Abstract
Background
Despite the extensive hopes and expectations for value creation resulting from the implementation of artificial intelligence (AI) applications in healthcare, research has predominantly been technology-centric rather than focused on the many changes that are required in clinical practice for the technology to be successfully implemented. The importance of leaders in the successful implementation of innovations in healthcare is well recognised, yet their perspectives on the specific innovation characteristics of AI are still unknown. The aim of this study was therefore to explore the perceptions of leaders in healthcare concerning the innovation characteristics of AI intended to be implemented into their organisation.
Methods
The study had a deductive qualitative design, using constructs from the innovation domain in the Consolidated Framework for Implementation Research (CFIR). Interviews were conducted with 26 leaders in healthcare.
Results
Participants perceived that AI could provide relative advantages when it came to care management, supporting clinical decisions, and the early detection of disease and risk of disease. The development of AI in the organisation itself was perceived as the main current innovation source. The evidence base behind AI technology was questioned, in relation to its transparency, potential quality improvement, and safety risks. Although the participants acknowledged AI to be superior to human action in terms of effectiveness and precision in some situations, they also expressed uncertainty about the adaptability and trialability of AI. Complexities such as the characteristics of the technology, the lack of conceptual consensus about AI, and the need for a variety of implementation strategies to accomplish transformative change in practice were identified, as were uncertainties about the costs involved in AI implementation.
Conclusion
Healthcare leaders not only saw potential in the technology and its use in practice, but also felt that AI’s opacity limits its evidence strength and that complexities in relation to AI itself and its implementation influence its current use in healthcare practice. More research is needed based on actual experiences using AI applications in real-world situations and their impact on clinical practice. New theories, models, and frameworks may need to be developed to meet challenges related to the implementation of AI in healthcare.
Similar content being viewed by others
Background
Artificial intelligence (AI) has the potential to enhance healthcare in many high-income countries through improved efficiency, quality, and clinical and health outcomes [1, 2]. However, there are substantial challenges to the implementation of AI-based applications in healthcare, as for many other types of innovations in healthcare. AI can be defined as “a machine-based system that can, for a given set of human-defined objectives, make predictions, recommendations, or decisions influencing real or virtual environments … with varying levels of autonomy” [3, 4]. The technology behind AI applications is developing at breakneck speed and is pushing the boundaries of what is technologically possible, introducing expectations for accomplishing improvements in cost-effectiveness, staff workflow, and patient empowerment. To achieve these results, the European Union highlights the importance of safely introducing AI into healthcare, and for the creation and adoption of regulatory frameworks based on human rights and fundamental values [5]. However, while interest in AI is on the rise and the number of explorative and proof-of-concept projects are growing, the level of diffusion is still relatively low in healthcare [2, 6, 7]. There are several potential barriers to using AI in healthcare related to data-based, methodological, technological, regulatory, policy, and human factors [8] and evidence to support implementation strategies to tackle these barriers is still at an early stage [7]. The Consolidated Framework for Implementation Research (CFIR) describes and predicts barriers and facilitators for implementation connected to the characteristics of five theory domains: innovation, outer setting, inner setting, individuals and implementation processes. The degree to which different characteristics of the innovation itself are perceived as appropriate, acceptable, and feasible by individuals involved in the implementation process is key for facilitating the adoption of an innovation [9]. Perceptions of innovation characteristics have been found to be relevant for the implementation of many types of innovations across diverse settings, but how they influence the implementation of AI remains largely unexplored [1, 10, 11].
Implementation science highlights the importance of accounting for stakeholder views in the initial phase of the implementation, as it is key to knowing how different stakeholder groups perceive the characteristics of an innovation and its potential impact on population health and its value for patients [12]. For successful implementation, it is especially important to understand and consider the perspective of leaders [13] yet this is one of the stakeholder groups that has received relatively little attention in research regarding AI implementation [14]. Leaders are usually important in promoting organisational capacity to initiate, guide, and accomplish implementation processes [15,16,17,18]. Still, research on leadership in implementation science is still underdeveloped, particularly in relation to the implementation of AI in healthcare, where the main focus has been on other stakeholder groups like healthcare professionals [19,20,21], patients [22], and industry partners [23]. The paucity of knowledge concerning the importance of leadership in the successful implementation of AI in healthcare has been illustrated in two recent scoping reviews which highlighted that few studies mentioned leadership in relation to AI implementation [24] and that there is a need for more theory-based research on the implementation of AI [7, 25].
Considering the importance of leadership for the implementation, adoption, and use of AI, this study addresses a significant knowledge gap: it aims to explore the perceptions of healthcare leaders in clinical and administrative roles concerning the innovation characteristics of AI as an innovation to be implemented into their organisation.
Methods
This study was conducted within the frame of a research program “Toward Successful Implementation of Artificial Intelligence in Health Care Practice” [6] with the objective of developing a theoretically and empirically informed framework for AI implementation in healthcare that can be used to facilitate AI implementation in routine healthcare practice. Some of the research activities in this program include mapping different stakeholder perspectives, including those of leaders, healthcare professionals, and patients, with the purpose of understanding contextual aspects regarding requirements, barriers, and enabling factors for the implementation of AI systems in practice. The current study is an important contribution to research on AI implementation in healthcare, offering insights into healthcare leader’s perspectives on the innovative characteristics of AI.
Design
The study has a qualitative design and adopts a directed approach to qualitative content analysis [26] meaning that the structure of the deductive data analysis was operationalised on the basis of previous knowledge, models, or theory. The Consolidated Framework for Implementation Research (CFIR) outlines determinants that influence implementation efforts, and provides concepts, terms, and definitions to aid researchers in navigating the complex research and practice field. Constructs from the innovation domain in CFIR are used as a deductive tool in the data analysis. The study is reported in accordance with the Consolidated Criteria for Reporting Qualitative Research 32-item checklist to ensure trustworthiness (Additional file 1) [27].
Theoretical framework
In this study, the CFIR framework was used as a theoretical foundation. The CFIR is intended to collect data from individuals who have power and influence over implementation outcomes [9] and was judged to be appropriate to guide our analysis. In this study, we limited the analysis to the framework’s innovation domain. CFIR’s innovation domain includes eight constructs (innovation source, evidence base, relative advantage, trialability, adaptability, complexity, design, and cost) (Table 1).
Setting
The study was conducted in southwest Sweden. Participants were employed in a county council that, over the last decade, has invested financial, personnel, and service resources to develop capacity to structure and analyse healthcare data to generate information on which improvement initiatives can be based [28]. The deployment of AI in the organisation is at an early stage.
Participants and recruitment
The purposeful recruitment of study participants from the county council focused on leaders in a position to potentially influence the implementation of AI. The study participants belong to a group of high-level county council managers with ‘working knowledge’ related both to AI and to implementing innovations. They had an understanding of the members in the setting and its contextual influences. Damschroder et al. (2022) refer to these individuals as “individuals with a high level of authority, including key decision-makers, executive leaders, or directors” [9].
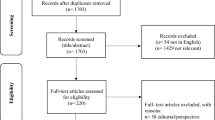
The number of interviewees was consequently increased organically through a snowballing technique until a sense of the multiple types of leaders emerged and no further roles in the representation of leadership functions within the county council’s organisation were identified. A total of 28 participants were invited to participate in the study via an email including study information. Of these, 26 individuals (18 men and 8 women) were willing to participate in interviews.
Fourteen participants worked in top-level management functions in healthcare. Two participants were top-level regional politicians. Two participants had a technical advisory function. Eight participants had a quality development portfolio in their remit and worked in a strategic role either at an intermediate level or in local quality development roles. Two participants worked in primary healthcare and two worked in secondary care.
Data collection
The interviews were conducted via phone or video communication by a female researcher (LP, trained in work technology environments, PhD) and a male colleague (DT, trained in management research, PhD); neither of whom had any previous relationship with the participants. The interviews were conducted with each participant on a one-to-one basis on one occasion. A semi-structured approach was used, and the participants were asked to share their perspectives of AI as a phenomenon, their experiences with AI, and their perceptions of what could hinder or facilitate implementation of AI in their workplace (Additional file 2). Although AI systems are designed to operate with varying levels of autonomy, the interview questions did not differentiate between different kinds of AI technology. Two pilot interviews were conducted to test the questions, and since no adjustments were required, these interviews were included in the study. The interviews took place between October 2020 and May 2021 and lasted between 30 and 120 min, with a total length of 23 h and 49 min. The interviews were audio-recorded and transcribed verbatim.
Data analysis
The study used qualitative content analysis with a directed (deductive) approach, using a stepwise method described by Hsieh and Shannon [25]. The analysis of the qualitative data was undertaken with the software program Nvivo (NVivo 14 for Windows). In the first step of the analysis, all transcripts were read in their entirety by all authors. In the second step, PN and MN constructed a codebook (Table 1) based on the definitions of the eight constructs in CFIR’s innovation domain [9] and adapted these to the study context by operationalising them to fit the innovation (AI). While the definitions adhered closely to the original content of the constructs, the adapted definitions were designed to serve as codes and facilitate the qualitative analysis of the data. The definitions were iteratively discussed and ultimately finalised by the authors. The codes based on these constructs formed the main categories. In the third step, the codes were applied to each interview. The first author (MN) allocated meaning units to the main categories, using the descriptions for each construct in the codebook. The preliminary allocation of meaning units to the main categories was iteratively and repeatedly discussed between all the authors until consensus was achieved. The content in each main category was collated by the first author (MN) and inductively abstracted into subcategories, with the conscious intention of preserving variation in the scope and depth of the data. Following this method, the researchers moved back and forth through the steps in order to validate, revise, and refine the findings. Although data saturation was indicated after the 19th interview (new data did not add to the variation and scope of codes), all interviews were coded. Quotes from the data were chosen to illustrate and add depth to the descriptive text in each category and translated verbatim.
Findings
The results show that the study participants have high expectations regarding the relative advantages of AI for the organisation, for health professionals, and for patients. They perceived the innovation source of AI to be located primarily in the organisation itself, but at the same time highlighted the need for outside professional assistance with the innovation design. Concerns were expressed around the evidence base of AI innovation; mainly for reasons of data security and undetected bias in the technology. They perceived that AI was highly complex—something reflected in the scope and nature of the technology itself, and in the steps involved in safely processing data and effectively managing clinical change. Perceptions of innovation trialability, adaptability, and costs were tentative because of the early stage of AI implementation in the organisation (Table 2).
Innovation relative advantage
Participants believed that a relative advantage of AI as an innovation to be implemented in healthcare lies in its effective and comprehensive management of large volumes of data from different sources, and in particular, data from the data warehouse of the organisation itself. Participants saw AI as part of a necessary development, as healthcare would not, in the long run, be able to keep up with the population’s healthcare needs. The application of AI technology was thought to enable decision-makers to allocate resources where they are most needed within the organisation. Management decisions regarding organisational changes in primary care units and hospitals were considered to be supported through the aggregation of data on outcomes from various care activities at multiple sites.
The participants also perceived AI’s potential to support professional decision-making in clinical care. AI was specifically perceived to be able to contribute through its ability to analyse images from digital imaging systems with a high level of precision and time effectiveness. The capacity of AI was perceived to be superior to the human analysing ability of even very clinically experienced professionals, in that it was not only more efficient and precise but also less biased.
AI was not perceived as replacing the need for human interaction between caregivers and patients, as this would provide other information, such as the patient’s preferences and state of mind. On the other hand, participants thought that AI could be equivalent to a colleague as a ‘second opinion’ in situations of uncertainty.
The participants described that AI could serve as a warning or a ‘yellow flag’, alerting healthcare professionals to clinical data that needs to be taken into account given a certain situation and specific conditions. The participants considered this to be uncontroversial, as they saw AI as just another tool to help healthcare professionals in their clinical work.
The participants had great expectations for possible AI-based applications that could about in the future. ‘Digital triage’ was perceived as an attractive idea to help empower patients in their own care and to achieve more effective care; acting as a self-help tool for some patients. This was expected to generate more time for clinicians to spend working with vulnerable patients. They also envisaged that standard health information could be collected from the patient and an AI-informed selection of laboratory tests could be completed prior to the primary healthcare visit, making the patient–provider encounter more informed and time-efficient.
Another aspect of perceived relative advantage was the potential of AI for discovering previously unknown patterns of care flow and its early detection of disease, facilitating health predictions for individual patients or groups of at-risk patients. Participants highlighted the AI algorithm’s ability to impartially discern clinical patterns based on multiple data sources without the need for prior clinical training, preunderstandings, or assumptions.
Innovation source
Regarding the innovation source subdomain, participants thought that AI would primarily be internally developed in the near future. They thought that their organisation had some readiness to develop AI because of a relatively long history of investing in AI. Strategic leadership in the county council was perceived to have supported AI development and research early on, which led to a perception of local ownership in AI development within the county council.
AI as an innovation was perceived as a ‘hot topic’, and collaborations with universities and other actors like those in industry were seen as strategic, allowing the county council to take advantage of this ‘window of opportunity’. Some even expected local healthcare professionals to actively participate in the development of AI-based applications for use in their own field of interest.
Networking around the use of AI within the larger national healthcare system was perceived as a slower and more cumbersome process than regional collaboration with specific tech companies. However, participants believed that many tech companies were not equipped to follow the accepted quality and safety standards in healthcare, which led to hesitations about relying on these companies for AI implementation.
Innovation evidence base
Although the participants described the innovation’s evidence base to be of key importance in AI implementation, they perceived the evidence base itself to be highly questionable. The participants felt they lacked control over the long chains of data processing and perceived that they had no insight into which process decisions were made along the way, for which reasons, and by whom.
Some participants perceived that it was possible to take the positive results of using AI as proof of its effectiveness, but highlighted the risk of bias in the data upon which the technology is based and how health data were processed. They felt strongly about the need for quality and safety control of AI-based applications; considering the consequences of faulty and skewed data-processing in AI and the large potential impact AI imperfections could have on managerial and health outcomes.
The participants thought that due to data being transferred between systems, aggregated, and repackaged, the original data would become increasingly difficult to retrieve and use.
The participants perceived that the mathematical complexity of AI prohibited an easy understanding of the reasoning that lay behind the information presented by AI; they characterised AI as a ‘little black box’. One of the reasons for questioning the evidence base of AI-based applications was that the knowledge-base and data behind AI could not be verified in traditional and transparent ways, like reading up on relevant scientific research findings.
Innovation adaptability
The participants perceived AI to have a degree of adaptability, but they also believed it to fit more naturally into some clinical contexts than in others. Care units relying on medical imaging techniques as an important work tool were perceived as especially prepared to make changes toward AI-based diagnostic support. Areas that were highlighted in this aspect were radiology, pathology, clinical laboratory medicine, and dermatology. The participants thought that using AI would encounter barriers in other work units because of the perceived need to protect sensitive personal data.
Innovation trialability
Regarding the innovation’s trialability, participants suggested testing AI on a small scale in the organisation but did not discuss any ways to retract the implementation, if necessary. The current use of AI for managing care within the organisation was experienced as gaining in importance and was tested in an ongoing process. The participants expected to be able to test a small number of AI-based applications in clinical contexts within the next few years; partly due to having observed that IT systems had prepared the technical infrastructure for AI ‘behind the scenes’.
AI-based digital imaging tools intended for use as diagnostic tools were seen as feasible for testing in clinical use, but participants also perceived it would be necessary to create more opportunities for testing other AI algorithms developed for use in care processes in clinical practice. The participants tentatively discussed where new AI-based applications could be appropriate and feasible; e.g. in situations that are a step removed from patient–provider encounters. They also reasoned about the usefulness of AI in situations of broader diagnostic uncertainty; in primary care consultations, for example. Some participants perceived that AI is already more or less informally present in some clinical contexts.
Innovation design
Participants perceived that AI’s innovation design will be important for future implementation. They imagined that AI applications in healthcare need the AI component to be as simple to use as possible, while at the same time should be designed to target complex problems healthcare professionals need help in solving.
Participants were not convinced that the healthcare organisation itself could manage to design the AI applications without external expertise. They perceived that only developing AI models and algorithms were insufficient when it came to integrating the technology into practice and that the technical functions of AI needed to be integrated into user-friendly products designed for the use of healthcare professionals. They also perceived that future IT infrastructure development was necessary to integrate AI into IT systems for ease of use. Participants believed that AI could have different designs based on the same data but tailored to users of different professional backgrounds and patients with differing levels of digital and health literacy.
Innovation complexity
Participants perceived multifaceted innovation complexity in the implementation and use of AI. They believed that there are many competing and occasionally conflicting opinions about what AI is and what it is not. Decisions about investments in AI were the remit of top-level management, but participants expressed a lack of guidance pertaining to decisions connected to AI. They wanted their decisions to be based on a thorough knowledge of the AI technology itself, and which type of problems it can be expected to solve. However, they were unclear as to which criteria should be used for decision-making about how and where to start applying AI in clinical practice.
The participants highlighted that collecting large volumes of data was not realistic at present, as health data were fragmented in the system, and current IT systems were not mutually compatible. Sharing data and exchanging knowledge between county councils was anticipated to be difficult, as different county councils make independent choices concerning how to build the data warehouses and which technologies and suppliers to invest in. The participants perceived risks of privacy violation during managing, monitoring, and storing large volumes of sensitive health data from many different data sources, involving different IT systems and numerous staff in technical and medical capacities and storage in commercial facilities. They also said that current legislation prohibits data sharing between different caregiving agencies in county councils and municipalities.
Participants experienced that processes of change tend to move very slowly in healthcare. In addition to professional change resistance and organisational barriers, a high level of scepticism around AI was to be expected.
Participants also expected AI to be potentially challenging to professionals in their professional role, in situations where AI might possibly provide healthcare professionals and patients with information that was not previously available, and which they are currently unequipped and unprepared to deal with.
Many other factors were expected to add to the complexity of implementing AI: levels of digital literacy on the part of patients and healthcare professionals, varying interest levels in AI in different professional fields, levels of technological know-how available in the organisation, and the capacity of healthcare leadership at all levels.
Not being fully cognisant of the scope and depth of knowledge in AI was thought to have consequences for patient safety in clinical practice. The participants perceived that there were risks of staff becoming overly reliant on the knowledge provided by AI, which could lead to more limited use of clinical reasoning. They highlighted that repeatedly exercising professional judgement was necessary for developing clinical expertise over time. This was seen as especially important for younger professionals, but even more experienced clinicians could risk becoming overly confident in AI-informed decision support.
The participants expected that the issue of AI leading to transformative changes for healthcare professionals and patients needed to be discussed by society, as healthcare would change profoundly towards being more prevention-focused in the future, with citizens expected to be more in charge of managing their own health.
Innovation costs
The participants could not estimate the innovation costs of AI technology at present, but perceived that no state-allocated resources were available for more large-scale implementation and roll-out of AI. The participants had varying perceptions as to the success of the organisation’s efforts in developing AI so far, with some applauding current and past AI development efforts, while others instead questioned the outcome of the resources that the organisation had used for AI development.
Participants were uncertain about the level of costs involved in the future larger-scale implementation of AI but feared that some currently ongoing research and development projects could suffer. Although purchasing AI products and upgrading IT system capacity was thought to be costly, some participants thought that IT infrastructure was ready and able to accommodate AI, which would alleviate costs over the long term. The cost of product development by external companies was perceived as a barrier to implementation in the short term, as procurement procedures at present do not apply to AI. Over a longer perspective, participants expected that the organisation could incur financial costs for purchase, support, and maintenance of AI technology. Future projections of costs was perceived to include the potential recruitment of AI-competent staff.
Discussion
The study explored the perceptions of leaders in healthcare concerning the innovation characteristics of AI of relevance for the adoption, implementation and use of AI in their organisation. Their perceptions were categorised in accordance with the eight constructs in the Innovation domain in CFIR. The results show that participants had high expectations of the innovation relative advantage of AI even though they were not convinced of the innovation evidence base of AI. The leaders were more tentative in their perceptions of innovation trialability, innovation adaptability, innovation design, and innovation costs, because of the relatively early stage of deployment of AI in their organisation. Participants’ expressions concerning innovation source and innovation complexity were indicative of conflicting perceptions: there were both perceptions that AI could be developed internally and that it needed a commercial expertise to make it work, and participants expressed both that AI was simple and very complex to implement.
The degree to which the characteristics in the innovation domain were perceived by leaders to support their expected implementation of AI may be seen to reflect both technology-related aspects and socio-organisational (people-process) aspects of AI. Considerations related to the technology-related aspects of AI were mainly found in leaders’ perceptions related to navigating the complicated issues concerning weighing the ins and outs of data management and data security and limited knowledge of the evidence of AI against the promises of its advantage over the effectiveness of current healthcare. AI-relevant legislation protecting health data, limited technological standardisation, ethical issues and supporting legal infrastructure for data-sharing are barriers to tackle if the ambitious Swedish eHealth goals are to be realised [29]. The complexity around legal and logistical barriers for implementing AI in healthcare non-withstanding, the spread of AI in all parts of society was not doubted by the leaders in our study. It is notable that the current societal and political enthusiasm for the benefits of AI was prominent in all the interviews, and in some cases compensated some leaders’ more negative perceptions about its evidence base, even though the opacity in AI was highlighted. The lack of intuitive understanding of the theory underlying AI model development and the high level of mathematical and statistical complexity has been termed as the “black box problem” [30]. Similarly, the ways in which AI models achieve their results are not always comprehensible [31]. Among the most important weaknesses in AI are potential biases embedded both within algorithms and within the data used to train algorithms [32]. Some potential trialability of AI was perceived by the leaders in the study, mainly because of the infrastructure they had in the organisation for some to test a small number of AI-based applications. Research confirms that a necessary foundation for delivering AI in healthcare is the extensive use of electronic health records and a high degree of interoperability between IT systems, even though the latter is a problem in many instances [8].
Considerations related to the socio-organisational aspects in many cases concerned dealing with uncertainties. This was expressed as the conceptual ambiguity of AI and the expected difficulties of managing distrust of AI in parts of the organisation, the uncertainty around where to develop and test AI, which types of AI applications to prioritise, and managing an unknown budget for AI implementation. The leaders described complexity in relation to AI’s conceptual ambiguity, which they perceived as potentially detrimental to communication around the technology. The general understanding of AI is diffuse for several reasons. Firstly, the term AI is used in many different ways in computer science, engineering and healthcare [33]. Secondly, the characteristics of AI are continually evolving, and different types of “AI” exist in parallel [30, 31, 34]. Thus, how we use the term AI needs to be clarified to identify nuances and differences of the AI technologies and AI systems, and study the specific challenges involved in their safe and effective implementation [31]. Leaders’ expressions concerning the innovation source were indicative of conflicting perceptions: there were both perceptions that AI could and should be developed internally and that the organisation needed commercial expertise to make it work. Internally developed AI was seen as providing a real possibility of input by users (such as healthcare professionals and patients) on the innovation design, which could impact implementation at all levels. Indeed, research confirms that there is a need to incorporate expertise and knowledge from different user groups in the development of AI-based applications. Combining the expertise of both computer scientists and healthcare professionals is key for making meaningful use of the data [2]. Furthermore, collaboration between levels and parts of systems and between organisations is needed to counter the disruptiveness in care flows [35]. Regarding costs, the leaders expressed that many aspects are unclear about the trade-off between costs and profits. Research confirms that there is a need to describe the initial investment and operational costs for infrastructure and service delivery of AI in future studies and that other options to achieve a similar impact must be benchmarked to inform strategic planning [36].
The considerations that managers and leaders express around both technical aspects and socio-organisational aspects of AI as a technology to be implemented into their organisation are of interest because of their central importance in the implementation process. The importance of leadership is evident in several of the models and frameworks used in implementation science. However, while implementation science has increasingly drawn attention to the role of leadership for successful implementation of interventions and innovations in healthcare, there is relatively limited research on leadership in healthcare [13, 37,38,39] and especially in the field of AI implementation in healthcare. Leadership is usually defined in terms of a process of influence to achieve certain goals, i.e. guiding a group to accomplish a task [40]. The vast majority of the 28 participants in our study were leaders with a position as a manager in the county council and all were considered to be leaders with regard to the implementation of AI in healthcare. However, there may also be other persons in healthcare who are not necessarily formal managers but still have a great deal of influence on AI implementation. Physicians are often described as leaders in many healthcare contexts and their involvement in various implementation and improvement initiatives is often crucial for achieving desired goals [41]. Research has documented ambivalence among physicians towards AI, with diverse and sometimes contradictory viewpoints [42,43,44]. Concern has been expressed about a loss of autonomy among physicians and the increasing integration of AI into human-centred care, which some fear could lead to a gradual replacement of physicians with AI applications. Physicians gather and process medical information to make a diagnosis, which are tasks that could potentially be performed by AI applications [20, 45, 46]. In our study the leaders’ expressed expectations of mistrust among healthcare professions in health care. Research has documented a diversity in attitudes regarding AI among various stakeholders [44, 47, 48]. Thus, understanding what drives different stakeholders’ perceptions of AI in healthcare is important. Further research into how and why differing views are held could assist the development of strategies that accommodate such diversity of views.
Study limitations and methodological considerations
The study has some limitations that need to be considered when interpreting the results. Participation in the study was voluntary, which means that the leaders who agreed to participate may have been particularly interested in the topic or may have vested interest in ongoing efforts to implement AI. However, it is difficult to determine how this might have affected the results. The innovation itself (i.e., AI) appeared to be interpreted by participants in different ways. The different terms that the participants used reflect the general immaturity of the language describing different forms of AI and the topic’s relative novelty for the participants. The manifold terms used when talking about AI are also indicative of the participants’ perception of AI as a “general purpose technology”. [33]. Future studies could benefit from a clearer delineation up-front of the different applications of the technology to understand more in-depth how each application is perceived by leaders in healthcare.
We applied CFIR in the analysis to categorise the findings concerning perceptions of AI. CFIR is a widely-used determinant framework to evaluate the implementation of interventions in healthcare. Determinant frameworks are used in implementation science to describe different types of influences on implementation that are hypothesised to—or have been found to—impact implementation outcomes. CFIR has previously been used to assess the implementation of AI applications in various settings [49, 50]. In this study, we limited its use to eight characteristics in the innovation domain in the CFIR framework [9] which we found suitable to address aspects of perceptions deemed relevant to the study aim.
The transferability of the study’s results is primarily limited to Swedish healthcare. However, key characteristics of AI may be generalisable beyond the Swedish context to inform stakeholders about possible facilitators and barriers for the adoption, implementation, and use of AI [51]. Communication around these determinants in a standardised manner may facilitate dialogue [52]. It should be remembered, however, that the characteristics of an innovation are not stable features, nor are they the only determinant of adoption and implementation. The interaction between the innovation, the intended adopters, and the context influences the adoption and implementation of innovations [53, 54].
The multidisciplinary research team was a strength of the study because it permitted different perspectives on the issue of leaders’ perceptions of AI. The team consisted of researchers with expertise in implementation science, intervention science, and health science with a specific focus on the implementation of health innovations (such as AI applications) in healthcare. Another strength was the relatively high number of interviews (n = 28) which added trustworthiness to the findings.
Conclusions
In conclusion, this study found that Swedish healthcare leaders preparing to implement AI acknowledged the potential for AI to contribute to improvements in healthcare. They had high expectations of the relative advantage of AI but were less convinced of its evidence base (AI’s safety and effectiveness) and tentative in their perceptions of the innovation’s trialability, adaptability, design, and costs. This may have implications for future implementation of AI: to ensure the adoption, implementation, and sustained use of AI in healthcare, implementation strategies will likely need to be designed to manage perceptions of innovation characteristics of AI at the leadership level at early stages of the technology’s implementation. More in-depth knowledge is needed about perceptions of the barriers and facilitators to AI implementation in other stakeholder groups and about outcomes from the implementation of AI in real-world situations to develop strategies to support its implementation in practice.
Availability of data and materials
Empirical material generated and/or analysed during the current study are not publicly available, but are available from the corresponding author on reasonable request.
References
Mehta N, Pandit A, Shukla S. Transforming healthcare with big data analytics and artificial intelligence: a systematic mapping study. J Biomed Inform. 2019;100:103311.
De Nigris S. CM, Nepelski D., Hradec J., Gómez-González E, Gomez E , M.Vazquez-Prada Baillet, R. Righi, G.De Prato, M. López Cobo, S. Samoili, M.Cardona. AI Watch: AI Uptake in Health and Healthcare 2020. Luxembourg: Publications Office of the European Union; 2020. p. 2022–02–19.
WHO. Ethics and governance of artificial intelligence for health: WHO guidance. Geneva: World Health Organisation; 2021. Available from: https://www.who.int/publications/i/item/9789240029200.
EU. Excellence and trust in artificial intelligence. 2019. Updated 2021–03–09. Available from: https://commission.europa.eu/strategy-and-policy/priorities-2019-2024/europe-fit-digital-age_en.
EU. National strategies on Artificial Intelligence A European perspective in 2019 Country report – Sweden. 2021. Cited 2022 March 23. Information material. Available from: https://knowledge4policy.ec.europa.eu/sites/default/files/sweden-ai-strategy-report.pdf
Svedberg P, Reed J, Nilsen P, Barlow J, Macrae C, Nygren J. Toward successful implementation of artificial intelligence in health care practice: protocol for a research program. JMIR Res Protoc. 2022;11(3):e34920.
Sharma M, Savage C, Nair M, Larsson I, Svedberg P, Nygren JM. Artificial Intelligence Applications in Health Care Practice: Scoping Review. J Med Internet Res. 2022;24(10): e40238.
Topol EJ. High-performance medicine: the convergence of human and artificial intelligence. Nat Med. 2019;25(1):44–56.
Damschroder LJ, Reardon CM, Widerquist MAO, Lowery J. The updated consolidated framework for implementation research based on user feedback. Implement Sci. 2022;17(1):75.
He J, Baxter SL, Xu J, Xu J, Zhou X, Zhang K. The practical implementation of artificial intelligence technologies in medicine. Nat Med. 2019;25(1):30–6.
Yin J, Ngiam KY, Teo HH. Role of artificial intelligence applications in real-life clinical practice: systematic review. J Med Internet Res. 2021;23(4):e25759.
Braithwaite J, Churruca K, Long JC, Ellis LA, Herkes J. When complexity science meets implementation science: a theoretical and empirical analysis of systems change. BMC Med. 2018;16(1):63.
Reichenpfader U, Carlfjord S, Nilsen P. Leadership in evidence-based practice: a systematic review. Leadersh Health Serv (Bradf Engl). 2015;28(4):298–316.
Nilsen P, Bernhardsson S. Context matters in implementation science: a scoping review of determinant frameworks that describe contextual determinants for implementation outcomes. BMC Health Serv Res. 2019;19(1):189.
Damanpour FSM. Phases of the adoption of innovation inorganizations: effects of environment, organization and top managers. Brit J Manage. 2006;17:215–36.
Weiner BJ. A theory of organizational readiness for change. Implement Sci. 2009;4(1):67.
Harvey G, Fitzgerald L, Fielden S, McBride A, Waterman H, Bamford D, et al. The NIHR collaboration for leadership in applied health research and care (CLAHRC) for Greater Manchester: combining empirical, theoretical and experiential evidence to design and evaluate a large-scale implementation strategy. Implement Sci. 2011;6(1):96.
Aarons GA HJ, Dlugosz LR, Ehrhart MG. The role of organizational processes in dissemination and implementation research. In: Brownson RC CG, Proctor EK, editors. Dissemination and implementation research in health: translating science to practice. New York: Oxford University Press; 2012.
Shinners L, Aggar C, Grace S, Smith S. Exploring healthcare professionals’ understanding and experiences of artificial intelligence technology use in the delivery of healthcare: an integrative review. Health Informatics J. 2020;26(2):1225–36.
Laï MC, Brian M, Mamzer MF. Perceptions of artificial intelligence in healthcare: findings from a qualitative survey study among actors in France. J Transl Med. 2020;18(1):14.
Diprose WK, Buist N, Hua N, Thurier Q, Shand G, Robinson R. Physician understanding, explainability, and trust in a hypothetical machine learning risk calculator. J Am Med Inform Assoc. 2020;27(4):592–600.
Nelson CA, Pérez-Chada LM, Creadore A, Li SJ, Lo K, Manjaly P, et al. Patient perspectives on the use of artificial intelligence for skin cancer screening: a qualitative study. JAMA Dermatol. 2020;156(5):501–12.
Lee D, Yoon SN. Application of artificial intelligence-based technologies in the healthcare industry: opportunities and challenges. Int J Environ Res Public Health. 2021;18(1):271.
Chomutare T, Tejedor M, Svenning TO, Marco-Ruiz L, Tayefi M, Lind K, et al. Artificial Intelligence implementation in healthcare: a theory-based scoping review of barriers and facilitators. Int J Environ Res Public Health. 2022;19(23):16359.
Gama F, Tyskbo D, Nygren J, Barlow J, Reed J, Svedberg P. implementation frameworks for artificial intelligence translation into health care practice: scoping review. J Med Internet Res. 2022;24(1):e32215.
Hsieh HFSS. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–88.
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–57.
Ashfaq A, Lönn S, Nilsson H, Eriksson JA, Kwatra J, Yasin ZM, et al. Data resource profile: regional healthcare information platform in Halland Sweden. Int J Epidemiol. 2020;49(3):738–9.
eHälsomyndigheten. A strategy for implementing Vision for eHealth 2025: Swedish National Council for eHealth solutions; 2020. Cited 2022 March 6. Available from: https://ehalsa2025.se/wp-content/uploads/2021/02/Strategy-2020-2022_eng.pdf.
Asan O, Bayrak AE, Choudhury A. Artificial intelligence and human trust in healthcare: focus on clinicians. J Med Internet Res. 2020;22(6):e15154.
Shaw J, Rudzicz F, Jamieson T, Goldfarb A. Artificial intelligence and the implementation challenge. J Med Internet Res. 2019;21(7):e13659.
Howard A, Borenstein J. The ugly truth about ourselves and our robot creations: the problem of bias and social inequity. Sci Eng Ethics. 2018;24(5):1521–36.
Samoili S, López Cobo M, Delipetrev B, Martínez-Plumed F, Gómez E, De Prato G. AI watch, defining artificial intelligence 2.0 : towards an operational definition and taxonomy for the AI landscape. European Commission Joint Research Centre Publications Office of the European Union; 2021.
Challen R, Denny J, Pitt M, Gompels L, Edwards T, Tsaneva-Atanasova K. Artificial intelligence, bias and clinical safety. BMJ Qual Saf. 2019;28(3):231–7.
Scott W. Institutional change and healthcare organisations: from professional dominance to managed care. Chicago: University of Chicago Press; 2000.
Wolff J, Pauling J, Keck A, Baumbach J. The economic impact of artificial intelligence in health care: systematic review. J Med Internet Res. 2020;22(2):e16866.
Wensing M, Wollersheim H, Grol R. Organizational interventions to implement improvements in patient care: a structured review of reviews. Implement Sci. 2006;1:2.
Yano EM. The role of organizational research in implementing evidence-based practice: QUERI Series. Implement Sci. 2008;3(1):29.
French B, Thomas LH, Baker P, Burton CR, Pennington L, Roddam H. What can management theories offer evidence-based practice? A comparative analysis of measurement tools for organisational context. Implement Sci. 2009;4:28.
Yukl G. Leadership in Organizations. 6th ed. Upper Saddle River, NJ: Pearson Education; 2006.
Danielsson M. Patient Safety Cultural Perspectives. Linköping: Linköping University; 2018.
Aung YYM, Wong DCS, Ting DSW. The promise of artificial intelligence: a review of the opportunities and challenges of artificial intelligence in healthcare. Br Med Bull. 2021;139(1):4–15.
Martinho A, Kroesen M, Chorus C. A healthy debate: exploring the views of medical doctors on the ethics of artificial intelligence. Artif Intell Med. 2021;121: 102190.
Scott IA, Carter SM, Coiera E. Exploring stakeholder attitudes towards AI in clinical practice. BMJ Health Care Inform. 2021;28(1):e100450.
Karches KE. Against the iDoctor: why artificial intelligence should not replace physician judgment. Theor Med Bioeth. 2018;39(2):91–110.
Bhattacharya S, Pradhan KB, Bashar MA, Tripathi S, Semwal J, Marzo RR, et al. Artificial intelligence enabled healthcare: a hype, hope or harm. J Family Med Prim Care. 2019;8(11):3461–4.
Quinn TP, Senadeera M, Jacobs S, Coghlan S, Le V. Trust and medical AI: the challenges we face and the expertise needed to overcome them. J Am Med Inform Assoc. 2021;28(4):890–4.
Sujan MA, White S, Habli I, Reynolds N. Stakeholder perceptions of the safety and assurance of artificial intelligence in healthcare. Saf Sci. 2022;155: 105870.
Castor D, Saidu R, Boa R, Mbatani N, Mutsvangwa TEM, Moodley J, et al. Assessment of the implementation context in preparation for a clinical study of machine-learning algorithms to automate the classification of digital cervical images for cervical cancer screening in resource-constrained settings. Front Health Serv. 2022;2:1000150.
Schouten B, Schinkel M, Boerman AW, van Pijkeren P, Thodé M, van Beneden M, et al. Implementing artificial intelligence in clinical practice: a mixed-method study of barriers and facilitators. J Med Artif Intell. 2022;5:12. https://doi.org/10.21037/jmai-22-71.
Engell T, Løvstad AM, Kirkøen B, Ogden T, Amlund HK. Exploring how intervention characteristics affect implementability: a mixed methods case study of common elements-based academic support in child welfare services. Child Youth Serv Rev. 2021;129:106180.
Bewick BM, Ondersma SJ, Høybye MT, Blakstad O, Blankers M, Brendryen H, et al. Key intervention characteristics in e-health: steps towards standardized communication. Int J Behav Med. 2017;24(5):659–64.
Greenhalgh T, Wherton J, Papoutsi C, Lynch J, Hughes G, A’Court C, et al. Beyond adoption: a new framework for theorizing and evaluating nonadoption, abandonment, and challenges to the scale-up, spread, and sustainability of health and care technologies. J Med Internet Res. 2017;19(11):e367.
Nilsen P, Birken, S. Prologue. In: Nilsen P, Birken, S, editor. Handbook on implementation science: Edward Elgar Publishing; 2020. p. 1–6.
WMA. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–4.
Acknowledgements
The authors would like to thank Daniel Tyskbo (DT) and the participants who contributed to this study with their experiences.
Funding
Open access funding provided by Halmstad University. The funders of this study are the Swedish Government Innovation Agency Vinnova (grant 2019–04526) and the Knowledge Foundation (grant 20200208 01H). The funders were not involved in any aspect of study design, collection, analysis, interpretation of data, or in the writing or publication processes.
Author information
Authors and Affiliations
Contributions
All authors together identified the research question and designed the study. Applications for funding and coproduction agreements were put into place by PS and JMN. Data collection (the interviews) was carried out by LP and DT. Data analysis was performed by MN, LP, and IL and then discussed with JN, PN, and PS. The manuscript was drafted by all the authors, and all of them have read and approved the final submitted version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study conforms to the principles outlined in the Declaration of Helsinki [55] and was approved by the Swedish Ethical Review Authority (no. 2020–06246). The study fulfilled the requirements of Swedish research: information, consent, confidentiality, and safety of the participants; and is guided by the ethical principles of autonomy, beneficence, non-maleficence, and justice. Participants first received an e-mail with a short information on the research project and, at the same time, were asked whether they wanted to participate in the study. If they agreed to participate, they were verbally informed at the beginning of the interview about the purpose and the structure of the study and that they could withdraw their consent to participate at any time. They were also informed of their right to decline participation altogether or to exit the interview and the study at any time. Participants were informed that the interview was confidential and that any personal data obtained in the interview would be protected during the entirety of the research process and in the final publication. Participation was voluntary and the respondents were informed about the ethical considerations of confidentiality. Informed consent was obtained from all participants prior to the interview.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no potential conflicts of interest with respect to the research, authorship, and publication of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Consolidated criteria for reporting qualitative studies (COREQ): 32-item checklist.
Additional file 2.
Interview guide.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Neher, M., Petersson, L., Nygren, J.M. et al. Innovation in healthcare: leadership perceptions about the innovation characteristics of artificial intelligence—a qualitative interview study with healthcare leaders in Sweden. Implement Sci Commun 4, 81 (2023). https://doi.org/10.1186/s43058-023-00458-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43058-023-00458-8