Abstract
Background
Intussusception in adults is a rare cause of abdominal pain that is often associated with organic pathology. We describe a case of ileocolic intussusception revealing a cecal adenocarcinoma in a young woman successfully managed by laparoscopic-assisted surgery adhering to oncological principles.
Case presentation
A 30-year-old woman with a family history of colon adenocarcinoma in a young brother presented to our emergency department with a 2-month history of intermittent colicky abdominal pain accompanied by nausea and vomiting. Physical examination showed a palpable mass in the right lower quadrant of the abdomen. Computed tomography showed a 3-layered structure giving the characteristic target-shaped appearance in the ascending colon, highly suggestive for an ileocolic intussusception associated with right colic parietal thickening and an adjacent lymphadenopathy.
Patient was planned for laparoscopic exploration and eventually definitive surgery. Intra-operatively, we found an ileocolic intussusception with thickening of the colic wall and slight proximal intestinal dilation. Multiple lymphadenopathies along the ileocecal artery were observed. Laparoscopic right hemicolectomy was performed following strict oncologic principles with “en bloc resection” and lymphadenectomy given the risk of an underlying malignancy. Considering this risk, previous reduction of the invaginated segments was not attempted and primary extracorporeal anastomosis was performed using manual sutures.
Macroscopic examination of the resected specimen revealed a tumor mass of the caecal wall .The histological analysis identified a moderately differentiated tubular adenocarcinoma invading the serosa (T3) without permeation of the lymphatic or venous capillaries .No lymphatic metastasis of 28 nodes removed was seen. Postoperative course was uneventful and patient was discharged 5 days after surgery.
Postoperative chest, abdomen, and pelvis CT scan were normal .Therefore, tumor is classified as stage II A (T3N0 M0).There was loss of MLH2 and MSH6 protein expression on immunohistochemistry findings reflecting a microsatellite instability phenotype, and the patient was followed up without adjuvant chemotherapy.
Conclusion
Ileocolic intussusception rarely revealed a cancer in young adults. Laparoscopic surgery has a special interest in the diagnosis and treatment in this pathology. Oncogenetic consultation should be required in malignant lesion.
Similar content being viewed by others
Background
Intussusception in adults is a rare cause of abdominal pain. Unlike its pediatric counterpart, intussusception in adults is often associated with organic pathology. We describe a case of ileocolic intussusception revealing a cecal adenocarcinoma in a young woman successfully managed by laparoscopic-assisted surgery adhering to oncological principles.
Case presentation
A 30-year-old woman with a family history of colon adenocarcinoma in a young brother presented to our emergency department with a 2-month history of intermittent colicky abdominal pain accompanied by nausea and vomiting. She denied any history of gastrointestinal bleeding, fever, or past abdominal surgery. Her appetite was good but she reported a 3-kg weight loss during the previous 3 months. Physical examination showed a palpable mass in the right lower quadrant of the abdomen, but digital rectal examination was unremarkable. This mass was firm, non-tender, and slightly painful with limited mobility, but no signs of peritoneal reaction were evident. All laboratory investigations, particularly tumor markers including carcinoembryonic antigen (CEA) and carbohydrate antigen (CA 19.9) were within the normal limits.
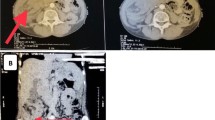
Ultrasound revealed a prominent swelling of the intestinal wall with target signs and a hyperechoic mass over the right lower quadrant area. An abdominal computed tomography (CT) was carried out to confirm the ultrasound findings. This showed a three-layered structure giving the characteristic target-shaped appearance in the ascending colon, highly suggestive for an ileocolic intussusception (Fig. 1). Additionally, the CT showed a right colic parietal thickening with an adjacent lymphadenopathy measuring 11 × 13 mm but without signs of intestinal obstruction. Moreover, complete colonoscopy with exploration of the caecal region was paradoxically normal.
Patient was planned for laparoscopic exploration and eventually definitive surgery. Intra-operatively, we found an ileocolic intussusception with thickening of the colic wall and slight proximal intestinal dilation. In addition, multiple lymphadenopathies along the ileocecal artery were observed, but no signs of intestinal ischemia or peritoneal carcinosis were noted. Consequently, we performed a laparoscopic right hemicolectomy (Fig. 2) following strict oncologic principles with “en bloc resection” and lymphadenectomy given the risk of an underlying malignancy. Considering this risk, previous reduction of the invaginated segments was not attempted. The specimen was exteriorized through a 5-cm incision in the right upper quadrant, and primary extracorporeal anastomosis was performed using manual sutures.
Macroscopic examination of the resected specimen revealed a tumor mass of the caecal wall measuring 4 × 5 × 4 cm and occupying more than 3-quarters of the circumference (see Fig. 3). The histological analysis identified a moderately differentiated tubular adenocarcinoma invading the serosa (T3) without permeation of the lymphatic or venous capillaries. Mucinous component was estimated at 40 %.No lymphatic metastasis of 28 nodes removed was seen and surgical margin was negative for cancer. Postoperative course was uneventful and patient was discharged 5 days after surgery.
Postoperative chest, abdomen, and pelvis CT scan were normal .Therefore, tumor is classified as stage II A (T3N0 M0). Microsatellite status and immunohistochemistry of four deoxyribonucleic acid (DNA) mismatch repair proteins, including mutL homologue 1, post meiotic segregation increased 2, mutS homologue 2, and mutS homologue 6, were checked.
There was loss of MLH2 and MSH6 protein expression on immunohistochemistry findings reflecting a microsatellite instability phenotype (Fig. 4), and the patient was followed up without adjuvant chemotherapy.
Microscopic findings and immunohistochemistry for deoxyribonucleic acid mismatch repair proteins (×200). The tumor is a moderately differentiated adenocarcinoma with immunohistochemical expression of mutL homologue 1 (MLH1) and postmeiotic segregation increased 2 (PMS2) and loss of immunohistochemical expression of mutS homologue 2 (MSH2) and mutS homologue 6 (MSH6) reflecting a microsatellite instability phenotype
Discussion
Intussusception is an uncommon disease in the adult population compared with that in children [1]. First described by Barbette in 1674, it is defined as the telescoping of a proximal segment of the gastrointestinal tract within the lumen of an adjacent segment [2]. The exact mechanism is still unknown, and it is believed that any lesion in the bowel wall or irritant within the lumen that alters normal peristaltic activity is able to initiate invagination. Unlike in children, the clinical presentation of adult intussusception is considerably various and non-specific. Most patients present with intermittent or chronic symptoms that are suggestive of incomplete intestinal obstruction. The classic pediatric triad of abdominal pain, palpable abdominal mass, and bloody stool is rarely seen [1, 3, 4].
The accuracy of computed tomography for diagnosis of adult intussusception is better than that of other examinations, including abdominal ultrasonography, barium enema study, and colonoscopy [5]. Typical features include the “target” or “sausage-shaped” mass seen at the axial and coronal view, respectively, or the appearance of bowel-within-bowel configuration with or without fat and mesenteric. The CT scan may also define the location, the nature of the mass, its relationship to surrounding tissues and additionally, it may help in disease staging in malignancy causes [6] and exploration of no specific or acute abdominal pain [7].
In this case, a preoperative diagnosis of intussusception was easily made by conventional imaging techniques including ultrasonography and CT scan despite longstanding digestive symptoms, but colonoscopy did not show the intussusception. Preoperative diagnosis of intussusception is infrequent in the adult with a rate reported to range from 32 to 70 % [8].
The optimal therapeutic management of adult intussusception remains controversial due to the differing etiology between pediatric and adult populations. A pathologic lesion is found in 90 % of adult intussusception cases [9]. Primary colon adenocarcinoma and malignant lymphoma were the two most common underlying malignant lesions [10]. Therefore, surgical exploration and bowel resection is generally recommended. However, reduction of intussusception prior to resection is deemed unsafe, considering the risk of an underlying malignancy more likely in the colic invaginations. The downsides of reduction prior to resection include the theoretical risk of intralumenal tumor seeding, reduction of externally viable bowel despite mucosal necrosis, venous embolization of malignant cells, spillage of succus through inadvertent perforation, and anastomotic complication in cases of an edematous and weakened bowel [4]. In our patient, some data suspected a malignant tumor such as: lymphadenopathy, colic parietal thickening, young age, and family history. Reducing the intestine before resection of the bowel was not performed.
Conventionally, laparotomy should be considered for the treatment. Given that laparoscopic management of pediatric intussusception has been available for some time [11] and that the long-term safety of laparoscopic resection for colorectal cancer is well established, laparoscopic-assisted surgery currently appears to be an attractive alternative to laparotomy in selected patients. This procedure entails mobilization and delivering the specimen with an extracorporeal anastomosis in most patients. This requires utmost care and an experienced laparoscopic surgeon.
We herein describe a laparoscopic treatment for adult colonic intussusception caused by cecum carcinoma. In the present case, laparoscopic right hemicolectomy was successfully performed. The experience gained in the present case suggests that laparoscopy may be a diagnostic or therapeutic tool for selected cases of young adult intussusception.
The histological examination showed a cecal adenocarcinoma stage II A according to the TNM classification, for which the indication of adjuvant chemotherapy is subject of controversy. Our patient presented more favorable prognostic factors such that: tumor was pT3, moderately differentiated and without angiolymphatic, or perineural invasion. Node dissection was optimal, and surgical margins were negative. Microsatellite was instable, and patient can be spared adjuvant chemotherapy [12].
Finally, many items are in favor of a lynch syndrome according to BETHESDA criteria; colon cancer was diagnosed before the age of 50 years, with one first-degree relative with an HNPCC-related tumor diagnosed under age 50 years. The abundant mucus is presented, and microsatellite was an instable phenotype with loss of expression of MSH2 and MSH 6 which often reflects a germline mutation and therefore an HNPCC. Lynch syndrome is suspected, and cancer genetics consultation is required [13].
Conclusions
Ileocolic intussusception rarely revealed a cancer in young adults. It can detect a genetic predisposition. Laparoscopic surgery has a special interest in the diagnosis and treatment in this pathology. Oncogenetic consultation should be required in a malignant lesion.
Consent
Written informed consent was obtained from the patient for publication of this Case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Abbreviations
- CA 19.9:
-
carbohydrate antigen
- CEA:
-
carcinoembryonic antigen
- CT:
-
computed tomography
- DNA:
-
deoxyribonucleic acid
- HNPCC:
-
Hereditary non polyposis colorectal cancer
- MLH:
-
mutL homologue
- MSH:
-
mutS homologue
- TNM:
-
tumor nodes metastasis
References
Zubaidi A, Al-Saif F, Silverman R. Adult intussusception: a retrospective review. Dis Colon Rectum. 2006;49:1546–51 [PubMed].
Marinis A, Yiallourou A, Samanides L, Dafnios N, Anastasopoulos G, Vassiliou I, et al. Intussusception of the bowel in adults: a review. World J Gastroenterol. 2009;15:407–11 [PubMed].
Morera-Ocon FJ, Hernandes-Montes E, Bernal-Sprekelsen JC. Intestinal invagination in adults: presentation of a case and a review of the Spanish literature. Cir Esp. 2009;86:358–62. doi:10.1016/j.ciresp.2009.08.002 [PubMed].
Azar T, Berger D. Adult intussusception. Ann Surg. 1997;226:134–8. doi:10.1097/00000658-199708000-00003 [PubMed].
Erbil Y, Eminoglu L, Cais A, Berber E. Ileocolic invagination in adults due to caecal carcinoma. Acta Chir Belg. 1997;97:190–1.
Barussaud M, Regnet N, Briennon X, Kerviler BD, Pessaux P, Sharhi NK, et al. Clinical spectrum and surgical approach of adult intussusceptions: a multicentric study. Int J Colorectal Dis. 2006;21:834–9. doi:10.1007/s00384-005-0789-3 [PubMed].
Yamada H, Morita T, Fujita M, Miyasaka Y, Senmaru N, Oshikiri T. Adult intussusception due to enteric neoplasms. Dig Dis Sci. 2007;52:764–6 [PubMed].
Wang N, Cui XY, Liu Y, Long J, Xu YH, Guo RX, et al. Adult intussusception: a retrospective review of 41 cases. World J Gastroenterol. 2009;15:3303–8 [PubMed].
Eisen LK, Cunningham JD, Aufses AH. Intussusception in adults: institutional review. J Am Coll Surg. 1999;188:390–5 [PubMed] [Ref list].
Chiang JM, Lin YS. Tumor spectrum of adult intussusception. J Surg Oncol. 2008;98:444–7. doi:10.1002/jso.21117 [PubMed].
Bonnard A, Demarche M, Dimitriu C, Podevin G, Varlet F, François M, et al. GECI (Groupe d'Etude de Coelioscopie Pédiatrique). Indications for laparoscopy in the management of intussusception: a multicenter retrospective study conducted by the French Study Group for Paediatric Laparoscopy (GECI). J Pediatr Surg. 2008;43:1249–53 [PubMed] [Ref list].
Saridaki Z, Souglakos J, Georgoulias V. Prognostic and predictive significance of MSI in stages II/III colon cancer. World J Gastroenterol. 2014;20(22):6809–14 [PubMed].
Umar A, Boland CR, Terdiman JP, et al. Revised Bethesda guidelines for hereditary nonpolyposis colorectal cancer (Lynch syndrome) and microsatellite instability. J Natl Cancer Inst. 2004;96:261–8 [PubMed].
Acknowledgements
We thank Meryem Derai (Department of Radiology, Mohammed V military teaching hospital of Rabat) for her assistance in the acquisition of the scanner image.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
CE and MT conceived of the idea and drafted the manuscript. CE, MT and MR K did the research and data collection. MT, ME, and AAA performed the surgical procedure and did patient surgical follow-up. CE and RT did patient oncological follow-up. FK performed the histopathological examinations. HE and MI have contributed in supervision and guidance of the manuscript. All authors read and approved the final version of the manuscript.
Mohamed Tarchouli, Mohamed Reda Khmamouche, Rachid Tanz, Mohammed Elfahssi, Fouad Kettani, Abdelmounaim Ait Ali, Hassan Errihani and Mohammed Ichou contributed equally to this work.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Elm’hadi, C., Tarchouli, M., Khmamouche, M.R. et al. Intestinal intussusception in a young women: unusual cause and specific management. World J Surg Onc 13, 252 (2015). https://doi.org/10.1186/s12957-015-0660-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12957-015-0660-0