Abstract
Background
Ileocolic intussusception is a rare condition that is difficult to diagnose. A pathological lead point, usually malignant, is often the cause of adult intussusception. In emergency scenarios, radiologists must be able to identify this entity and its causes and express their opinions on associated complications.
Case presentation
The hospital's emergency room admitted a 75-year-old woman who was suffering from intermittent abdominal pain and constipation. An abdominal contrast-enhanced computed tomography revealed a long giant ileocolic intussusception. Considering the clinical stability and the absence of signs of complications on CT, the patient did not undergo an urgent surgical procedure but underwent a colonoscopy the following day. Surprisingly, the colonoscopy highlighted the spontaneous resolution and revealed the presence of the three tumour lead points in the cecum and ascending colon. A CT was performed after the colonoscopy, confirming the intussusception's resolution. The surgeon performed a right oncological hemicolectomy. The malignant lead points on histological examination were moderate to poorly differentiated adenocarcinomas.
Conclusions
A giant and long ileocolic intussusception with a long embedded visceral segment (the python colon sign) could suggest pathological lead points in the cecum and ascending colon. Despite the large size, a spontaneous resolution of the python colon is possible. In this scenario, even if, on imaging, it is impossible to macroscopically identify a lead point, in cases of giant and long ileocolic intussusceptions, every effort must be undertaken to search for the cause of the intussusception.
Similar content being viewed by others
Background
Ileocolic or colocolic intussusception is a rare condition less common to intussusception of the small intestine [1]. Nearly 90% of adult cases of intussusception have a pathological lead point (generally malignant in the large bowel and benign in the small one) [2].
Without specific signs, physicians usually require imaging to make a diagnosis. Abdominal CT, with the renowned bowel-within-bowel configuration, is the most accurate radiological modality for diagnosing intussusception in adults [2].
Adult intussusception begins with a lead point, which serves as a focal point of traction, drawing the proximal bowel within the distal one beyond the neoplastic bowel situs. The intussuscepted segment's continued peristaltic contractions cause the symptoms [3]. With continued invagination and oedema, the vascular flow to the bowel becomes compromised, resulting in ischaemia to the affected segment, which, if not treated, can lead to necrosis and perforation. Understanding the imaging spectrum of intussusception and its associated pathological lead points is critical for recognising and treating these patients [3].
Preoperative imaging can be challenging in establishing the diagnosis of ileocolic intussusception and its complications.
This case presents some CT findings that facilitate a prompt diagnosis of this uncommon condition.
We consider, to the best of our knowledge, our case a unique case because it describes a voluminous and long ileocolic portion swallowed up to the mid-distal transversus similar to a giant python that has swallowed a voluminous prey which surprisingly resolved spontaneously, caused by three malignant leads points. Therefore, the uniqueness of the case presented, in our opinion, lies in the exceptional length of the intussusception and the surprising spontaneous resolution. Therefore, we speculate that multiple lead points, rather than just one, may contribute to generating giant intussusceptions. Therefore, searching for more than one pathological lead point is necessary.
Case presentation
A 70-year-old woman came to our hospital's emergency room with nausea, vomiting, 24 h of generalised intense and intermittent abdominal pain, and constipation over the past two days. The patient showed no signs of peritonism. The patient's medical and surgical history was nonspecific. The patient exhibited typical vital signs and body temperature. Laboratory tests indicated a white blood cell count of 9500 cells/mm3 and a haemoglobin count of 12 g/dL. There were no further particular findings.
An abdominal contrast-enhanced computed tomography revealed a long giant ileocolic intussusception, about 30 cm, with mechanical obstruction and three tumour masses of the ascending colon, the ileocecal valve and the cecum (Figs. 1, 2, and 3).
Contrast-enhanced abdominal CT scan showing a heterogeneous abdominal soft tissue mass: A: Coronal view shows the ileocolonic intussusception as a sausage-shaped lesion (green arrowheads). Asterisk in A, E and F represents the cecum and the terminal ileum with the respective mesentery, invaginated inside the mid-proximal transverse colon. The blue arrowheads in B, D, E and F represent the arterial and venous mesenteric vessels that accompany the invaginated intestine into the lumen of the colon. Target sign (orange arrowhead) in D on axial view as a typical sign of bowel intussusception. Entrance of the intussusception (green arrow in C) on axial CT images in the shape of a “mushroom”. The yellow arrowheads in the coronal CT images in A represent the areas of neoplastic tissue that are the lead points responsible for intussusception
A Gate of intussusception or mouth of the python where vessels, loops and mesenteric structures converge at the entrance as they sink. B Giant and long ileocolic intussusception with the downstream colon of normal calibre simulating the condition in which a python has swallowed a large part of a prey swelling proximally
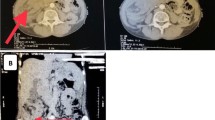
Due to the stability of the clinical conditions and the absence of signs of perforation, necrosis, or vascular compromise, the patient was a candidate for a colonoscopy the day following the night of hospitalisation to confirm the radiological appearance of intussusception ileocolic. The following day, surprisingly, the colonoscopy highlighted the spontaneous resolution of the extended intussusception ileocolic and confirmed the presence of the three tumour lead points in the cecum and proximal ascending colon. A few hours after the colonoscopy, the medical team performed an unenhanced CT scan and confirmed the resolution of the giant ileocolic intussusception (Fig. 4). The colonoscopy confirmed the tumour lead points, and the patient was a candidate for the dedicated oncological surgery procedure.
An unenhanced CT scan performed a few hours after the colonoscopy (coronal planes A and B; axial plane D) showed the resolution of the giant ileocolic intussusception. Yellow arrowheads in A, B, C and D) indicate that intussusception unoccupied the transverse colon. The green arrows in A, B, and D in the coronal and axial images indicate that the caecum and ascending colon are still oedematous but without residual intussusception. A small effusion layer (asterisk in A, B and D) surrounds the cecum and terminal ileum. The contrast-enhanced CT examination performed four days after resolution of the intussusception (coronal image in C) demonstrates (blue arrowhead) the tumour lead point of the cecum with conspicuous enhancement
A right oncological hemicolectomy and lymph node dissection were performed (Fig. 2). The hospital discharged the patient without complications ten days after surgery.
On histological examination, the malignant lead points revealed moderate to poorly differentiated adenocarcinomas, one of which had diffuse mucinous aspects, with ulcerated aspects and infiltration of the visceral wall up to the muscular layer. The three malignant lead points showed dimensions of 4.5, 3 and 1.5 cm, respectively; no metastatic lymph nodes accompanying tumours.
Discussion
Intussusception in adults is rare, accounting for less than 5% of all cases of intussusception and 1–2% of bowel obstructions [4].
Children commonly experience intussusception, which presents with cramping abdominal pain, bloody diarrhoea, and a palpable tender mass. It can affect any part of the gastrointestinal tract but is most commonly associated with the small intestine. Unlike children, nearly 90% of adult cases have a pathological malignant or benign lead point [1, 2, 5].
Ileocecal intussusception can start with a lead point in the colon, ileum, or appendix [1]. The lead point may reside within the lumen of the bowel, within the wall, or outside the wall; in 60% of cases, the lead point is a tumour, malignant, or benign, while in the other 40%, it is related to adhesions or phlogistic and inflammatory conditions [6].
Traditionally, academics categorise intestinal intussusception into four subtypes based on its point of origin, extension, and propagation. Type 1, called the enteric type (49.5%), is confined to the involvement of only the small intestine; in type 2, i.e. the ileocolic type (29.1%), the ileum invaginates into the colon without invagination of the vermiform appendix; in type 3, i.e. the ileocecal type (13%) sees the cecum and ileum completely invaginated into the ascending colon, while in type 4, the colo-colonic type (19.9%), it is limited to involving the colon or the rectum [6, 7].
Imaging is typically necessary when specific signs are absent because the condition is associated with various other diagnoses.
The abdominal CT is the most frequently used radiological modality for diagnosing intussusception in adults [2], with sensitivity ranges from 58 to 100%, depending on the series reviewed providing answers to important questions such as location, lesion type, vascular compromise, and process extent [7,8,9].
There are three distinct patterns of intussusception, depending on the seriousness and course of the disease [8, 9]: the target-like appearance for the earliest stage, the sausage-shaped, and pseudokidney if a vascular compromise occurs [9]. The classic “sausage sign” and “target sign,” which have alternating low and high attenuation areas, are generated by the layered overlap of the bowel wall, mesenteric fat, and intestinal lumen contents [10].
The pseudokidney CT pattern indicates wall oedema and thickening with vascular compromise. Loss of the layers pattern, perivisceral fluid collection, and bowel perforation may indicate intestinal necrosis, a severe consequence of intussusception [9, 10].
Although CT is highly effective in identifying an intussusception, demonstrating the typical signs that allow for an accurate diagnosis, CT cannot always identify the cause of intussusception [10, 11]. Furthermore, the possibility of measuring the length of the intussusception that CT offers is significant as short intussusceptions can self-resolve and, on the contrary, as can be imagined, the more involved and deeper ones are predisposed to more severe complications and, therefore, require rapid surgical management [11,12,13].
While transient intussusception cases are typically characterised by a short segment (2–3.5 cm) without obstruction and can be managed conservatively without surgery, it is worth noting that in adults, approximately 65% are caused by neoplasms, with a slightly higher rate observed in intussusceptions involving the colon [10, 13].
As reported in full in the conclusions of the work by Lvoff et al. [13], there is a cut-off of interception length, which acts as a watershed in the wait-and-see or operational management of these patients; they specifically contend that the length of intussusception plays a crucial role in differentiating between the majority of small-bowel intussusceptions identified through CT scans that resolve on their own and the minority that necessitate surgical intervention. An intussusception with a less than 3.5 cm measurement usually resolves spontaneously without surgical intervention. Patients, whether symptomatic or asymptomatic, can experience spontaneous reduction of intussusceptions. [10]. Surgical resection should be contemplated only as a final resort regarding therapeutic options. Treatment should be customised based on the patient's comorbidities, clinical status, and likelihood of malignancy [14, 15].
Our case appears particularly interesting because it describes the spontaneous resolution of a giant and very long ileocolic intussusception. However, at the same time, it highlights how the abdomen contrast-enhanced CT could identify the malignant lead points responsible for the pathological intussusception.
CT appearance of an intussusception depends on several factors, including the amount of invaginated mesenteric fat, the possible presence of single or multiple lead points, benign or malignant, their shape and volume, and the degree of intestinal wall oedema. Contrast-enhanced CT can distinguish between lead point and non-lead point intussusception. Although there may be considerable similarity in the CT findings, differentiation can be achieved by identifying a leading mass separate from the oedematous bowel [16,17,18].
Conclusions
Adult intussusception is always difficult to diagnose. Radiologists, particularly with the increasing use of abdomen CT in emergencies, must be prepared to correctly identify this entity, determine its causes, and express their opinions on associated complications. Patients with vascular compromise, necrosis, or perforation require emergency surgery, whereas in cases where no complications are present and the risk of malignancy is shallow, a watchful waiting approach may be recommended. The sign of the python colon could suggest the presence of pathological lead points. Therefore, if identified, even if the CT scan does not demonstrate possible lead points or if the intussusception resolves spontaneously, every effort must be undertaken to search for the cause of the intussusception.
Availability of data and material
Available on request.
Abbreviations
- CT:
-
Computed tomography
References
Gollub MJ (2011) Colonic intussusception: clinical and radiographic features. AJR Am J Roentgenol 196(5):W580–W585. https://doi.org/10.2214/AJR.10.5112
Augustin D, Gérald J, Lafontant GF, Joseph O, Zidor EM (2022) Transient colonic intussusception versus colon adenocarcinoma: a case report on ultrasound features in the emergency department. Cureus 14(10):e30710
Marsicovetere P, Ivatury SJ, White B, Holubar SD (2017) Intestinal intussusception: etiology, diagnosis, and treatment. Clin Colon Rectal Surg 30(1):30–39
Minaya Bravo AM, Vera Mansilla C, Noguerales Fraguas F, Granell Vicent FJ (2012) Ileocolic intussusception due to giant ileal lipoma: Review of literature and report of a case. Int J Surg Case Rep 3(8):382–384
Marinis A, Yiallourou A, Samanides L, Dafnios N, Anastasopoulos G, Vassiliou I, Theodosopoulos T (2009) Intussusception of the bowel in adults: a review. World J Gastroenterol 15(4):407–411
Panzera F, Di Venere B, Rizzi M, Biscaglia A, Praticò CA, Nasti G, Mardighian A, Nunes TF, Inchingolo R (2021) Bowel intussusception in adult: prevalence, diagnostic tools and therapy. World J Methodol 11(3):81–87. https://doi.org/10.5662/wjm.v11.i3.81.PMID:34026581;PMCID:PMC8127421
Gupta RK, Agrawal CS, Yadav R, Bajracharya A, Sah PL (2011) Intussusception in adults: institutional review. Int J Surg 9(1):91–95. https://doi.org/10.1016/j.ijsu.2010.10.003
González-Carreró Sixto C, Baleato-González S, García Palacios JD, Sánchez Bernal S, Junquera Olay S, Bravo González M, García FR (2023) Intestinal intussusception in adults: location, causes, symptoms, and therapeutic management. Radiologia (Engl Ed) 65(3):213–221. https://doi.org/10.1016/j.rxeng.2022.10.005
Baleato-González S, Vilanova JC, García-Figueiras R, Juez IB, Martínez de Alegría A (2012) Intussusception in adults: what radiologists should know. Emerg Radiol 19(2):89–101. https://doi.org/10.1007/s10140-011-1006-z
Park SB, Ha HK, Kim AY, Lee SS, Kim HJ, Park BJ, Jin YH, Park SH, Kim KW (2007) The diagnostic role of abdominal CT imaging findings in adults intussusception: focused on the vascular compromise. Eur J Radiol 62(3):406–415. https://doi.org/10.1016/j.ejrad.2007.01.003
Al-Radaideh AM, Omari HZ, Bani-Hani KE (2018) Adult intussusception: a 14-year retrospective study of clinical assessment and computed tomography diagnosis. Acta Gastroenterol Belg 81(3):367–372
Warshauer DM, Lee JK (1999) Adult intussusception detected at CT or MR imaging: clinical-imaging correlation. Radiology 212:853–860
Lvoff N, Breiman RS, Coakley FV, Lu Y, Warren RS (2003) Distinguishing features of self-limiting adult small-bowel intussusception identified at CT. Radiology 227:68–72
Álvarez-Bautista FE, Moctezuma-Velázquez P, Pimienta-Ibarra AS, Vergara-Fernández O, Salgado-Nesme N (2023) Adult intussusception: still a challenging diagnosis for the surgeon. Rev Gastroenterol Mex (Engl Ed) 88(4):315–321. https://doi.org/10.1016/j.rgmxen.2022.06.009
Moniakis AA, Flamourakis ME, Gkionis IG, Giakoumakis MI, Tsagkataki ES, Kazamias GM, Spiridakis KG, Christodoulakis MS (2021) Ileocolic intussusception in a woman: a case report and literature review. Am J Case Rep 8(22):e933341
Kim YH, Blake MA, Harisinghani MG, Archer-Arroyo K, Hahn PF, Pitman MB, Mueller PR (2006) Adult intestinal intussusception: CT appearances and identification of a causative lead point. Radiographics 26(3):733–44
Chiu HT, Yen H, Weng YS, Chen CY, Lin KH, Chen PH, Jhou HJ, Pu TW (2022) Combined ileoileal and ileocolic intussusception secondary to inflammatory fibroid polyp in an adult: a case report. Medicina (Kaunas) 58(2):310
Zanni M, Vaccari S, Lauro A, Marino IR, Cervellera M, D’Andrea V, Tonini V (2021) Bleeding edge therapy: ileocolic intussusception due to ileocecal valve adenocarcinoma and its management in an adult patient-case report and literature review. Dig Dis Sci 66(5):1436–1440
Acknowledgements
None
Funding
Dr Totaro was co-funded by Next Generation EU, in the context of the National Recovery and Resilience Plan, Investment PE8 – Project Age-It: “Ageing Well in an Ageing Society”. This resource was co-financed by the Next Generation EU [DM 1557 11.10.2022]. The views and opinions expressed are only those of the authors and do not necessarily reflect those of the European Union or the European Commission. Neither the European Union nor the European Commission can be held responsible for them.
Author information
Authors and Affiliations
Contributions
AP contributed to conceptualisation, supervision, investigation, and writing—original draft. BFPA, PM, AV, RC, and TB performed investigation. PO and GT performed supervision. AT contributed to conceptualisation, supervision, and writing—original draft. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study does not require institutional review board approval.
Consent for publication
Informed consent was obtained for the case report to be published.
Competing interests
None of the authors have any relevant conflict of interest or industry support related to this report.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pierro, A., Apollonio, B.F.P., Mirco, P. et al. Antegrade long giant ileocolic intussusception via colon–cecum cancer lead points: case report with focus on the sign of the python colon. Egypt J Radiol Nucl Med 55, 121 (2024). https://doi.org/10.1186/s43055-024-01291-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-024-01291-2