Abstract
Background
EuroSCORE stratifies surgical risk in cardiac surgery; however, it is not explicitly for tricuspid valve surgery. Therefore, we aimed to apply machine learning (ML) methods to predict operative mortality after tricuspid valve surgery and compare the predictive ability of these models to EuroSCORE.
This retrospective analysis included 1161 consecutive patients who underwent tricuspid valve surgery at a single center from 2009 to 2021. The study outcome was operative mortality (n=112), defined as mortality occurring within 30 days of surgery or the same hospital admission. Random forest, LASSO, elastic net, and logistic regression were used to identify predictors of operative mortality.
Results
EuroSCORE was significantly higher in patients who had operative mortality [8.52 (4.745–20.035) vs.4.11 (2.29–6.995), P<0.001] [AUC=0.73]. Random forest identified eight variables predicting operative mortality with an accuracy of 92% in the test set (age≥70 years, heart failure, emergency surgery, chronic kidney disease grade IV, diabetes mellitus, tricuspid valve replacement, hypertension, and redo surgery). The classification error rate in the training data was 9%, and in the testing data, it was 4.8%. Logistic regression identified eight variables with an AUC of 0.76. LASSO identified 13 variables with an AUC of 0.78, and elastic net identified 17 variables (AUC=0.795). The AUCs of the elastic net (P=0.048) and random forest (P<0.001) models were significantly higher than that of EuroSCORE.
Conclusions
ML effectively predicted TV surgery mortality more accurately than the traditional risk-scoring method. Incorporating ML in cardiac surgery risk scoring with comprehensive inclusion of all possible variables is recommended.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Machine learning (ML) is a discipline of artificial intelligence and data science that uses algorithms and models to learn from previous data and make the computer predict future events based on these data [1]. ML has achieved significant advancement in recent years and has been incorporated into the medical field for several purposes, including predicting disease diagnosis and prognosis [2, 3]. ML methods were implemented to predict surgery outcomes, and several ML methods’ performances were comparable to the available risk stratification methods [4,5,6]. EuroSCORE is one of the most commonly used risk-scoring systems in cardiac surgery and has proven accuracy [7]. Tricuspid valve surgery is associated with a higher risk than other cardiac procedures, which could be attributed to the disease, surgery, or patient characteristics [8]. The risk of tricuspid valve surgery varies widely in the literature because of the low volume of tricuspid valve surgery and the variability of the associated procedures [9]. EuroSCORE predicts mortality after cardiac surgery in general. The Society of Thoracic Surgeons (STS) cardiac surgery risk model and EuroSCORE II are not explicit for predicting outcomes after tricuspid valve surgery. ML could be superior to the traditional risk-scoring methods because of the high out-of-sample prediction. Therefore, we aimed to apply several ML methods, including shrinkage methods and decision trees, to predict operative mortality after tricuspid valve surgery and compare the predictive ability of these models to EuroSCORE II.
Methods
Design
This retrospective analysis included 1161 consecutive patients who underwent tricuspid valve surgery at a single tertiary referral center from 2009 to 2021. We included all tricuspid valve surgery, repair or replacement, isolated or concomitant with other cardiac procedures, and functional or organic tricuspid valve disease. The local ethical committee approved the study under approval number R21013 for data collection for tricuspid valve surgery projects.
Study data and definitions
The data included in this study were dichotomized to simplify the interpretation of the models. Age was dichotomized at 70 years old, and the cutoff point for dichotomizing body mass index (BMI) was 30 kg/m2. Anormal bilirubin was defined as levels ≥ 21 µmmol/L. Low ejection fraction (EF) was defined as EF of 40% or lower [10], and systolic pulmonary artery pressure was dichotomized at 50 mmHg [8]. Other variables included in the model were sex, hypertension, diabetes mellitus, chronic obstructive pulmonary artery disease (COPD), endocarditis, previous stroke, atrial fibrillation, chronic kidney disease (CKD) grade IV, New York Heart Association grade III-IV, history of heart failure within 1 year, moderate/severe right ventricular (RV) dysfunction, moderate/severe RV dilatation, emergency surgery, and reoperative surgery. Operative data included surgical urgency, TV repair or replacement, beating tricuspid valve surgery, and isolated tricuspid valve surgery.
CKD grade IV was defined as a creatinine clearance < 30 ml/min using the Cockcroft-Gault equation [11]. RV dilatation was diagnosed if the right ventricular basal diameter was >42 mm or the mid-level diameter was >35 mm. The severity of RV dysfunction was graded using tricuspid annular plane systolic excursion (TAPSE) measured in M-mode. Mild dysfunction was defined as TAPSE>20 mm, moderate dysfunction as TAPSE=15–20 mm, and severe dysfunction as TAPSE<15 mm [12, 13].
The study outcome was operative mortality (n= 112), defined as mortality occurring within 30 days of surgery or within the same hospital admission.
Secondary tricuspid regurgitation was the indication for tricuspid valve repair, and the indications for tricuspid valve replacement were failed previous repair, infective endocarditis, and degenerative tricuspid valve disease. Tricuspid valve repair was performed with annuloplasty rings (n= 927), De-Vega repair (n= 61), and one patient had biscuspidization. Annuloplasty prostheses used for repair were SMB50 band (Sovering MiniBand, SMB50, Sorin) (n=547), Duran band (Medtronic, Inc.) (n=210), MC3 (Edwards Lifesciences) (n=106), Tri-Ad (Medtronic ATS Medical Inc.) (n=49), Cosgrove-Edwards band (Edwards Lifesciences) (n=10), Contour 3-D (Medtronic Inc.) (n=4), and Simplici-T (Medtronic Inc.) was used in one patient. Mechanical valves were used in 20 patients, and biological valves in 139 patients. Coronary artery bypass grafting was performed concomitantly in 320 patients, aortic valve replacement in 247, and mitral valve surgery in 1040.
Data analysis
Descriptive analysis
For descriptive analysis, patients were grouped according to operative mortality into two groups: patients who survived (n= 1049) and those who had operative mortality (n= 112). Data are presented as numbers and percentages and were compared between surviving and non-surviving patients with the chi-squared test. The study included covariates with a small percentage of missing data. Missing data were due to documentation issues and unrelated to patients’ characteristics; therefore, they were considered missing completely at random and will not affect the analysis. Data analysis was performed using STATA 17 (Stata Corp, College Station, TX, USA).
Machine learning analysis
The study data were divided by random sampling into two sets: the training set (75%) and the testing dataset (25%). The analysis was performed on the training set, and the model’s performance was evaluated on the test dataset.
Random forest
All categorical variables listed in Table 1 were used to predict operative morality. Random forest with cross-validation was used to optimize testing accuracy and identify the optimal number of trees, tree depth, and splitting features. After identifying feature importance, recursive feature elimination was used to reach the minimum number of variables that achieve the same accuracy. The correlation between variables was visualized using a heat plot. The model was tested after eliminating the correlated variables, and the accuracy of the prediction was reported [14]. The analysis was performed using the Stata command (c_ml_stata_cv) that integrates scikit-learn, numpy, and pandas python packages [15].
Logistic regression
Multivariable logistic regression was used on the training set, and the final model was evaluated in the testing set with a cross-validated area under the curve (cvAUC) and k-fold receiver operator curves. Subset selection was performed using stepwise forward selection methods with a P value of 0.05 required for retaining the variables in the final model.
Shrinkage methods
Least absolute shrinkage and selection operator (LASSO) and elastic net with cross-validation were used to identify the most important variables for mortality prediction. Lambda was used as a tuning parameter for LASSO, and the best lambda associated with the lowest mean square error in the testing dataset was used Appendix. Cross-validation was used to identify the optimal alpha and lambda for the elastic net model. The deviance ratios in the training and testing sets were calculated. The analysis was performed using the Stata code (lasso logit).
Comparison with EuroSCORE
The AUCs of random forest, logistic regression, LASSO, and elastic net were plotted and compared with the AUC of EuroSCORE, and the P value was reported.
Results
Baseline characteristics
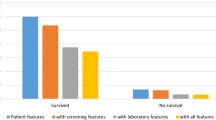
The operative mortality group had more patients aged ≥70 years, with a higher prevalence of diabetes mellitus, hypertension, endocarditis, COPD, history of heart failure, chronic kidney disease grade IV, moderate/severe RV dilatation, and dysfunction, reoperative surgery, isolated tricuspid valve surgery, and tricuspid valve replacement (Table 1).
The EuroSCORE was significantly higher in patients with operative mortality [8.52 (4.745–20.035) vs. 4.11 (2.29–6.995), P<0.001]. The correlation between all variables was visualized in the heat plot (Fig. 1).
Random forest classification
The optimal number of trees was 50, tree depth was 2, and splitting features was 3. The model that included all variables achieved a training accuracy of 90.5% and a testing accuracy of 90.4%. The classification error in the training set was 9.7%, and in the testing set, it was 8.6%. The feature importance of all variables is presented in Fig. 2A.
Recursive feature elimination was used to reach the minimum number of variables with the same accuracy. Progressive elimination of the features with minor importance was performed. In the final model, the number of trees was 150, the optimal depth was 8, and the splitting features were 3. The accuracy of the training data was 93%, and the testing data was 92%. The classification error rate in the training data was 9%, and in the testing data, it was 4.8%. The final model had eight variables (Fig. 2B).
Tricuspid valve replacement was correlated with chronic kidney disease (correlation r= 0.77) (Fig. 1). When removing the tricuspid valve replacement, the training accuracy was 91%, and the testing accuracy was 90%. The classification error rate in the training set was 8.4% and that in the test set was 10%.
Prediction of operative mortality using logistic regression, LASSO, and elastic net
Factors identified with logistic regression were age, hypertension, COPD, nonobese, heart failure, reoperative surgery, emergency surgery, and tricuspid valve replacement (Table 2). The model’s predictive power was assessed using cvAUC and 10-fold ROC curves with an AUC of 0.76 (Fig. 3).
LASSO identified 13 variables that can predict operative mortality (Table 3). The predictive power was assessed using the cvAUC and 10-fold ROC curves (AUC= 0.78) (Fig. 4).
Elastic net identified 17 variables that affected operative mortality (Table 3). The predictive power was assessed using the cvAUC and 10-fold ROC curves (AUC= 0.795) (Fig. 5). The deviance ratio was better in the test set in both lasso and ENET (the deviance ratio was 0.129 for both).
Comparison with EuroSCORE II
The observed mortality was 9.65% (95% CI 8.01–11.49). The predicted EuroSCORE II operative mortality was 6.58% (95% CI 6.16–7.01), and the predicted mortality in the test dataset with the random forest was 9.89% (95% CI 9.57–10.21). EuroSCORE II significantly predicted mortality [OR 1.11 (95% CI 1.06–1.15); P<0.001], and the AUC was 0.73. AUC nonsignificantly increased with logistic regression using our model compared to EuroSCORE II (P= 0.25) and nonsignificantly increased with LASSO (P= 0.057). The AUCs of the elastic net (P= 0.048) and random forest (P<0.001) models were significantly increased compared to EuroSCORE (Fig. 6).
Discussion
The application of machine learning to predict the outcomes after cardiac surgery is increasing [16]. Machine learning methods use training data to learn important features and make predictions on out-of-sample data. Additionally, several assumptions for ordinary statistical methods are not required for many ML methods, such as linearity, collinearity, and the limited number of variables introduced into the models. These features could make the predictive value of ML methods better than ordinary statistical tests such as multivariable regression for predicting the outcomes after surgical interventions. Nevertheless, the debate about the performance of ML methods compared to logistic regression is ongoing, with several studies reporting conflicting results [17]. Furthermore, ML methods have several drawbacks, such as the need for a large sample size, lack of interpretability, and the probability of overfitting the training data. In addition, there are several ML algorithms, and their prediction ability could vary widely and not be suitable for all datasets. However, a study reported comparable accuracy of ML algorithms in predicting cardiac surgery outcomes with a relatively smaller number of patients than those used in STS scoring [16]. Meanwhile, evaluation of the risk of every surgical cardiac procedure separately is required, especially after the wide use of transcatheter interventions [18].
This study evaluated ML methods in predicting operative mortality after tricuspid valve surgery. Operative mortality was defined as 30-day mortality or mortality occurring within the indexed hospitalization. Tricuspid valve surgery is relatively infrequent compared to other surgical procedures, and the current risk stratification with EuroSCORE or STS is not explicitly for predicting mortality after tricuspid valve surgery [7]. Additionally, several operative risk factors were not considered in risk stratification, such as valve repair vs. replacement, isolated vs. concomitant tricuspid valve surgery, and beating vs. arrested tricuspid valve surgery. In this analysis, we used parametric shrinkage methods to identify the most relevant factors (LASSO and elastic net), and we used the nonparametric random forest algorithm with recursive feature elimination. The random forest model achieved the best accuracy, and the model’s performance was better than that of EuroSCORE. The ability of the random forest to identify strong predictors could be affected by collinearity [19]. In this analysis, we found that the performance of random forest was not affected by the correlated variables. Darst and associates found that the presence of many correlated variables decreased the importance of causal variables [14]. They concluded that random forests might not be suitable for high-dimensional data.
Factors included in EuroScore II calculation were age, gender, chronic lung disease, extracardiac arteriopathy, poor mobility, previous cardiac surgery, active endocarditis, critical preoperative status, renal impairment, Canadian Cardiovascular Society (CCS) angina class 4, left ventricular function, recent myocardial infarction, pulmonary hypertension, NYHA class, surgery on thoracic aorta, the urgency of surgery, and concurrent procedures. Factors identified by LASSO were emergency surgery, COPD, age ≥ 70 years, reoperative surgery, hypertension, heart failure, moderate/severe right ventricular dysfunction, nonobese, tricuspid valve replacement, diabetes mellitus, grade IV chronic kidney disease, endocarditis, and pulmonary artery systolic pressure ≥ 50 mmHg. In addition to these factors, elastic net identified isolated tricuspid valve surgery, beating tricuspid valve surgery, NYHA III-IV, and moderate/severe right ventricular dilatation. Eight variables were identified using the random forest method: age ≥ 70 years, heart failure, emergency surgery, chronic kidney disease grade IV, diabetes mellitus, tricuspid valve replacement, hypertension, and redo surgery.
The mortality rate in our series is comparable to that in other studies. Dreyfus and associates studied 466 patients who underwent isolated tricuspid valve surgery for severe noncongenital tricuspid regurgitation at 12 French centers between 2007 and 2017, and the in-hospital mortality rate was 10% [8]. Chen’s and colleagues reported a perioperative mortality of 11.8% after isolated reoperative tricuspid valve replacement [20]. It has been shown that the hospital mortality rate is more than 35% in patients who undergo tricuspid valve replacement after previous tricuspid valve repair [21]. Albacker and colleagues reported 13% mortality after tricuspid valve replacement [22].
Age is the most robust risk factor for increased complications after cardiac surgery and the most frequent cause for deferring patients from surgery. The relationship between age and mortality is not linear and varies across surgical procedures [23]. In Chen’s study, the deceased patients were significantly older than the survivors by 10 years [20]. However, Topilsky and coworkers reported that early mortality was not associated with increased age, and age should not be considered in deciding surgery for symptomatic patients with severe tricuspid regurgitation [24]. In the Tri-Score for predicting mortality in isolated tricuspid valve surgery, age ≥ 70 years was a significant predictor of mortality, similar to our series [8].
Heart failure is a well-established predictor of postoperative mortality across many surgical specialties. Consequently, it is included in several risk prediction tools, such as the American College of Surgeons (ACS) Surgical Risk Calculator [25]. Additionally, preoperative low ejection fraction is a risk factor for increased morbidity and mortality after cardiac surgery [10]. Subbotina and associates demonstrated that preoperative severe right ventricular dysfunction was associated with acute preoperative and postoperative decompensations and poor outcomes after tricuspid valve surgery [26]. Additionally, the risk is increased in cases of biventricular dysfunction [20]. In the Tri-Score, the number of patients who were hospitalized for heart failure within 1 year was 163, and hospital mortality occurred in 25 (out of 48 total mortalities) [8]. Furthermore, NYHA functional classes III–IV were identified as predictors of morbidity and mortality after cardiac surgery [24, 27]. Among these variables, heart failure was identified in all models, RV dysfunction in the LASSO and elastic net models, NYHA III–IV and RV dilatation in the elastic net model only, and low ejection fraction did not appear in any of the risk models.
The risk of cardiac surgery increases substantially with repeated procedures. The operative techniques have improved recently, and together with the increased life expectancy, reoperative cardiac surgery has increased. Reoperative cardiac surgery could be associated with catastrophic complications, such as hemorrhage, which lead to increased morbidity and mortality [28]. Resternotomy complications are almost triple those of primary sternotomy [29]. When a reoperative tricuspid valve replacement is performed, mortality risk increases [30]. Right mini-thoracotomy could be the preferred incision for repeat sternotomy because of the lower complication rate compared to redo sternotomy [31]. In the Tri-Score, 33% of the mortality group had previous left-sided valve surgery, and previous surgery was a predictor for mortality [8].
Several investigators have reported that a higher risk of tricuspid valve replacement remains significant compared to valve repair and independent of other preoperative characteristics [22, 32]. In the Tri-Score, patients with tricuspid valve replacement had a higher mortality risk, as 69% of mortalities occurred in patients with replacement [8]. These results are comparable to other series [22]. Tricuspid valve replacement was identified as a risk factor in all our models. Aspects unique to tricuspid valve replacement should be thoroughly investigated to determine the contributing factors to mortality and whether they are disease- or technique-related.
COPD is a risk factor for morbidity and mortality after cardiac surgery [33]. COPD is already included in the EuroSCORE as a predictor of operative mortality; however, disease severity was not assessed [34]. In the Tri-Score, COPD was not a predictor of mortality, in contrast to our results [8]. COPD was a risk factor in the logistic regression, LASSO, and elastic net models but not in the random forest model. The effect of COPD may be more comprehensive if included as a severity stage.
Machine learning methods undergo continuous improvement. Despite their promising results, more research is required to validate their use in developing a risk score for predicting outcomes after cardiac surgery. Their role in developing a prediction score would replace the current traditional scoring methods.
Study limitations
The study has several limitations. This is a single-center experience, and the outcomes of tricuspid valve surgery could vary widely among centers. The external validity of our results should be confirmed in a multicenter study. Although we included preoperative and operative variables, there are several nonreported variables that could have affected the outcomes, such as the cardioplegia types [35] and TV prosthesis [36]. Although the study included patients who underwent tricuspid valve surgery, it included heterogeneous subgroups (repair vs. replacement and isolated vs. concomitant tricuspid valve surgery). A large sample size is required to improve the accuracy of machine learning prediction, and future studies on more selective cohorts will yield a prediction model specific to each group with improved prediction accuracy. We included abnormal bilirubin level as a covariate in the analysis; however, other scores indicative of hepatic dysfunction and known to be associated with increased mortality after surgical procedures, such as MELD and Child-Pugh scores, were not evaluated in this study. We encourage the performance of future studies that incorporate several unusually recorded variables related to the hemodynamic status, laboratory results, and operative times.
Conclusions
Machine learning methods effectively predict operative mortality following tricuspid valve surgery with high accuracy compared to traditional risk-scoring methods using EuroSCORE II. The incorporation of machine learning methods in cardiac surgery risk scoring with comprehensive inclusion of all possible variables is recommended.
Availability of data and materials
The authors declare that the data supporting the findings of this study are not available per hospital-related regulations.
Abbreviations
- ACS:
-
American College of Surgeons
- AUC:
-
Area under the curve
- CCS:
-
Canadian Cardiovascular Society
- CKD:
-
Chronic kidney disease
- COPD:
-
Chronic obstructive pulmonary disease
- ML:
-
Machine learning
- NYHA:
-
New York Heart Association
- RV:
-
Right ventricle
- STS:
-
Society of Thoracic Surgeons
- TAPSE:
-
Tricuspid annular plane systolic excursion
- TV:
-
Tricuspid valve
References
Choi RY, Coyner AS, Kalpathy-Cramer J, Chiang MF, Campbell JP (2020) Introduction to machine learning, neural networks, and deep learning. Transl Vis Sci Technol 9(2):14
Deo RC (2015) Machine learning in medicine. Circulation 132(20):1920–30
Arfat Y, Mittone G, Esposito R, Cantalupo B, DE Ferrari GM, Aldinucci M (2022) Machine learning for cardiology. Minerva Cardiol Angiol 70(1):75–91
Zhou N, Ji Z, Li F, Qiao B, Lin R, Jiang W et al (2022) Machine learning-based personalized risk prediction model for mortality of patients undergoing mitral valve surgery: the PRIME score. Front Cardiovasc Med 9:866257
Jiang H, Liu L, Wang Y, Ji H, Ma X, Wu J et al (2021) Machine learning for the prediction of complications in patients after mitral valve surgery. Front Cardiovasc Med 8:771246
Kilic A, Goyal A, Miller JK, Gleason TG, Dubrawksi A (2021) Performance of a machine learning algorithm in predicting outcomes of aortic valve replacement. Ann Thorac Surg 111(2):503–10
Nashef SAM, Roques F, Sharples LD, Nilsson J, Smith C, Goldstone AR et al (2012) EuroSCORE II†. Eur J Cardio-Thoracic Surg 41(4):734–45. https://doi.org/10.1093/ejcts/ezs043
Dreyfus J, Audureau E, Bohbot Y, Coisne A, Lavie-Badie Y, Bouchery M et al (2022) TRI-SCORE: a new risk score for in-hospital mortality prediction after isolated tricuspid valve surgery. Eur Heart J 43(7):654–62
Topilsky Y, Khanna A, Tourneau T Le, Park S, Michelena H, Suri R, et al. Clinical context and mechanism of functional tricuspid regurgitation in patients with and without pulmonary hypertension. Circ Cardiovasc Imaging. 2012;5(3):314–23. Available from: https://www.ahajournals.org/doi/abs/https://doi.org/10.1161/CIRCIMAGING.111.967919
Arafat AA, Alawami MH, Hassan E, et al (2023) Surgical vs Transcatheter Aortic Valve Replacement in Patients With a Low Ejection Fraction. Angiology 74(7):664–671. https://doi.org/10.1177/00033197221121012
Chen TK, Knicely DH, Grams ME (2019) Chronic kidney disease diagnosis and management: a review. JAMA. 322(13):1294–304
Di Mauro M, Foschi M, Tancredi F, Guarracini S, Di Marco M, Habib AM, et al. Additive and independent prognostic role of abnormal right ventricle and pulmonary hypertension in mitral-tricuspid surgery. Int J Cardiol. 2018;252:39–43. Available from: https://www.sciencedirect.com/science/article/pii/S0167527317349902
Algarni KD, Arafat A, Algarni AD, et al (2021) Degree of right ventricular dysfunction dictates outcomes after tricuspid valve repair concomitant with left-side valve surgery. Gen Thorac Cardiovasc Surg 69(6):911–918. https://doi.org/10.1007/s11748-020-01536-7
Darst BF, Malecki KC, Engelman CD (2018) Using recursive feature elimination in random forest to account for correlated variables in high dimensional data. BMC Genet 19(Suppl 1):65
Cerulli G (2022) Machine learning using Stata/Python. Stata J 22(4):772–810. https://doi.org/10.1177/1536867X221140944
Park J, Bonde PN (2022) Machine learning in cardiac surgery: predicting mortality and readmission. ASAIO J 68(12):1490–500
Penny-Dimri JC, Bergmeir C, Perry L, Hayes L, Bellomo R, Smith JA (2022) Machine learning to predict adverse outcomes after cardiac surgery: a systematic review and meta-analysis. J Card Surg 37(11):3838–45
Almedimigh AA, Albabtain MA, Alfayez LA, Alsubaie FF, Almoghairi A, Alotaiby M et al (2023) Isolated surgical vs. transcatheter aortic valve replacement: a propensity score analysis. Cardiothorac Surg 31(1):2. https://doi.org/10.1186/s43057-022-00094-3
Gregorutti B, Michel B, Saint-Pierre P (2017) Correlation and variable importance in random forests. Stat Comput 27(3):659–78. https://doi.org/10.1007/s11222-016-9646-1
Chen C, Ge M, Ye J, Cheng Y, Chen T, Lu L et al (2020) The risk and outcomes of reoperative tricuspid valve replacement surgery. Heart Surg Forum 23(5):E658-64
Bernal JM, Morales D, Revuelta C, Llorca J, Gutiérrez-Morlote J, Revuelta JM (2005) Reoperations after tricuspid valve repair. J Thorac Cardiovasc Surg 130(2):498–503
Albacker TB, Arafat AA, Alotaibi AM, Alghosoon H, Algarni KD (2023) Mechanical Tricuspid Valves Have Higher Rate of Reintervention: A Single Center Experience. Ann Thorac Cardiovasc Surg 29(2):78–85. https://doi.org/10.5761/atcs.oa.22-00086
Afilalo J, Steele R, Manning WJ, Khabbaz KR, Rudski LG, Langlois Y et al (2016) Derivation and validation of prognosis-based age cutoffs to define elderly in cardiac surgery. Circ Cardiovasc Qual Outcomes 9(4):424–31
Topilsky Y, Khanna AD, Oh JK, Nishimura RA, Enriquez-Sarano M, Jeon YB et al (2011) Preoperative factors associated with adverse outcome after tricuspid valve replacement. Circulation 123(18):1929–39
Lerman BJ, Popat RA, Assimes TL, Heidenreich PA, Wren SM (2019) Association between heart failure and postoperative mortality among patients undergoing ambulatory noncardiac surgery. JAMA Surg 154(10):907–14
Subbotina I, Girdauskas E, Bernhardt AM, Sinning C, Reichenspurner H, Sill B (2017) Comparison of outcomes of tricuspid valve surgery in patients with reduced and normal right ventricular function. Thorac Cardiovasc Surg 65(8):617–25
Chen J, Abudupataer M, Hu K, Maimaiti A, Lu S, Wei L et al (2018) Risk factors associated with perioperative morbidity and mortality following isolated tricuspid valve replacement. J Surg Res 221:224–31
Rupprecht L, Schopka S, Keyser A, Lunz D, Sossalla S, Hilker M et al (2022) 25 years’ experience with redo operations in cardiac surgery-third-time sternotomy procedures. Thorac Cardiovasc Surg 70(5):377–83
Bianco V, Kilic A, Gleason TG, Aranda-Michel E, Habertheuer A, Wang Y et al (2020) Reoperative cardiac surgery is a risk factor for long-term mortality. Ann Thorac Surg 110(4):1235–42
Jeganathan R, Armstrong S, Al-Alao B, David T (2013) The risk and outcomes of reoperative tricuspid valve surgery. Ann Thorac Surg 95(1):119–24
Kwon Y, Park SJ, Kim HJ, Kim JB, Jung S-H, Choo SJ et al (2022) Mini-thoracotomy and full-sternotomy approach for reoperative mitral valve surgery after a previous sternotomy. Interact Cardiovasc Thorac Surg 34(3):354–60
Topilsky Y (2015) Indications for surgery for tricuspid regurgitation. Interv Cardiol (London, England). 10(1):58–60
Pieri M, Belletti A, Monaco F, Pisano A, Musu M, Dalessandro V et al (2016) Outcome of cardiac surgery in patients with low preoperative ejection fraction. BMC Anesthesiol 16(1):97
Saleh HZ, Mohan K, Shaw M, Al-Rawi O, Elsayed H, Walshaw M et al (2012) Impact of chronic obstructive pulmonary disease severity on surgical outcomes in patients undergoing non-emergent coronary artery bypass grafting. Eur J cardio-thoracic Surg Off J Eur Assoc Cardio-thoracic Surg. 42(1):108–13 (discussion 113)
Arafat AA, Hassan E, Alfonso JJ, Alanazi E, Alshammari AS, Mahmood A et al (2021) Del Nido versus warm blood cardioplegia in adult patients with a low ejection fraction. Cardiothorac Surg 29(1):24. https://doi.org/10.1186/s43057-021-00061-4
Algarni KD, Alfonso J, Pragliola C, Kheirallah H, Adam AI, Arafat AA (2021) Long-term outcomes of tricuspid valve repair: the influence of the annuloplasty prosthesis. Ann Thorac Surg 112(5):1493–500
Acknowledgements
Not applicable
Funding
No funding was received for this project. This research did not receive any grants from funding agencies in the public, commercial, or non-profit sectors.
Author information
Authors and Affiliations
Contributions
AAA: study design, analysis, interpretation, drafting, and revising; SA: data collection, drafting, and critical revision, MMA, study design, supervision, and revising the manuscript; AIA: study design, revision, and supervision; HI: data interpretation and revising; CP: supervision, design, revision, and critical appraisal; MAA: study design, supervision, and critical appraisal. The authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
IRB approval number: R21013. Prince Sultan Cardiac Center, Riyadh, Saudi Arabia, 2021. Consent to participate was waived by the Ethical Committee.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Arafat, A.A., Alamro, S., AlRasheed, M.M. et al. Applying machine learning methods to predict operative mortality after tricuspid valve surgery. Cardiothorac Surg 31, 16 (2023). https://doi.org/10.1186/s43057-023-00107-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43057-023-00107-9