clinic’s EHR were provided along with suggested language providers could use to describe BeatPain to patients. Ongoing updates were provided during staff meetings, including reminders on e-referral procedures, troubleshooting barriers, and anecdotal patient experiences.
We operationalized patient implementation strategies by developing a study webpage, in English and Spanish, accessible through a QR code on recruitment materials, to describe BeatPain and build positive expectations (https://health.utah.edu/physical-therapy-athletic-training/research/clinical-outcomes-researh/beatpain-utah/eng). The webpage described the partnership between BeatPain and CHC clinics, gave biographies of BeatPain personnel, and described telehealth PT treatment. We used the MedBridge phone app (MedBridge, Inc., Bellevue, WA, USA) to provide exercise and education videos.
Physical therapist training focused on the intervention core components and integration of MAPS for English- and Spanish-speaking patients [35]. Training in culturally competent care used Hays ADDRESSING framework as a structured self-exploration method of how the PT’s cultural background may interact with their patient’s background and influence care [55]. We also used Betancourt’s framework for cross-cultural communication to help PTs consider major cultural issues they may encounter and provide person-centered care characterized by empathy and respect for patients’ values and preferences [56].
Step 5 — Evaluate implementation outcomes
Implementation outcomes for the BeatPain trial [35] were selected to evaluate the success of the IM process across groups. Because BeatPain adapted nonpharmacologic pain EBIs for underrepresented populations using novel delivery strategies, we identified important implementation outcomes as adoption, acceptability, feasibility, and fidelity as defined in Table 3.
Discussion
Implementing telehealth pain care in CHCs creates an opportunity to increase the reach of EBIs and reduce pain management disparities. BeatPain Utah uses an e-referral process of persons with LBP from CHC clinics to a centralized telehealth PT team, requiring behavior changes and new work processes for clinical teams, patients, and PTs. The five-step IM process informed by additional models helped us to understand needs and assets for CHC leadership/providers, patients, and PTs, identify actions necessary to achieve implementation outcomes, identify determinants of those actions, and operationalize implementation strategies to address key determinants. Through this process, we developed a multifaceted implementation plan to connect patients with telehealth EBIs. The final IM step identified implementation outcomes for the hybrid effectiveness-implementation study.
We identified knowledge and positive expectations around nonpharmacologic pain care, EHR support for placing e-referrals, and minimizing workflow disruptions as important determinants of e-referrals from CHC clinics, consistent with other findings that technology challenges and workflow disruptions are barriers to e-referral implementation and sustainment [57]. These determinants were influenced by COVID impacts on staffing and the varied EHR systems used within clinics. We used brief, intermittent trainings on the e-referral process, ongoing EHR support, and a secondary text message recruitment approach as strategies to address these determinants. Lack of knowledge and uncertain expectations for telehealth PT were not surprising given limited exposure to nonpharmacologic EBIs or telehealth PT in CHCs [20, 23, 58] but could adversely impact providers’ self-efficacy for advising patients with LBP about BeatPain. Educating providers and sending feedback on referred patients addressed these concerns.
Patient needs assessments reflected uncertainty that telehealth PT is equivalent to in-person care, consistent with other reports [59, 60]. Also, studies during COVID reported persons of Hispanic ethnicity expressed less willingness to use telehealth [61, 62]. We therefore considered positive expectations about telehealth PT, a determinant of patients’ attendance, which we addressed by emphasizing the personalized nature of telehealth and ability to individualize care in patient-facing materials. Some patients expressed preferences for passive coping strategies that are associated with lower self-efficacy for engaging in active EBIs such as physical activity [63]. Developing self-efficacy for active coping had to balance recognition that preferences can reflect cultural norms and individual experiences [64,65,66]. We addressed this through training PTs in cross-cultural communication emphasizing the patient as teacher and strategies to negotiate differences in a patient-centered manner [56, 67].
Like most PTs, BeatPain therapists had limited telehealth experience [68]. Thus, building PTs’ self-efficacy to deliver telehealth care and build effective patient-therapist relationships, particularly with phone-only communication, was a key determinant. We trained PTs in MAPS which combines motivational interviewing and cognitive behavioral techniques to help patients set and achieve personally meaningful goals [51]. Motivational interviewing is a person-centered communication strategy well-suited to phone delivery [69,70,71] and circumstances where the patient and PT have different cultural backgrounds [72, 73], possibly due to motivational interviewing’s collaborative, nonjudgmental nature which may reduce risks for implicit biases by providers [74].
There are important limitations to note in our IM process. We did not pilot our implementation strategies or resources before beginning our hybrid clinical trial. As a hybrid trial, a secondary goal of the BeatPain study is the evaluate implementation. We intended to conduct needs assessments and patient interviews in-person, but COVID restrictions necessitated using zoom instead.
Conclusion
BeatPain Utah is a hybrid type I trial evaluating effectiveness and implementation outcomes [36]. IM provided a systematic, theory-driven process to develop and evaluate implementation strategies. Assessment of implementation outcomes will allow us to evaluate the success of our implementation strategies for future trials and clinical applications.
Availability of data and materials
Not applicable.
Abbreviations
- CFIR:
-
Consolidated Framework for Implementation
- CHC:
-
Community health center
- EBI:
-
Evidence-based intervention
- EHR:
-
Electronic health record
- IM:
-
Implementation mapping
- LBP:
-
Low back pain
- MAPS:
-
Motivation and problem-solving
- PT:
-
Physical therapist
- SCT:
-
Social cognitive theory
References
Institute of Medicine (US) Committee on Advancing Pain Research, Care, and Education. Relieving pain in America: a blueprint for transforming prevention, care, education, and research. Washington: National Academies Press (US); 2011.
Dieleman JL, Cao J, Chapin A, et al. US health care spending by payer and health condition, 1996–2016. JAMA. 2020;323(9):863–84.
Chou R, Deyo R, Friedly J, Skelly A, Hashimoto R, Weimer M, et al. Noninvasive treatments for low back pain. Comparative effectiveness review No. 169. (Prepared by the Pacific Northwest evidence-based practice center under contract No. 290–2012–00014-I.). Rockville: Agency for Healthcare Research and Quality; 2016.
Chou R, Deyo R, Friedly J, Skelly A, Hashimoto R, Weimer M, et al. Nonpharmacologic therapies for low back pain: systematic review for an American College of Physicians clinical practice guideline. Ann Intern Med. 2017;166(7):493–505.
Dowell D, Haegerich TM, Chou R. CDC guidelines for prescribing opioids for chronic pain - United States, 2016. JAMA. 2016;315(15):1624–45.
Pangarkar SS, Kang DG, Sandbrink F, Bevevino A, Tillisch K, Konitzer L, et al. VA/DoD clinical practice guideline: diagnosis and treatment of low back pain. J Gen Intern Med. 2019;34:2620–9.
Corp N, Mansell G, Stynes S, Wynne-Jones G, Morsø L, Hill JC, et al. Evidence-based treatment recommendations for neck and low back pain across Europe: a systematic review of guidelines. Eur J Pain. 2021;25(2):275–95.
Mikosz CA, Zhang K, Haegerich T, Xu L, Losby JL, Greenspan A, et al. Indication-specific opioid prescribing for US patients with Medicaid or private insurance, 2017. JAMA Netw Open. 2020;3(5):e204514.
Goldstick JE, Guy GP, Losby JL, Baldwin G, Myers M, Bohnert ASB. Changes in initial opioid prescribing practices after the 2016 release of the CDC guideline for prescribing opioids for chronic pain. JAMA Netw Open. 2021;4(7):e2116860.
Raad M, Pakpoor J, Harris AB, Puvanesarajah V, Marrache M, Canner JK, et al. Opioid prescriptions for new low back pain: trends and variability by state. J Am Board Fam Med. 2020;33(1):138–42.
Frogner BK, Harwood K, Andrilla HA, Schwartz M, Pines JM. Physical therapy as the first point of care to treat low back pain: an instrumental variables approach to estimate impact on opioid prescription, health care utilization, and costs. Health Serv Res. 2018;53(6):4629–46.
Feldman DE, Carlesso LC, Nahin RL. Management of patients with a musculoskeletal pain condition that is likely chronic: results from a national cross sectional survey. J Pain. 2020;21(7–8):869–80.
Marrache M, Prasad N, Margalit A, Nayar SK, Best MJ, Fritz JM, et al. Initial presentation for acute low back pain: is early physical therapy associated with healthcare utilization and spending? A retrospective review of a National Database. BMC Health Serv Res. 2022;22(1):851.
Salt E, Gokun Y, Rankin Kerr A, Talbert J. A description and comparison of treatments for low back pain in the United States. Orthoped Nurs. 2016;35(4):214–21.
Dahlhamer J, Lucas J, Zelaya C, Nahin R, Mackey S, DeBar L, et al. Prevalence of chronic pain and high-impact chronic pain among adults - United States, 2016. MMWR Morb Mortal Wkly Rep. 2018;67(36):1001–6.
Janevic MR, McLaughlin SJ, Heapy AA, Thacker C, Piette JD. Racial and socioeconomic disparities in disabling chronic pain: findings from the health and retirement study. J Pain. 2017;18(12):1459–67.
Booher L. The impact of low socioeconomic status in adults with chronic pain: an integrative review. Orthoped Nurs. 2019;38(6):381–9.
Gebauer S, Salas J, Scherrer JF. Neighborhood socioeconomic status and receipt of opioid medication for new back pain diagnosis. J Am Board Fam Med. 2017;30(6):775–83.
Prunuske JP, St Hill CA, Hager KD, Lemieux AM, Swanoski MT, Anderson GW, et al. Opioid prescribing patterns for non-malignant chronic pain for rural versus non-rural US adults: a population-based study using 2010 NAMCS data. BMC Health Serv Res. 2014;14:563.
Eaton LH, Langford DJ, Meins AR, Rue T, Tauben DJ, Doorenbos AZ. Use of self-management interventions for chronic pain management: a comparison between rural and nonrural residents. Pain Manag Nurs. 2018;19(1):8–13.
Garcia MC, Heilig CM, Lee SH, Faul M, Guy G, Iademarco MF, et al. Opioid prescribing rates in nonmetropolitan and metropolitan counties among primary care providers using an electronic health record system - United States, 2014–2017. MMWR Morb Mortal Wkly Rep. 2019;68(2):25–30.
Health Center Program: impact and growth. https://bphc.hrsa.gov/sites/default/files/bphc/about/healthcenterfactsheet.pdf. Accessed 17 June 2023.
Anderson D, Wang S, Zlateva I. Comprehensive assessment of chronic pain management in primary care: a first phase of a quality improvement initiative at a multisite community health center. Qual Prim Care. 2012;20(6):421–33.
Smith LJ, Johnson-Lawrence V, Andrews M, Parker S. Opportunity for interprofessional collaborative care - findings from a sample of federally qualified health center patients in the Midwest. Public Health. 2017;151:131–6.
Hollingshead NA, Ashburn-Nardo L, Stewart JC, Hirsh AT. The pain experience of Hispanic Americans: a critical literature review and conceptual model. J Pain. 2016;17(5):513–28.
Zvolensky MJ, Smit T, Rogers AH, Matoska C, Garey L, Viana AG, et al. Exploring pain experience and anxiety sensitivity among Latinx adults in a federally qualified health center. J Behav Med. 2022;45(3):404–15.
Anderson DR, Zlateva I, Coman EN, Khatri K, Tian T, Kerns RD. Improving pain care through implementation of the stepped care model at a multisite community health center. J Pain Res. 2016;9:1021–9.
DeMonte CM, DeMonte WD, Thorn BE. Future implications of eHealth interventions for chronic pain management in underserved populations. Pain Manag. 2015;5(3):207–14.
Greenberg AJ, Haney D, Blake KD, Moser RP, Hesse BW. Differences in access to and use of electronic personal health information between rural and urban residents in the United States. J Rural Health. 2018;34(Suppl 1):s30–8.
Spooner KK, Salemi JL, Salihu HM, Zoorob RJ. eHealth patient-provider communication in the United States: interest, inequalities, and predictors. J Am Med Inform Assoc. 2017;24(e1):e18–27.
Adepoju OE, Chae M, Ojinnaka CO, Shetty S, Angelocci T. Utilization gaps during the COVID-19 pandemic: racial and ethnic disparities in telemedicine uptake in Federally Qualified Health Center clinics. J Gen Intern Med. 2022;37(5):1191–7.
Fritz JM, Davis AF, Burgess DJ, et al. Pivoting to virtual delivery for managing chronic pain with nonpharmacological treatments: implications for pragmatic research. Pain. 2021;62(6):1591–6.
Fernandez ME, Ten Hoor GA, van Lieshout S, Rodriguez SA, Beidas RS, Parcel G, et al. Implementation mapping: using intervention mapping to develop implementation strategies. Front Public Health. 2019;7:158.
Bastian LA, Cohen SP, Katsovich L, Becker WC, Brummett BR, Burgess DJ, et al. Stakeholder engagement in pragmatic clinical trials: emphasizing relationships to improve pain management delivery and outcomes. Pain Med. 2020;21(Suppl 2):S13-s20.
Fritz JM, Del Fiol G, Gibson B, Wetter DW, Solis V, Bennett E, et al. BeatPain Utah: study protocol for a pragmatic randomised trial examining telehealth strategies to provide non-pharmacologic pain care for persons with chronic low back pain receiving care in Federally Qualified Health Centers. BMJ Open. 2022;12(11):e067732.
Curran GM, Bauer M, Mittman B, Pyne JM, Stetler C. Effectiveness-implementation hybrid designs: combining elements of clinical effectiveness and implementation research to enhance public health impact. Med Care. 2012;50(3):217–26.
Association for Utah Community Health. Utah Community Health Centers 2021/2022 Overview. https://auch.org/2022overview. Published 2020. Accessed 20 June 2023.
Bandura A. Self-efficacy: the exercise of control. New York: WH Freeman and Company; 1997.
Proctor E, Silmere H, Raghavan R, Hovmand P, Aarons G, Bunger A, et al. Outcomes for implementation research: conceptual distinctions, measurement challenges and research agenda. Adm Policy Ment Health. 2011;38:65–76.
Rolland B, Resnik F, Hohl SD, Johnson LJ, Saha-Muldowney M, Mahoney J. Applying the lessons of implementation science to maximize feasibility and usability in team science intervention development. J Clin Transl Sci. 2021;5(1):e197.
Damschroder LJ, Reardon CM, Widerquist MAO, Lowery J. The updated Consolidated Framework for Implementation Research based on user feedback. Implement Sci. 2022;17(1):75.
Berg M, Aarts J, van der Lei J. ICT in health care: sociotechnical approaches. Methods Inf Med. 2003;42(4):297–301.
Gibson B, Kramer H, Weir C, Fiol G, Borbolla D, Schlechter CR, et al. Workflow analysis for design of an electronic health record-based tobacco cessation intervention in community health centers. JAMIA Open. 2021;4(3):ooaa070.
Blumenthal K, Schlotterback B, Oliver JG, Abrew K, Fritz J. Chronic low back pain experiences of low-income immigrants in a Hispanic community in Midvale, Utah and their relevance to physical therapist practice. PTJ-PAL. 2018;18(2):5–14.
Bandura A. Health promotion by social cognitive means. Health Ed Behav. 2004;31(2):143–64.
Bartholomew LK, Markham CM, Ruiter RAC, Fernandez ME, Kok G, Parcel GS. Planning health promotion programs: an intervention mapping approach. 4th ed. San Francisco: Jossey-Bass; 2016.
Luszczynska A, Schwarzer R. Changing Behavior Using Social Cognitive Theory. In: Hamilton K, Cameron LD, Hagger MS, Hankonen N, Lintunen T, editors. The Handbook of Behavior Change. Cambridge: Cambridge University Press; 2020. p. 32–45.
Kok G, Gottlieb NH, Peters GY, Mullen PD, Parcel GS, Ruiter RAC, et al. A taxonomy of behaviour change methods: an intervention mapping approach. Health Psychol Rev. 2016;10(3):297–312.
Waltz TJ, Powell BJ, Matthieu MM, Damschroder LJ, Chinman MJ, Smith JL, et al. Use of concept mapping to characterize relationships among implementation strategies and assess their feasibility and importance: results from the Expert Recommendations for Implementing Change (ERIC) study. Implement Sci. 2015;10:109.
Lane SR, Miller H, Ames E, Garber L, Kibbe DC, Schneider JH, et al. Consensus statement: feature and function recommendations to optimize clinician usability of direct interoperability to enhance patient care. Appl Clin Inform. 2018;9(1):205–20.
Vidrine JI, Reitzel LR, Figueroa PY, Velasquez MM, Mazas CA, Cinciripini PM, et al. Motivation and problem solving (MAPS): motivationally based skills training for treating substance use. Cogn Behav Pract. 2013;20(4):501–16.
Wetter DW, Mazas C, Daza P, Nguyen L, Fouladi RT, Li Y, et al. Reaching and treating Spanish-speaking smokers through the National Cancer Institute’s Cancer Information Service. A randomized controlled trial. Cancer. 2007;109(2 Suppl):406–13.
Vinci C, Lam C, Schlechter CR, Shono Y, Vidrine JI, Wetter DW. Increasing treatment enrollment among smokers who are not motivated to quit: a randomized clinical trial. Trans Behavior Med. 2022;12(1):ibab114.
Betancourt JR, Green AR, Carrillo JE. Cultural competence in health care: emerging frameworks and practical approaches. New York: The Commonwealth Fund; 2002.
Hays PA. Addressing cultural complexities in practice: a framework for clinicians and counselors. Washington: American Psychological Association; 2001.
Betancourt JR, Green AR, Carrillo JE. The patient’s culture and effective communication. https://www.uptodate.com/contents/the-patients-culture-and-effective-communication. Published 2021. Accessed 31 Mar 2023.
Knox M, Murphy EJ, Leslie T, Wick R, Tuot DS. e-Consult implementation success: lessons from 5 county-based delivery systems. Am J Manag Care. 2020;26(1):e21–7.
Dhingra L, Schiller R, Teets R, Nosal S, Rodriguez S, Cruciani G, et al. Race and ethnicity do not clinically associate with quality of life among patients with chronic severe pain in a Federally Qualified Health Center. Pain Med. 2018;19(7):1408–18.
Fritz JM, Lane E, Minick KI, Bardsley T, Brennan G, Hunter SJ, et al. Perceptions of telehealth physical therapy among patients with chronic low back pain. Telemed Rep. 2021;2(1):258–63.
Skolasky RL, Kimball ER, Galyean P, Minick KI, Brennan G, McGee T, et al. Identifying perceptions, experiences, and recommendations of telehealth physical therapy for patients with chronic low back pain: a mixed methods survey. Arch Phys Med Rehabil. 2022;103(10):1935–43.
Fischer SH, Predmore Z, Roth E, Uscher-Pines L, Baird M, Breslau J. Use of and willingness to use video telehealth through the COVID-19 pandemic. Health Aff. 2022;41(11):1645–51.
Chen K, Zhang C, Gurley A, Akkem S, Jackson H. Patient characteristics associated with telehealth scheduling and completion in primary care at a large, urban public healthcare system. J Urban Health. 2023;[Epub ahead of print].
Jones GT, Johnson RE, Wiles NJ, Chaddock C, Potter RG, Roberts C, et al. Predicting persistent disabling low back pain in general practice: a prospective cohort study. Br J Gen Pract. 2006;56:334–41.
Orhan C, Van Looveren E, Cagnie B, Mukhtar NB, Lenoir D, Meeus M. Are pain beliefs, cognitions, and behaviors influenced by race, ethnicity, and culture in patients with chronic musculoskeletal pain: a systematic review. Pain Physician. 2018;21(6):541–58.
Campbell LC, Andrews N, Scipio C, Flores B, Feliu MH, Keefe FJ. Pain coping in Latino populations. J Pain. 2009;10(10):1012–9.
Yoshikawa K, Brady B, Perry MA, Devan H. Sociocultural factors influencing physiotherapy management in culturally and linguistically diverse people with persistent pain: a scoping review. Physiotherapy. 2020;107:292–305.
Betancourt JR, Green AR, Carrillo JE, Ananeh-Firempong F. Defining cultural competence: a practical framework for addressing racial/ethnic disparitie in health and health care. Public Health Rep. 2003;118:293–302.
Werneke MW, Deutscher D, Grigsby D, Tucker CA, Mioduski JE, Hayes D. Telerehabilitation during the Covid-19 pandemic in outpatient rehabilitation settings: a descriptive study. Phys Ther. 2021;101(7):pzab110.
Jiang S, Wu L, Gao X. Beyond face-to-face individual counseling: a systematic review on alternative modes of motivational interviewing in substance abuse treatment and prevention. Addict Behav. 2017;73:216–35.
Patel ML, Wakayama LN, Bass MB, Breland JY. Motivational interviewing in eHealth and telehealth interventions for weight loss: a systematic review. Prev Med. 2019;126:105738.
Teeter BS, Kavookjian J. Telephone-based motivational interviewing for medication adherence: a systematic review. Transl Behav Med. 2014;4(4):372–81.
Gwadz M, Serrano S, Linnemayr S, Cleland CM, Cluesman SR, Freeman RM, et al. Behavioral intervention grounded in motivational interviewing and behavioral economics shows promise with Black and English-speaking Latino persons living with HIV with unsuppressed HIV viral load in New York City: a mixed methods pilot study. Front Public Health. 2022;10:916224.
Lee CS, Colby SM, Magill M, Almeida J, Tavares T, Rohsenow DJ. A randomized controlled trial of culturally adapted motivational interviewing for Hispanic heavy drinkers: theory of adaptation and study protocol. Contemp Clin Trials. 2016;50:193–200.
Anastas TM, Miller MM, Hollingshead NA, Stewart JC, Rand KL, Hirsh AT. The unique and interactive effects of patient race, patient socioeconomic status, and provider attitudes on chronic pain care decisions. Ann Behav Med. 2020;54(10):771–82.
Acknowledgements
The authors wish to thank the community health center staff, patients, and physical therapists for their contributions.
Funding
This work was supported by the NIH through the NIH HEAL Initiative under award number UG3NR019943 from the National Institute of Nursing Research. This work also received logistical and technical support from the PRISM Resource Coordinating Center under award number U24AT010961 from the NIH through the NIH HEAL Initiative. The work was also supported in part by the National Center for Advancing Translational Sciences of the NIH under award UL1TR002538 supporting research services through the Clinical and Translational Science Institute at the University of Utah. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or its HEAL Initiative.
Author information
Authors and Affiliations
Contributions
Conceptualization of this work was led by JMF, BG, DWW, GDF, and AT. Information was collected and curated by BG and VS. JMF, BG, GDF, DWW, VS, KL, IF, EB, and AT contributed to the interpretation of the information collected. Funding for the research was obtained by JMF. The original manuscript was compiled by JMF with major contributions from BG and AT. All authors contributed to the review and editing of the paper and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the University of Utah Institutional Review Board. Consent for participation in the activities reported in this study was obtained following guidelines from the University of Utah Institutional Review Board.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Fritz, J.M., Gibson, B., Wetter, D.W. et al. Use of implementation mapping in the planning of a hybrid type 1 pragmatic clinical trial: the BeatPain Utah study. Implement Sci Commun 5, 3 (2024). https://doi.org/10.1186/s43058-023-00542-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43058-023-00542-z