Abstract
Background
Minimally invasive direct coronary artery bypass (MIDCAB) grafting is a safe technique for revascularization of the left anterior descending artery. The objective of this study was to evaluate the long-term outcomes of patients who underwent MIDCAB surgery in our institution. This was a retrospective, observational outcome study of retrospectively collected data. Data was collected using community, electronic, and paper medical records as well as telephone follow-up conversations with patients who underwent MIDCAB between December 1996 and June 2021. The primary outcome measure was mortality. Secondary outcomes included revascularization, myocardial infarction, and wound infection. Survival analysis was performed using the Kaplan–Meier method.
Results
A total of 215 patients were identified in the study period undergoing MIDCAB at our center. The median age was 77 years, and the cohort consisted of 180 (83.3%) of male patients. The median follow-up period was 16 years (12.1–17.7). At follow-up, freedom from repeat left anterior descending revascularization and from other vessels, revascularization was 96.7% and 89.1% respectively. Survival rates were 99.5%, 81.0%, and 45.2% survival at 1 year, 10 years, and 25 years respectively. Univariate analysis showed age (p < 0.01, Hazard ratio 1.08 confidence interval 1.05–1.11) and left ventricular function (p < 0.01, hazard ratio 2.40, confidence interval 1.66–3.45) as factors associated with mortality.
Conclusions
Our single-center experience of MIDCAB demonstrated excellent long-term freedom from revascularization and other complications. Although limited by the retrospective nature, the study shows MIDCAB to be a safe procedure for definitive revascularization of the left anterior descending coronary artery.
Similar content being viewed by others
Background
In the 1990s, with the observed success of minimally invasive surgery in several surgical specialties including general surgery, urology, and thoracic surgery, minimally invasive surgery (MIS) was gradually introduced into cardiac surgery with the goal of not only limiting incision but also limiting the use of cardiopulmonary bypass [1]. The first minimally invasive coronary artery bypass (MIDCAB) was performed in 1994 with a left internal mammary artery (LIMA) graft to the left anterior descending artery via a left-sided mini-thoracotomy [1, 2]. MIDCAB has been found to be an alternative to open coronary artery bypass graft (CABG) in a select group of patients [3,4,5]. The use of smaller incisions to perform CABG is surgically challenging, as there are difficulties in accessing an anastomosis site [6, 7]. For this reason, MIDCAB surgery is mostly indicated in patients with isolated single-vessel left anterior descending (LAD) disease [8,9,10]. In multivessel disease, it is only an option in patients undergoing hybrid revascularization [11]. Despite the relatively smaller select cohort of patients for which MIDCAB is indicated compared to conventional CABG surgery, MIDCAB has been established as an effective option for revascularization.
There are several methods by which optimal access can be achieved in MIDCAB surgery, either through small thoracotomy incision, mini sternotomies, thoracoscopically, endoscopically, or robot-assisted [3, 4, 12]. The thoracotomy approach involves making an incision in the left anterior fourth intercostal space and extending as appropriate to gain access to the left internal mammary artery (LIMA) graft and the pericardium [13]. Mini sternotomies on the other hand involve the use of a single midline skin incision, of about 5 cm to allow sternotomy from the fourth intercostal space downwards [13].
By use of these methods, MIDCAB surgery has been associated with reduced perioperative hemorrhage, lower incidence of surgical site infection, shorter hospital stays, and faster patient recovery [11, 14]. Birla et al. reported a significantly reduced length of hospital stay in MIDCAB (6.1 days) compared to open surgery (8.5 days) [14]. They also reported a reduced need for blood transfusion in the MIDCAB group (1.8 units) compared to the open surgery group (3.2 units) [14]. Several studies have demonstrated these short-term outcomes following MIDCAB; however, long-term outcomes of MIDCAB such as long-term freedom from repeat revascularization have not been extensively studied. With MIDCAB surgery having just emerged in the last three decades, it is important that its long-term outcomes are studied to ensure that long-term freedom from revascularization is comparable with that of open CABG. The aim of this study was to evaluate the immediate and long-term outcomes of patients who underwent MIDCAB surgery in our center.
Methods
Study design, population, and ethical approval
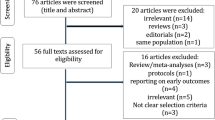
This was a retrospective observational study that reviewed data from patients who underwent MIDCAB surgery at our center, Royal Papworth Hospital, between December 1996 and June 2021. The study included all patients who underwent MIDCAB via a limited left anterior thoracotomy or mini sternotomy (lower midline sternotomy) in the time period. A total sample size of 215 patients met the eligibility criteria and were included in the study. Ethical approval of the Institutional Review Board (IRB) or equivalent ethics committee of the Royal Papworth Hospital, Cambridge, was waived as this is a retrospective study. Patient written consent for the publication of the study data was not required as the study was retrospective in nature and no identifiable information was disclosed.
Data collection
Patients’ data was collected through electronic and paper patient records. All available pre-operative patient data was reviewed to identify patients’ baseline characteristics. Outcome data were collected using electronic records as well as telephone follow-up conversations with patients and community records. Survival analysis was performed using the Kaplan–Meier method.
Outcomes
The primary endpoint of interest was overall mortality, with secondary outcomes including freedom from repeat revascularization, subsequent stroke, myocardial infarction (MI), and wound infection. Death was identified by the National Death Registry. The need for repeat revascularization was defined as any repeat coronary procedure either via percutaneous coronary intervention (PCI) or open CABG.
Statistical analysis
The baseline demographic and preoperative characteristics of the patients were summarised based on the total cohort and on the outcomes of interest using the appropriate summary statistics. Continuous variables with normal distribution were summarised with mean and standard deviation (SD) while those with skewed distribution were summarised with median and interquartile range (IQR). Categorical variables were summarised using counts and proportions. To test the difference in the baseline demographics between groups, the chi-squared test was used for categorical variables (with the Fisher exact test used if cell counts were less than 20) while the Welch’s unpaired t-test or Mann–Whitney U test was used for continuous variables, as appropriate. The Kaplan–Meier (KM) survival curves were constructed to visualize and evaluate the freedom from survival. The Cox-proportional hazard regression models were fitted to explore the association between the predictor variables and the overall survival outcomes. The level of significance for the analytical models was set at two-tailed p value < 0.05. All statistical analysis was done using R software (version 4.1.2GUI 1.77 High Sierra build (8007)).
Results
Baseline characteristics
A total of 215 patients were enrolled in the study who had MIDCAB (see Table 1). The majority, 180 (83.7%), were males. The median age of participants was 78.0 years (IQR 70–85 years) with the youngest patient being 36 years. There was no statistically significant difference in the age of participants among the sexes with males having a median age of 78.0 and females 78.5 (p = 0.67). The median follow-up period was 16 (11.85–17.70) years. The minimum and maximum follow-up time were 0.7 years and 25.2 years respectively. About three-quarters of the patients had good left ventricular function with only 8 (3.7%) of the cohort with poor left ventricular function. Also, 124 (57.6%) of the patients had New York Heart Association (NYHA) classification I with only 34 (15.8%) with NYHA III and above. The mean logistic EuroSCORE and EuroSCORE II were 3.88 ± 4.57 and 1.01 ± 0.43 respectively. There was, however, a significant amount of missing EuroSCORE data. This is because patients operated in the 1990s did not have a EuroSCORE recorded, as the logistic EuroSCORE was only developed in 1999 [15]. Due to the evolution of the score from the logistic EuroSCORE to EuroSCORE II, most subsequent patients had just one of the two scores recorded.
Survival rate and predictors of survival
Overall survival rate was 99.5% (95% confidence interval (CI) I 98.6–1.000) at 1 year, 81.1% (95% CI 75.7–86.8) at 10 years, 62.2% (9%% CI 55.1–70.3) at 20 years and 47.4% (95% CI 31.8–70.7) at 25 years (shown in Fig. 1). At the end of the follow-up period, mortality was recorded in 68 patients (31.6%). There was no difference in survival between males and females (HR 0.86. CI = 0.43–1.68, p = 0.66). Factors that were found to be predictive of survival were age, left ventricular function (p < 0.001) shown in Fig. 2, and Canadian Cardiovascular Society (CCS) class (p = 0.01).
As expected, univariate analysis showed increasing age (hazard ratio (HR) 1.08, 95% CI 1.05–1.11, p = < 0.001) to be predictive of overall mortality. For every 1-year increase in age, there was an 8% increased risk of death. Moderate left ventricular (LV) dysfunction (HR 2.52, 95% CI 1.49–4.26, P < 0.001) and severe LV function (HR 5.39, 95% CI 2.26–12.86, p < 0.001) were also shown to be predictive of mortality. Patients with moderate LV function had a 2.5 times increased hazard of death compared to patients with good LV function, while patients with severe LV function had a 5 times increased risk of death. Table 2 shows the relationship between the variables of interest and mortality.
Other outcomes of interest
A total of 11 patients had repeat revascularization, 3 patients (1.4%) had repeat LAD revascularization, 2 (0.9%) patients had repeat LAD and other vessel revascularization, and 6 patients (2.8%) had only repeat other-vessel revascularization. Repeat revascularization was via CABG in four patients and via PCI in six patients. One patient had a CABG following the initial MIDCAB for LAD disease and then a PCI to the RCA a few years later. At the end of the follow-up period, freedom from repeat revascularization was 93.3 (95% CI 96.6–100.0%) and 87.6% (95% CI 79.6–96.4%) at 25 years (illustrated in Fig. 3). Rate of freedom from repeat LAD revascularization was 96.7% (95% CI 93.9–99.6%), while rate of freedom from other-vessel revascularization was 89.4% (95% CI 81.4–98.0%).
There was no statistically significant difference in overall survival between patients who had repeat LAD revascularization and those who did not (HR 2.37, CI 0.57–9.80, p = 0.234). There was no difference in the rate of repeat LAD revascularization in patients with severe left ventricular function compared to those with good or moderate LVF (HR 1.43, CI 0.24–5.24, p = 0.63). Surgical site infection occurred in 11 (5.1%), with a majority being superficial wound infection (n = 9, 4.18%) and only 2 (0.93%) patients with deep wound infection needing debridement. At the end of the follow-up period, only 6 (2.8%) patients suffered from an MI. Table 3 shows the proportion of occurrence of other outcomes of interest.
Discussion
The results from our single-center study demonstrated good long-term outcomes following MIDCAB with mini lower sternotomy. Our survival rates were similar to those of the study done by Davierwala et al. in Germany [16]. Their study demonstrated a 66.1% and 55.6% survival at 15 years and 20 years respectively, close to the 67.5% and 62.2% shown in our study. In their study, their patients underwent MIDCAB via a left anterior small thoracotomy which differed from our cohort of patients who underwent MIDCAB via both lower mini sternotomy and left anterior small thoracotomy. Regardless of this slight difference in the population characteristics, the 15-year and 20-year survival was comparable in both cohorts of patients. Their study represents one of the largest population cohorts that reported on long-term outcomes following MIDCAB with over 2500 patients. Regardless of our smaller sample size, our study was still able to demonstrate the effectiveness of MIDCAB.
In another study, Raja et al. [17] compared MIDCAB and sternotomy for isolated LAD disease and reported an overall mortality of 22.4% in the MIDCAB group. This mortality was lower than that shown in our study, with a mortality of about 31.2%. In their study, however, their surgical approach involved the use of only left anterior thoracotomy incision which differed from ours, which included the use of both mini-sternotomy and left anterior thoracotomy. Also, their participants were much younger with a mean age of 63 years compared to the average age of 77 years in our own study. In addition to this, their 20-year follow-up period was much shorter than the longest 25-year follow-up period in our study, which could account for the higher mortality rate in our study. Though their study did not provide specific data on survival rates, they reported that there was no statistically significant difference in survival rates between the full sternotomy and MIDCAB groups.
Several studies have reported on short-term outcomes following MIDCAB. In the study by Martinovic [18], they reported the 1-year outcomes following MIDCAB via mini sternotomy. Like our study, they reported no in-hospital mortality, though they had a small sample size of 12 patients. Similarly, another study by Del Giglio et al. in Italy [19] reported on the short-term outcomes following MIDCAB. In their study, however, access was via an inferior J-shaped mini sternotomy. Though in our study, the mediastinotomy incision was longitudinal, our results are comparable.
In an earlier study done on our center by Farid et al. [13] reporting the 10-year outcomes following MIDCAB, they reported outcomes for all MIDCAB patients (both via the midline mini sternotomy approach and the left anterior thoracotomy). A survival rate of 84.8% and freedom from revascularization of 89.9% at 10 years were reported.
Comparing our results to other studies, we have shown that survival rates in patients undergoing MIDCAB are similar regardless of incision access type (thoracotomy, longitudinal mediastinotomy, or J-shaped mediastinotomy).
Following a quick database search, very limited data was seen to have reported on much longer time outcomes in patients who had MIDCAB via mini sternotomy. Our study has reported on this long-term outcome and has demonstrated that in patients who undergo MIDCAB, survival rate and freedom from revascularization are like those who had left anterior thoracotomy with excellent long term. These patients have good long-term survival and freedom from revascularization.
Limitations
One major limitation of our study was the relatively smaller sample size, as opposed to a larger sample size which increased the power of the study. Another limitation of the study was in the study design. Although the data for this study was prospectively collected, it was retrospectively analyzed. Thus, some variables of interest had missing data for some proportion of patients. There was also significant missing data on some comorbidities (such as hypertension, diabetes mellitus, and smoking) which could have served as confounders to the analysis. In addition, phone call conversations were used to collect data on long-term outcomes for some patients which were lost to follow-up. The data gathered using this method was subjective without methods of objective verification, and this could also serve as a limitation. The incidence rates of the outcomes of interest, especially revascularization may not have been complete.
Conclusions
Our single-center experience on mini-sternotomy MIDCAB demonstrated excellent long-term survival and freedom from revascularization over a median period of 16 years. Although limited by the retrospective nature, the study showed a trend toward MIDCAB as a safe procedure for definitive revasculariz.
ation. Further comparison with open CABG and other minimally invasive techniques, as well as hybrid revascularization and pump CABG, is required in future research to determine its relative safety and efficacy in larger populations.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CABG:
-
Coronary artery bypass graft surgery
- CCS:
-
Canadian Cardiovascular Society
- CI:
-
Confidence interval
- HR:
-
Hazard ratio
- IQR:
-
Interquartile range
- KM:
-
Kaplan-Meier
- LAD:
-
Left anterior descending
- LV:
-
Left ventricular
- LIMA:
-
Left Internal Mammary Artery Graft
- MIDCAB:
-
Minimally invasive coronary artery bypass
- MI:
-
Myocardial infarction
- MIS:
-
Minimally invasive surgery
- PCI:
-
Percutaneous Coronary intervention
- SD:
-
Standard deviation
References
Bonatti J, Wallner S, Crailsheim I et al (2021) Minimally invasive and robotic coronary artery bypass grafting—a 25-year review. J Thorac Dis 13(3):1922–1944. https://doi.org/10.21037/jtd-20-1535
Benetti FJ (1994) Uso de la toracoscopeia en cirugia coronaria para diseccion de la arteria mamaria interna. La Prensa Medica Argentina 81:877–879
Iribarne A, Easterwood R, Chan EY et al (2011) The golden age of minimally invasive cardiothoracic surgery: current and future perspectives. Future Cardiol 7(3):333–346. https://doi.org/10.2217/fca.11.23
Onan B (2020) Minimal access in cardiac surgery. Turk Gogus Kalp Damar Cerrahisi Derg 28(4):708–724. https://doi.org/10.5606/tgkdc.dergisi.2020.19614
Chiu KM (2013) Minimally invasive cardiac surgery. Formosan Journal of Surgery 46(6):183–188. https://doi.org/10.1016/j.fjs.2013.06.002
Langer NB, Argenziano M (2016) Minimally invasive cardiovascular surgery: incisions and approaches. Methodist Debakey Cardiovasc J 12(1):4–9. https://doi.org/10.14797/mdcj-12-1-4
Kayatta MO, Halkos ME, Narayan P (2018) Minimally invasive coronary artery bypass grafting. Indian J Thorac Cardiovasc Surg 34(Suppl 3):302–309. https://doi.org/10.1007/s12055-017-0631-x
Van Praet KM, Kofler M, Shafti TZN et al (2021) Minimally invasive coronary revascularisation surgery: a focused review of the available literature. Interv Cardiol 16:e08. https://doi.org/10.15420/icr.2021.05
Monica G, de Jong AR, Jacob KA et al (2022) Minimally invasive surgery or stenting for left anterior descending artery disease – meta-analysis. IJC Heart Vasc 2022(40):101046. https://doi.org/10.1016/j.ijcha.2022.101046
Repossini A, Di Bacco L, Nicoli F et al (2019) Minimally invasive coronary artery bypass: Twenty-year experience. J Thorac Cardiovasc Surg 158(1):127-138.e1. https://doi.org/10.1016/j.jtcvs.2018.11.149
Monsefi N, Alaj E, Sirat S (2023) Postoperative results of minimally invasive direct coronary artery bypass procedure in 234 patients. Front Cardiovasc Med 9:1051105. https://doi.org/10.3389/fcvm.2022.1051105
Mack M, Acuff T, Yong P (1997) Minimally invasive thoracoscopically assisted coronary artery bypass surgery. Eur J Cardiothorac Surg 12(1):20–24. https://doi.org/10.1016/S1010-7940(97)00141-3
Farid S, Ali JM, Stohlner V et al (2018) Long-term outcome of patients undergoing minimally invasive direct coronary artery bypass surgery: a single-center experience. Innovations (Phila). 13(1):23–28. https://doi.org/10.1097/imi.0000000000000466
Birla R, Patel P, Aresu G et al (2013) Minimally invasive direct coronary artery bypass versus off-pump coronary surgery through sternotomy. Ann R Coll Surg Engl 95(7):481–485. https://doi.org/10.1308/003588413X13629960047119
Nashef SAM, Roques F, Michel P et al (1999) European system for cardiac operative risk evaluation (EuroSCORE). Eur J Cardio-Thorac Surg 16(9):9–13. https://doi.org/10.1016/S1010-7940(99)00134-7
Davierwala PM, Verevkin A, Bergien L et al (2023) Twenty-year outcomes of minimally invasive direct coronary artery bypass surgery: The Leipzig experience. J Thorac Cardiovasc Surg 165(1):115-127.e4. https://doi.org/10.1016/j.jtcvs.2020.12.149
Raja SG, Garg S, Rochon M et al (2018) (2018) Short-term clinical outcomes and long-term survival of minimally invasive direct coronary artery bypass grafting. Ann Cardiothorac Surg 7(5):62127–62627. https://doi.org/10.21037/acs.2018.06.14
Martinovic I, Lindemann S, Irqsusi M et al (2019) Minimally invasive direct coronary bypass surgery via distal mini-sternotomy: promising clinical results with anaortic, multivessel, all-arterial technique. Herz 44(7):666–672. https://doi.org/10.1007/s00059-018-4696-0
Del Giglio M, Dell’Amore A, Aquino T et al (2008) Minimally invasive coronary artery bypass grafting using the inferior J-shaped ministernotomy in high-risk patients. Interact Cardiovasc Thorac Surg 7(3):402–405. https://doi.org/10.1510/icvts.2007.172973
Acknowledgements
The abstract of this paper was presented as a poster presentation at the 2023 Society of Cardiothoracic Surgery of Great Britain Meeting, 19th–21st March 2023, Birmingham, United Kingdom.
Funding
No funding to declare.
Author information
Authors and Affiliations
Contributions
OA, AD, SF, SN, and RDS were involved in the conceptualization of the research. OA and AD were involved in the design, data management, and data analysis and with the writing of the manuscript draft. SF, SN, and RDS were involved in the supervision of the research and review and editing of the manuscript draft. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Waived.
Consent for publication
Not applicable as no access to personalized patient information.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Akintoye, O., Divya, A., Farid, S. et al. Sixteen-year outcomes of patients undergoing minimally invasive direct coronary artery bypass surgery: a single-center experience. Cardiothorac Surg 32, 16 (2024). https://doi.org/10.1186/s43057-024-00135-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43057-024-00135-z