Abstract
Background
Dynamic contrast-enhanced magnetic resonance imaging (DCE-MRI) is the important tool in breast imaging. However, two major limitations are represented by its specificity and by the injection of contrast material. Diffusion weighted imaging (DWI) provides important functional information without the need for contrast material. A newly introduced diffusion weighted imaging with background suppression (DWIBS) sequence is an accurate and rapid tool for the identification and characterization of breast lesions, with its short examination time, high lesion-to-background contrast and lack of need for intravenous contrast agents.
Objective
To assess the role of DWIBS sequence in the evaluation of indeterminate and suspicious breast masses and to compare its accuracy with DCE-MRI in correlation with histopathological findings.
Methods
Thirty-five patients were included in the study, referred from sono-mammography clinic to MRI unit for further MRI assessment of probably benign, suspicious and malignant looking breast masses (BIRADS 3, BIRADS 4 & BIRADS 5) on sono-mammography imaging results. MRI breast protocol which included DCE-MRI and DWIBS sequences were obtained for characterization and were verified by core needle biopsy or excisional biopsy. The results were statistically analyzed. Sensitivity, specificity, diagnostic accuracy (DA), positive predictive value (PPV) and negative predictive value (NPV) were calculated for DCE-MRI and DWIBS. Apparent diffusion co-efficient (ADC) values were calculated with ADC ≤ 1.2 × 10−3 mm2/s was considered suspicious for malignancy. The results were then compared with the histological findings.
Results
Thirty-five female patients had 39 breast masses included in our study. By DCE-MRI, 8 (20.5%) masses were categorized as benign and 31(79.5%) masses were categorized as malignant. By DWIBS sequence, 7 (17.9%) masses were categorized as benign and 32 (82.1%) masses were categorized as malignant. By histopathology, 14 (35.9%) masses were benign and 25 (64.1%) masses were malignant. DCE-MRI obtained accuracy, sensitivity, specificity, PPV and NPV values of 84.6, 100, 57.1, 80.6 and 100%, respectively. DWIBS sequences obtained accuracy, sensitivity, specificity, PPV and NPV values of 82.1, 100, 50, 78.1and 100%, respectively.
Conclusions
DWIBS can be added to DCE-MRI, as complementary tool to make radiologist more confident about the diagnosis. It can also be used instead of DCE-MRI sequences in certain circumstances such as in cases of renal impairment.
Similar content being viewed by others
Background
Female breast cancer is the most common invasive cancer to affect females worldwide, and is also the second leading cause of cancer death among women [1]. Diagnosis of breast cancer patients in the early stages is one of the important aspects of breast cancer therapy [2].
Dynamic contrast-enhanced magnetic resonance imaging (DCE-MRI) is an important tool in breast imaging. Together with morphological criteria, it depends on the differential enhancement between normal and malignant tissue to improve lesion characterization. This is believed to be due to increased neo-angiogenesis and tissue permeability to contrast agent within malignant lesions [3].
However, two major limitations are present: Its specificity which ranges from 37 to 97% and the injection of contrast material which increases the acquisition time and costs and may be associated with various reactions or the rare nephrogenic systemic fibrosis syndrome in patients with impaired renal function. These limitations have been overcome by diffusion weighted imaging (DWI). DWI provides important functional information without the need for contrast material. The combination of DCE-MRI with DWI improves the specificity of breast MRI compared to DCE-MRI alone [4].
Diffusion-weighted MRI (DWI) visualizes and assesses the random thermal motion (Brownian motion) of water molecules, providing qualitative (the restricted diffusion regions appear as hyper-intense areas) and quantitative (the apparent diffusion coefficient (ADC) value) information about their diffusion within tissue, makes it capable of distinguishing breast lesions from the surrounding normal tissue and to differentiate benign from malignant breast lesions [5].
An important limitation of DWI imaging is represented by respiratory motion which decreases spatial resolution. Therefore, the acquisition of images in apnea or synchronized to a particular phase of the respiratory cycle is strictly recommended. The synchronization to the respiratory cycle improves the signal-to-noise ratio, but results in an increase of scan time [5].
Breath hold scanning only allows obtaining thick-sliced (usually 8–10 mm) diffusion weighted images with relatively low signal-to-noise ratio [6].
In order to overcome this discomfort, Takahara et al. introduced a new technique named DWIBS, which stands for diffusion-weighted whole body imaging with background body signal suppression. The suppression of background body signal, which is the adipose tissue in case of the breast, allows to increase the detection rate of glandular lesions by using free breathing scan [5].
DWIBS is an improved DWI technique, offering heavy diffusion weighting (with b values up to 1500 s/mm2), enhanced STIR (Short TI Inversion Recovery) fat suppression and the possibility of free breathing. This results in reduced scan times and movement artifacts with subsequent good quality examinations allowing thin slices (typically 4–5 mm) to be obtained [7].
The use of DWIBS approach is thought to reduce the rate of unnecessary biopsies from false mammography results without the need for a lengthy MRI procedure or the need for IV contrast administration [8].
Aim of the study
To assess the role of DWIBS sequence in the evaluation of indeterminate and suspicious breast masses and to compare its accuracy with DCE-MRI in correlation with histopathological findings.
Methods
Thirty five patients were included in the study with ages ranging from 28 to 71 years, referred from sono-mammography clinic to MRI unit for further MRI assessment of probably benign, suspicious and malignant breast masses (BIRADS 3, BIRADS 4& BIRADS 5) on sono-mammography imaging results.
The study was accepted by the local ethical committee of our institution. Full history taking and clinical examination were done. Complete renal function tests including (serum creatinine level & eGFR) were obtained. All patients then underwent breast MRI which included DCE-MRI and DWIBS sequences using dedicated breast coil. The results were then correlated with the histopathological findings.
Inclusion criteria were adult female gender (> 18 years) and patients who had breast masses (BIRADS 3, BIRADS 4& BIRADS 5), the imaging results of indeterminate, suspicious and malignant lesions were verified by core needle biopsy or excisional biopsy.
Exclusion criteria were patients having contraindications for MRI, e.g. Metal implants as cochlear implants, Cardiac defibrillators, pacemakers or claustrophobia. Patients known to have severe allergy to contrast material and with acute kidney injury or chronic renal disease were also excluded (elevated serum creatinine level more than 1.8 or e GFR less than 30 ml/min/1.73m2).
Patient preparation included fasting of the patients for 6 h before imaging, and informing them about a detailed explanation of the imaging procedure with obtaining written consent. The premenopausal women were examined on day 6–13 of the menstrual cycle in order to reduce the risk of false positives. Insertion of wide bore (18–20 g) IV cannula was done.
Method of MRI examination
-
Machine used:
The study was done in MRI unit on Philips Ingenia machine 1.5 Tesla.
-
Patient position:
The patient was positioned prone, using a special breast coil, on the MRI table. We ensured that both breasts were fit entirely within the coil.
-
MRI protocol:
-
Morphological sequences were performed in multiple projections, including pre-contrast axial T1-weighted images, axial T2- weighted images and axial STIR. All these sequences were single shot spin echo with flip angle 90°.
-
DWI study was performed for all cases with 2 b-values (0 and 750 s/mm2). ADC values were measured for all masses, as part of the routine breast MRI protocol of our institute.
-
DWIBS images were taken in all patients, using the parameters of TR/TE/TI = 6,900/70/180 ms; with 3-mm slice thickness and without gaps.
-
Dynamic contrast-enhanced MRI was performed after injection of a bolus of gadolinium, in a dose of 0.1 mmol/kg, using an automated injector at a rate of 3–5 ml/s. Contrast injection was followed by saline bolus injection (total of 20 ml at 3–5 ml/s). Dynamic study consisted of 1 pre contrast and 5 post-contrast series.
-
-
The procedure duration was about 30–40 min.
Image analysis
MRI with DWIBs was interpreted and analyzed by 2 different radiologists (of 7 and 11 years' experience) with full analysis of all sequences to assess the mass regarding the shape (oval, rounded, irregular), margins(circumscribed, not circumscribed) and degree of signal intensity in both T1 and T2 and STIR, with the addition of DWIBS findings. Then blindly of the non-contrast results, the same patients were analyzed using the post-contrast information in the form of enhancement characteristics (homogenous or heterogeneous), dynamic enhancement curve (kinetic curves). DWIBS images were assessed and the presence or absence of diffusion restriction was recorded, and finally compared with post-contrast images findings.
There were three types of time–intensity curves: Type I (persistent uptake), where a persistent increase in signal intensity was present beyond 2 min after contrast agent injection. Type II (plateau), where the maximum signal intensity was obtained in the first 2 min and then remained fairly constant. Type III (rapid washout), where the maximum signal intensity was obtained in the first 2 min and then decreased over time. Type I is often found in benign lesions. Type III is often found in malignant lesions.
Statistical analysis
Data were gathered, revised, coded and entered to the Statistical Package for Social Science (IBM SPSS) version 23. The quantitative data were displayed as mean, standard deviations and ranges for parametric. Also qualitative variables were displayed as number and percentages. The comparisons between groups with qualitative data were performed by using Chi-square test. The comparisons between two groups with quantitative data and parametric distribution were performed by using Independent t-test. Receiver operating characteristic curve (ROC) was used in the quantitative form to set sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and Area under curve (AUC) of ADC value to predict malignant results with pathology. Receiver operating characteristic curve (ROC) was used in the qualitative form to set sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and accuracy. The p-value < 0.05 was considered significant.
Results
-
All patients were females only, with an age range of 27 28–71 years; mean age ± standard deviation (SD), 50.31 ± 11.52 years).
-
Six patients were complaining of discomfort (15.8%), four with nipple discharge (10.5%), and twenty five complained of a palpable lump (73.7%).
-
Out of 35 patients, 11 (31.4%) had positive family history of breast cancer and 24 (68.6%) had negative family history of breast cancer.
-
All patients had breast masses (BIRADS 3 (28.2%), BIRADS 4 (28.2%) & BIRADS 5(43.6%) on imaging results.
-
Thirty-nine breast masses were detected in 35 patients. 24 masses (61.5%) were in right breast and 15 masses (38.5%) were in left breast.
-
Out of the 39 masses, 14 (35.9%) were histo-pathologically proven to be benign and 25 (64.1%) were histo-pathologically proven to be malignant.
On pre contrast T2WI images
Morphologic criteria
Out of the 25 malignant lesions, 19 lesions (76.0%) were not circumscribed (irregular or speculated) on T2 WI and 6 lesions (24.0%) were circumscribed. Out of the 14 benign lesions, 6 lesions (42.9%) were not circumscribed on T2WI and 8 lesions (57.1%) were circumscribed.
This indicates a significant increase in the association of non-circumscribed shape with malignant lesions (Fig. 1), and circumscribed shape with benign lesions (p< 0.05).
A 42-year-old female, complaining of right breast palpable lump. a–c Right breast irregular speculated mass with perilesional edema and intramammary LN seen on T2WIs (a), with heterogeneous post-contrast enhancement (b), showing peripheral diffusion restriction on DWIBS (c). Its ADC value was 0.7 × 10−3 mm2/s. It was pathologically proved to be invasive duct carcinoma of the right breast
On contrast enhanced images
Pattern of enhancement
Out of the 25 malignant lesions, 16 lesions (64.0%) showed heterogeneous enhancement on CE-MRI and 9 lesions (36.0%) showed homogenous enhancement on DCE-MRI.
Out of the 14 benign lesions, 4 lesions (28.6%) showed heterogeneous enhancement on CE-MRI and 10 lesions (71.4%) showed homogenous enhancement on DCE-MRI.
This indicates a significant increase in the association of heterogeneous enhancement pattern with malignant lesions (Figs. 1, 2), and homogenous enhancement pattern with benign lesions (p<0.05).
A 71-year-old female, complaining of right breast palpable lump. a–c Right breast malignant irregular mass seen on T2WIs (a), with heterogeneous post-contrast enhancement (b), showing diffusion restriction on DWIBS (c). Its ADC value was 1.1 × 10−3 mm2/s. It was pathologically proved to be invasive duct carcinoma (grade 2) of the right breast
Enhancement kinetics
Out of the 25 malignant lesions, 24 lesions showed suspicious enhancement kinetics (type II (52.0%) and type III (44.0%) kinetic curves), and 1 lesion showed type I kinetic curve (4.0%).
Out of the 14 benign lesions, 2 lesions only showed suspicious enhancement kinetics; type II (14.3%) kinetic curve, and 12 lesion showed type I kinetic curve (85.7%).
This indicates a highly significant increase in the association of suspicious enhancement kinetics (type II and type III kinetic curves) with malignant lesions and type I enhancement kinetic curve with benign lesions (p < 0.01).
The DCE-MRI imaging results were compared to the histopathology results, and then sensitivity, specificity, PPV, NPV and accuracy of DCE-MRI were calculated (Table 1).
On DWIBS imaging
Out of the 25 histopathologically malignant lesions, 25 lesions showed diffusion restriction (100.0%).
Out of the 14 histopathologically benign lesions, 7 lesions showed no diffusion restriction (50.0%) (Fig. 3), and 7 lesions showed diffusion restriction (50.0%).
A 68-year-old female, has left mastectomy, complaining of discomfort. a–c A case of right fibroadenoma seen on T2WIs (a), with homogenous post-contrast enhancement (b), showing non-restricted diffusion on DWIBS (c). Its ADC value was 1.3 × 10−3 mm2/s. There is right short linear non-mass enhancement that is relatively suspicious, with no definite correlate could be seen in mammography or ultrasound and due to unavailability of MRI guided biopsy, short-term follow-up after six months was advised, which was stationary and stable on follow-up
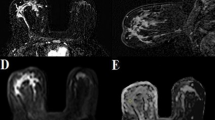
This indicates a highly significant increase in the association of diffusion restriction on DWIBS imaging with malignant lesions (Figs. 4, 5) (p < 0.01).
A 45-year-old female, complaining of right breast palpable lump. a–c Right breast malignant irregular two masses seen on T2WIs (a), with heterogeneous post-contrast enhancement (b), showing diffusion restriction on DWIBS (c). Its ADC value was 0.8 × 10−3 mm2/s and 0.7 × 10−3 mm2/s. It was pathologically proved to be multicentric invasive lobular carcinoma of the right breast. Left breast regular mass seen on T2WIs (a), with heterogeneous post-contrast enhancement (b), showing diffusion restriction on DWIBS (c). Its ADC value was 1.2 × 10−3 mm2/s. It was pathologically proved to be metastatic intra-mammary LN of left breast
A 44-year-old female, complaining of discomfort. a–c Right breast malignant irregular mass seen on T2WIs (a), with homogenous post-contrast enhancement (b), showing diffusion restriction on DWIBS (c). Its ADC value was 0.8 × 10−3 mm2/s. It was pathologically proved to be infiltrating lobular carcinoma of the right breast
The DWIBS imaging results were compared to the histopathology results, and then sensitivity, specificity, PPV, NPV and accuracy of DWIBS were calculated (Table 2).
The ADC value
The mean ADC value was 1.32 ± 0.32 × 10−3 mm2/s for benign lesions and 0.98 ± 0.23 × 10−3 mm2/s for malignant ones. The difference between the ADC values of benign and malignant lesions was statistically highly significant (p < 0.01) (Table 3).
Diagnostic validity test revealed that the best cut-off value to differentiate benign from malignant lesions was 1.2 × 10−3 (Table 4).
We obtained false-positive results for seven lesions showed restricted diffusion on DWIBS (Fig. 6), and six lesions on DCE-MRI, but no false negative results were found on DWIBS and DCE-MRI.
A 50- year-old female, complaining of right breast palpable lump. a–c Right breast irregular mass seen on T2WIs (a), with homogenous post-contrast enhancement (b), showing diffusion restriction on DWIBS (c). Its ADC value was 1.1 × 10−3 mm2/s. It was pathologically proved to be fibroadenoma of the right breast (false positive)
Discussion
In our study, we assessed the role of DWIBS in categorization of breast masses. There were 35 patients included with 39 masses detected. All underwent DCE-MRI with DWIBS sequences and results were correlated with histopathology.
In our study, DCE-MRI had overall accuracy of 84.6% when compared to histopathological results. It showed sensitivity of 100%; ability to detect all malignant lesions. Specificity of the DEC-MRI was 57.1%; ability to distinguish non-malignant lesions. It showed NPV of 100% and PPV of 80.6%.
In our study, DWIBS sequences had overall accuracy of 82.1% when compared to histopathological results. It showed sensitivity of 100%; ability to detect all malignant lesions. Specificity of the DWIBS was 50%; ability to distinguish non-malignant lesions. It showed NPV of 100% and PPV of 78.1%.
The DWIBS derived ADC map has shown a highly significant decrease in the mean ADC value associated with malignant lesions. The cut-off value obtained from our study was 1.2 × 10−3 at which it showed sensitivity of 92.0% and specificity of 57.14%.
In our study, DWIBS did not have a superior result to DCE-MRI as regards the specificity, accuracy and PPV, but minimal differences between them. They both have comparable sensitivity and NPV.
So, DWIBS can be added to DCE breast MRI as complementary tool to make radiologist more confident about the diagnosis. It can be useful in certain cases of renal impairment.
The study done by Bickelhaupt et al., [8] published in 2016 conducted over 50 patients with suspicious breast lesions on screening mammography reported results that the DWIBS was superior to DCE-MRI, regarding sensitivity 92%, specificity 94%, NPV 92% and PPV 93%, while DCE-MRI had sensitivity 85%, specificity 90%, NPV 87% and PPV 89%. Our study disagrees with it, DWIBS is not superior to DCE-MRI in our study, regarding specificity and PPV. These different results could be explained by our selection of patients where we included patients with probably benign, indeterminate and suspicious (BIRADS III–IV and V) sono-mammography results.
We agree with another study published in 2014 by Marco Moschetta et al., [5] which has closer results to our study. Ninety patients were evaluated by DCE-MRI and DWIBS sequences. By comparing DWIBS images with DCE-MRI data, no difference was found. DWIBS sequences obtained sensitivity, specificity, DA, PPV and NPV values of 100, 82, 87, 68 and 100%, respectively.
Stadlbauer et al., [9] in study published in 2009 conducted over 50 patients with 36 lesions detected in 30 patients, and reported results that the DWIB was superior in the detection and visualization of both malignant and benign lesions in the breast with sensitivity 94% and specificity 100%. We agree with this study regarding the sensitivity (100%), but disagree with it regarding the specificity (50%). These different results could be explained by the fact that the histopathological types of the lesions included in our study were limited to IDC, ILC, fibroadenomas and lymph nodes, but Stadlbauer et al. revealed wide range of histopathological types.
Our study showed closer results to the study done by Keriakos et al., [10] published in 2017 included 46 female, as DWIBS had a high sensitivity 87.5% and specificity 86.7%, in characterization of different suspicious breast lesions, that minimally inferior to DCE-MRI Sensitivity 93.3% and Specificity 93.3%.
We agree with study published in 2021 by Nabil et al., [11] included 45 female with suspicious breast lesions (BIRADS IV&V), regarding high DWIBS sensitivity (97.47%) and NPV (95.24%), and DCE-MRI showed specificity 95.7% and PPV 97.39% superior to those of DWIBS 87% and 92.5% respectively.
We also agree with Study published in 2017 by Adel et al., [12] as DWIBS showed high acceptable sensitivity of 93% with good over-all efficacy 90% and did not have a superior result to DCE-MRI regarding the specificity and PPV measuring 83.3% and 100% for DCE-MRI compared to 83.3% and 92.9% for DWIBS, respectively.
The estimated cut-off ADC value in our study was comparable to cut-off values presented in literature, that similar to Sebastian Bickelhaupt et al. 2016 [8], who reported a cut-off value of 1.24 × 10−3 and Adel M. et al. [12], who reported a cut-off value of 1.28 × 10−3, but lower than Moschetta et al. 2014 [5], who reported a cut-off value of 1.44 × 10−3 and Stadlbauer et al. 2009 [9], who reported a cut-off value of 1.44 × 10−3, and higher than Nabil et al. 2021 [11], who reported a cut-off value of 1.1 × 10−3.
Breast DWIBs may result in false positives due to hematomas, highly-cellulated fibroepithelial lesions, abscesses, cysts with thick content and intra-mammary lymph nodes. On the other hand, mucinous carcinoma and small lesions can result in false negatives [14].
In our study, we obtained false-positive results for only seven lesions that showed restricted diffusion on DWIBS, six of them were subsequently diagnosed pathologically as fibroadenomas with high fibrous content which had ADC values: (two lesions of 1 × 10−3 mm2/s, one lesion of 1.03 × 10−3 mm2/s, one lesion of 1.1 × 10−3 mm2/s and two lesions of 1.2 × 10−3 mm2/s).One of them was diagnosed pathologically as benign lymph node, with ADC value (1.2 × 10−3 mm2/s). The ADC cut-off value settled in our study was (1.2 × 10−3 mm2/s). On DCE-MRI, there were six false positive lesions diagnosed pathologically as fibroadenomas.
Fibroadenomas remain one of the most common lesions displaying as a false-positive finding on DCE-MRI. Although certain imaging characteristics, like strong homogeneous signal on T2-weighted sequences and non-enhancing dark septations, are reported as characteristic of fibroadenomas, these findings are not found in many fibroadenomas and are not sufficiently specific to exclude malignancy as insulated features.Fibroadenomas commonly present high ADC values in the non-malignant range due to low stromal cellularity with higher water mobility. However, for unclear reasons, numerous fibroadenomas display low ADC within the malignant range [13].
DWIBS in many cellular or fibrotic lesions, water diffusion is allowed to be more restricted. Breast cancers generally have higher cellularity, restricted water diffusion and lower ADC values than reference normal breast parenchyma and benign breast lesions [14]. Fibroadenomas with epithelial hyperplasia and high cellularity displayed significantly lower ADC values. Presence of immune cell infiltration in cases of mastitis, abscess or inflammatory carcinoma of the breast were reportedly associated with low ADC values [13].
On the other side, no false negative on DWIBS was recorded in our study, probably due to the absence of low cellularity breast tumors, such as mucinous carcinoma.
Although presence of one malignant lesion showed type 1 kinetic curve, denoting false negative result of kinetic curves only, but was not denoting a false negative of overall result of DCE-MRI, as characterization of malignant lesion by DCE-MRI depended on overall criteria included morphology, pattern of enhancement and kinetic curves, so we went with more suspicious findings. Overall on DCE-MRI, no false negative results were recorded in the current study.
Limitations of the study
Small sample size of the patients, so our results need to be further assessed on a larger sample. Most of the histopathologies encountered in our study were infiltrative ductal carcinoma, infiltrative lobular carcinoma or fibroadenoma and hence the results cannot be generalized for other malignant or benign pathologies.
Conclusions
DWIBS can be added to DCE breast MRI as complementary tool to make radiologist more confident about the diagnosis. It can as well be used instead of DCE-MRI sequences in certain circumstances as in cases of renal impairment.
Availability of data and materials
Available on request with the corresponding author.
Abbreviations
- DWIBS:
-
Diffusion weighted imaging with background signal suppression
- DCE:
-
Dynamic contrast enhanced
- CE-MRI:
-
Contrast enhanced magnetic resonance imaging
- ADC:
-
Apparent diffusion co-efficient
- ROC:
-
Receiver operating characteristic curve
- PPV:
-
Positive predictive value
- NPV:
-
Negative predictive value
- AUC:
-
Area under curve
- BIRADs:
-
Breast imaging reporting and data system
References
Bray F, Ferlay J, Soerjomataram I, Rebecca L, Lindsey A, Jemal A (2018) Global cancer statistics, GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Cancer J Clin 68(6):394–424. https://doi.org/10.3322/caac.21492
Jafari SH, Saadatpour Z, Salmaninejad A, Momeni F, Mokhtari M, Nahand JS, Rahmati M, Mirzaei H, Kianmehr M (2018) Breast cancer diagnosis: imaging techniques and biochemical markers. J Cell Physiol 233(7):5079–5489. https://doi.org/10.1002/jcp.26379
Belli P, Bufi E, Bonatesta A, Patrolecco F, Padovano F, Giuliani M, Rinaldi P, Bonomo L (2016) Unenhanced breast magnetic resonance imaging: detection of breast cancer. Eur Rev Med Pharmacol Sci 20:4220–4229
Telegrafo M, Rella L, Ianora AS, Angelelli G, Moschetta M (2015) Unenhanced breast MRI (STIR, T2-weighted TSE, DWIBS): an accurate and alternative strategy for detecting and differentiating breast lesions. Magn Reson Imaging 33:951–955. https://doi.org/10.1016/j.mri.2015.06.002
Moschetta M, Telegrafo M, Rella L, Ianora AS, Angelelli G (2014) MR evaluation of breast lesions obtained by diffusion-weighted imaging with background body signal suppression (DWIBS) and correlations with histological findings. Magn Reson Imaging 32:605–609. https://doi.org/10.1016/j.mri.2014.03.009
Kwee TC, Takahara T, Ochiai R et al (2009) Wholebody diffusion-weighted magnetic resonance imaging. Eur J Radiol 70(3):409–417. https://doi.org/10.1007/s00330-008-0968-z
Nechifor-Boilă IA, Bancu S, Buruian M, Charlot M, Decaussin-Petrucci M, Krauth JS, Nechifor-Boilă AC, Borda A (2013) Diffusion weighted imaging with background body signal suppression/T2 image fusion in magnetic resonance mammography for breast cancer diagnosis. Chirurgia (Bucur) 108(2):199–205
Bickelhaupt S, Laun FB, Tesdorff J, Lederer W, Daniel H, Stieber A, Delorme S, Schlemmer H (2016) Fast and noninvasive characterization of suspicious lesions detected at breast cancer X-ray screening: capability of diffusion-weighted MR imaging with MIPs. RSNA Radiol 278(3):634–689. https://doi.org/10.1148/radiol.2015150425
Stadlbauer A, Bernt R, Gruber S et al (2009) Diffusion-weighted MR imaging with background body signal suppression (DWIBS) for the diagnosis of malignant and benign breast lesions. Eur Radiol 19:2349–2356. https://doi.org/10.1007/s00330-009-1426-2
Keriakos N, Mary YT (2017) DWIBS: can it replace DCE-MRI in detection and characterization of suspicious breast lesions? Egypt J Radiol Nuclear Med 48:1171–1177. https://doi.org/10.1016/j.ejrnm.2017.05.002
Nabil YA, Aida ME, Noha MO, Essam MA (2021) Latest updates in the efficiency of the novel MRI technique diffusion weighted imaging with background signal suppression (DWIBS) in comparison to dynamic contrast enhancing MRI technique in clarifying suspicious breast lesions. Ann RSCB 25(4):7379–7393
Adel MA, Haytham MN, Sherine KA (2017) Comparison of sensitivity and specificity of DWIBS and contrast enhanced T1Wi sequences in characterization of suspicious mammography lesions. Egypt J Hosp Med 68(2):1279–1283. https://doi.org/10.12816/0039061
Parsian S, Rahbar H, Chai X et al (2016) Diffusion weighted imaging reflects variable cellularity and stromal density present in breast fibroadenomas. Clin Imaging 40(5):1047–1054. https://doi.org/10.1016/j.clinimag.2016.06.002
Messina C, Bignone R, Bruno A et al (2020) Diffusion-weighted imaging in oncology. Cancers 12(6):1493. https://doi.org/10.3390/cancers12061493
Acknowledgements
Not applicable.
Funding
All authors declare that no funding or any source of financial interest.
Author information
Authors and Affiliations
Contributions
SF: The idea, organization, data collection, and writing. AMO: The idea, writing, and corresponding author. SMA: Help in data collection and writing. ASA: Statistical analysis, help in writing, and revision. All authors declare that: they all read and approved the final version of the submitted manuscript. The authors declare that this is an original work, hasn't received prior publication, and isn't under consideration for publication elsewhere. The authors confirm sole submission to Egyptian Journal of Radiology and Nuclear Medicine. They all confirm that the article is not under consideration for publication elsewhere. All authors declare no subject overlap with previously published work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Were taken from our institute ethical committee (Faculty of Medicine-Ain shams university), the informed written consents were waived.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
El-Sawy Deif Allah, N.S., Abdallah, R.H., Hassan, M.S. et al. Role of diffusion weighted imaging with background body signal suppression (DWIBS) in diagnosis of breast masses and correlation with histopathological findings. Egypt J Radiol Nucl Med 55, 95 (2024). https://doi.org/10.1186/s43055-024-01260-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-024-01260-9