Abstract
Background
Chemotherapy-associated cardiomyopathy is a well-known cardiotoxicity of contemporary cancer treatment. As cancer outcomes improve, cardiovascular disease has become a leading cause of morbidity and mortality among cancer survivors. The objective of this study was to evaluate the role of CMR in the detection of early cardiotoxic changes and in the identification of patients at risk of developing CTRCD.
Patients and methods
Fifty patients diagnosed breast cancer examined by echocardiography and cardiac MRI before the start of chemotherapeutic regimen followed by 2 and 4 months post-chemotherapy.
Results
By echocardiography, all measures were within normal range at the start and at the first follow-up. Twenty (40%) patients show decreased LVEF at second follow-up reaching up to 50% with milder affection of the other parameters. CMR examination shows decreased LVF at second and third follow-up (p = 0.005). There was significant elevation of T2 value for 10 patients at first follow-up (p value 0.04) and for 22 patients at second follow-up (p value 0.01) in correlation with baseline. The T1 mapping and ECV showed elevation at first and second follow-up as compared to baseline (p = < 0.05).
Conclusion
T1 and T2 mapping is superior to echocardiography in early detection of the cardiotoxic effects of chemotherapy applied for breast cancer patients and can guide the management and patient lifestyle.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Several years ago, cancer therapy-induced cardiotoxic reactions were first recognized with the use of anthracyclines, but after that it was identified that such cancer therapy-related cardiac dysfunction (CTRCD) can be induced by other cancer therapies as well including Herceptin (trastuzumab) and immunotherapeutic agents [1,2,3].
Cardiotoxicity is a general term which refers to cardiac injury due to myocyte damage, which may or may not be accompanied by physiologic changes. Cardiac dysfunction is a more specific term which means the presence of a measurable systolic function decline [4].
Chemotherapeutic agents are classified into two types: Type I and Type Il [4,5,6,7]:
Type I: All types of anthracyclines (doxorubicin, epirubicin and idarubicin) are classified in this type [8, 9]. However, the characteristic agent is doxorubicin. This group of agents leads to permanent, irreversible damage which is also cumulative dose related.
Type II: The characteristic agent of this type is trastuzumab which is intended in our study. The damage caused by this group of agents is usually reversible and is unrelated to dose.
The risk of developing CTRCD is defined based on the cardiac review and evaluation committee criteria as a ≥ 10% reduction in left ventricular ejection fraction from baseline to < 55% in the absence of heart failure symptoms, or a reduction of ≥ 5 to < 55% with symptoms by CMR and 2DE separately [10].
Multiple factors are known to increase the risk of developing CTRCD including: patient-related factors (age and pre-existing CV disease), CV risk factors (obesity, diabetes, tobacco use and sedentary lifestyle), CV risk factors metabolic abnormalities and hypersensitivity to the drugs as well as prior chemotherapy and/or radiotherapy [11].
The most commonly discussed form of CTRCD is HF. However, cancer therapy-related cardiac complications may present in different ways, including myocardial ischemia, changes in blood pressure, arrhythmias (including bradycardia, tachyarrhythmias and atrio-ventricular (AV) blocks), pericarditis, pericardial effusion, or pericardial thickening [11, 12].
Trastuzumab is one of the monoclonal antibody-based tyrosine kinase inhibitors or what is called targeted cancer therapy. Their function is to bind a specific target and block its action. One of these targets is the human epidermal growth factor II (HER-2), which is a member of the epidermal growth factor receptor family. Trastuzumab (trade name of Herceptin) is the most commonly used tyrosine kinase inhibitor in the clinical practice especially in breast cancer and results in type II CTRCD [5, 13].
Chemotherapeutic regimens which include only trastuzumab lead to lower rates of CTRCD than combine trips to trastuzumab and anthracyclines. At the ultrastructure level, trastuzumab-related cardiotoxicity is characterized by monocyte dysfunction rather than necrosis [14].
Imaging modalities
Echocardiography is the most popular imaging technique for assessing patients before, during and then after potentially cardiotoxic medication. Its widespread accessibility, repeatability, adaptability, absence of radiation exposure and safety for individuals with concurrent renal illness all contribute to this [15].
The introduction of additive echocardiographic markers for the identification of subclinical myocardial dysfunction has thus received substantial scientific attention. The usefulness of echocardiographic measurements of diastolic function has been investigated following chemotherapy, but the findings are conflicting; thus, diastolic tests really are not usually advised for this indication. Diastolic dysfunction frequently occurs before systolic failure [16, 17].
Myocardial strain imaging can identify early myocardial injury [18]. Cardiac stress imaging can accurately measures the cardiac systolic function not only EF due to the ability of estimation of the myocardial displacement or strain in all three dimensions (longitudinal, radial and circumferential) [19,20,21].
Cardiovascular magnetic resonance (CMR) imaging
T1-weighted and T2-weighted CMR techniques have been successful in identifying myocardial infarction and provide valuable information for the early detection of cardiotoxicity. For example, T1-weighted and T2-weighted images have shown vascular dysfunction and edema in addition to changes in quantitative measures of tissue dysfunction in patients with myocardial infarction [22]. Delayed enhancement CMR imaging is rapid and standard in clinical practice but may yield variable results due to T2 effects [23].
Recent advances in CMR techniques have enabled quantitative mapping of magnetic relaxation values (T1 and T2), which overcome many of the disadvantages of qualitative techniques. Although there is an increased scan time associated with quantitative mapping of tissue, T1/T2 readings may be immediately examined on several scanners and on various pictures without the need to provide a contrast agent [24].
CMR plays an important role in the diagnosis of myocardial fibrosis. LGE can accurately recognize myocardial scars, while T1 mapping is another novel technique applied for the assessment of chronic diffuse myocardial fibrosis [25]. A recent CMR technique developed from a pre- and a post-contrast T1 measurement allows quantification of the ECV which is a marker of myocardial interstitial fibrosis [26, 27].
Patients and methods
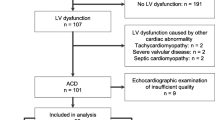
This prospective study was carried out in the period from November 2019 until June 2022 on 50 patients receiving cardiotoxic chemotherapy (trastuzumab) that were referred to the Department of Radiology, Faculty of Medicine, Minia University, for treatment of breast cancer patients scheduled to undergo treatment with trastuzumab "Herceptin." All patients had written the informed consent. The study was approved by the Ethics Committee of the Faculty of Medicine, Minia University.
Inclusion criteria: adult female patient (> 18 years) prepared for trastuzumab regimen and able to tolerate three CMR examinations, each one last about 45 min.
Exclusion criteria: patient’s age (< 18 years), previous start of chemotherapy which was intended to be studied, pre-existing symptomatic HF, recent acute coronary syndrome, persistent atrial fibrillation, patients with cardiac pacemakers, implantable hearing aids, intracranial metal clips, metallic bodies in the eye, insulin pumps, extreme claustrophobia, renal insufficiency (GFR < 30 ml/min/1.73 m2), inability to sustain a breath-hold, morbid obesity and clinically unstable patients.
Methods
All patients were subjected to full history taking, clinical cardiac examination and ECG examination. A written consent was taken from all patients.
A. Echocardiography
2D Echocardiography for assessment of LVEF, EDV, ESV, LVEDV and LVESV before the start of the chemotherapy (baseline), after 2 (early follow-up) and 4 months (late follow-up).
B. CMR
Imaging schedule
Serial CMR was performed at three time points:
-
Baseline: Before the start of chemotherapy.
-
Early follow-up: 2 months after the start of chemotherapy.
-
Late follow-up: 4 months after the start of chemotherapy.
CMR protocol and standard parameters
All CMR examinations were performed in Radiology Department, Faculty of Medicine, Minia University Hospital, using clinical MRI system (Ingenia 1.5 T Philips) equipped with a body phased-array 18-channel receiver coil and ECG gating.
All patients were scanned using an identical imaging protocol as follows:
(1) Scout images (axial, coronal and sagittal) using real-time interactive planning: imaging parameters were: FOV 450 × 450 mm2, TR/TE 2.1/0.82 ms, slice thickness 10 mm, acquisition matrix 192 × 96, voxel size = 2.38 × 4.69 × 10 mm3 and flip angle 50°. (2) Cine images using a breath-hold bSSFP with a retrospective ECG gating in LV LAx planes (2 Ch, 3 Ch and 4 Ch) as well as in contiguous SAx slices. (3) Native myocardial Tl mapping before IV contrast agent administration using a breath-hold MOLL1 sequence in three SAx planes at different LV levels. (4) Myocardial T2 mapping in three SAx plane using a breath-hold turbo SE (TSE) sequence. IV contrast agent administration (injection of 0.2–03 mmol/kg body weight gadolinium-based contrast agent)
NB: A breath-hold look-locker T1-scout sequence was acquired in one mid-ventricular SAx plane before LGE acquisition to determine the accurate T1 for nulling normal myocardial signal intensity.
(5) LGE After about 6–10 min of IV contrast agent administration using breath-hold TI-weighted inversion recovery PSIR sequences along the same planes of the cine bSSFP images. (6) Myocardial post-contrast T1 mapping after 10 min of IV contrast agent injection using a breath-hold MOLLI sequence with the same planning and CMR parameters as the native map in order to acquire the myocardial ECV maps.
CMR analysis
All the MRI images were transferred to a commercial off-line workstation for further analysis. The software we used for post-processing was IntelliSpace Portal (ISP) workstation (Version 9.1, Philips Healthcare, Best, The Netherlands).
The collected CMR parameters included standard morphological and functional parameters for LV as well as tissue characterization parameters (LV global TI and T2 Mapping) as well as the number of abnormal LV segments and percentage of healthy myocardium.
Ventricular volumes and function: Results for ventricular EDV index (EDVi), ESV index (ESVi), EF, SV and LV mass index (LVi) were quantitatively, evaluated in SAx-cine images through manually tracing the epi- and endocardial borders on successive images at end-diastole and mid-systole.
Myocardial TI, T2 mapping and ECV fraction: Epicardial and endocardial contours were manually traced in three SAx slices (basal, mid-ventricular and apical). ECV fraction was reported in percentage and measured using the native and post-contrast Tl values as well as patient's hematocrit value. Checking the presence of enhancement: LGE images were checked at the different planes for the presence or absence of enhancement in each segment.
Statistical analysis
The analysis of the data was carried out using the IBM SPSS 26.0 statistical package software (IBM; Armonk, New York, USA). Normality of the data was tested using the Shapiro–Wilk tests. Data were expressed as mean and standard deviation for quantitative measures, in addition to both number and percentage for categorized data McNemar test used to compare frequencies on multiple measures. A p-value less than 0.05 was considered significant.
Results
Regarding the demographic data, the mean age of study population was 44.8 years, 35 patients were female, and 15 patients were male. The mean body mass index (BMI) of the cohort study was 25.3 kg/m2.
Echocardiography findings
All patients underwent echocardiography examination before the start of chemotherapy, two- and four-month follow-up. All measures were within normal range including LVEF, EDV, ESV, LVEDV and LVESV at the start and at the first follow-up. Twenty (40%) patients show decreased LVEF at second follow-up reaching up to 45% with milder affection of the other parameters (Fig. 1).
CMR findings
-
Fifty patients prepared for cardiotoxic chemotherapy regimen were enrolled in our study with mean age 44.8 years, 60% being female and 40% being male.
-
They underwent prospective CMR at baseline of start of the chemotherapy, 2 months and 4 months thereafter as follow-up.
-
All patients showed normal CMR volumetric, functional and tissue characterization parameters at the baseline study.
-
LVEF was within normal range at baseline. However, it tended to decrease at first follow-up which was followed by a significant reduction at the second follow-up in comparison with the baseline with p = 0.005
-
Compared to the baseline, there was a significant increase of LVESV at the first and second follow-up with p = < 0.0001 for both (Table 1).
-
The LVMi was also decreased significantly at the first follow-up (p = 0.016) but no significant interval changes at the second follow-up (60%)
-
There was no significant correlation between changes at first follow-up in LVEF and LVMi (Pearson's correlation coefficient = −0.048, p = 0.740).
-
LVEDV shows mild increase at the first follow-up with no significant interval changes at the second follow-up (p = < 0.99)
-
LVESV shows mild increase at the first follow-up more appreciated at the second follow-up (p = < 0.001)
-
Only two patients (4%) showed at second follow-up; anterior, anteroseptal and anterolateral mid-segmental, subpericardial LGE (Fig. 2).
-
The T1 mapping and ECV showed mild elevation at first follow-up, which was followed by significant elevation at second follow-up as compared to baseline. Values are expressed as p, probability [significance < 0.05] (Fig. 3).
-
There was significant elevation of T2 value for 10 patients (20%) at first follow-up (p value 0.04) and for 22 patients (44%) at second follow-up (p value 0.01) in correlation with baseline (Figs. 1, 4, 5 and Tables 2, 3).
Discussion
Cancer survivors are increasing nowadays however with increased incidence of cardiovascular complications mainly due to the cardiotoxic effect of chemotherapy. Such cardiotoxic changes may adversely affect the clinical condition of cancer survivors. Therefore, monitoring cancer patients using cardiac imaging has been increasingly implemented in the cardio-oncology field, which may provide early diagnosis and prevention of chemotherapy-related cardiovascular complications through allowing early use of different cardioprotective measures [28, 29].
Recently, a significant increase in cancer survivors has been observed but with an increased risk of premature cardiac disease. The cardiotoxic effect of cancer chemotherapy is not the only reason for this observation but also the overlap in risk factors for cancer and CV disease [27, 30]. Therefore, the use of cardiac imaging with this group of patients is increasingly important for early recognizing and preventing complications that occur after treatment with cancer chemotherapy [31]. However, the detection of chemotherapy-related cardiotoxicity is still challenging, mainly because of the length of the period, during which cardiac dysfunction may occur as well as the frequent absence of clinical symptoms. Moreover, the currently used definition of CTRCD depends mainly on the changes of LVEF, which on the one hand does not demonstrate the early cardiotoxic changes and on the other hand is mainly measured by echocardiography, which has several limitations [32].
Although 2D TTE is still considered the standard cardiac imaging modality, because of its availability, low cost and absence of ionizing radiation, it does not achieve the accuracy of CMR in the measurement of cardiac function due to the underestimation of LV volumes together with its lower spatial resolution and hence its lower reproducibility [33].
Our study shows normal ranges at baseline examination but reduced parameters at the follow-up mainly the second one in comparison with early detection of reduced LV parameters by CMR.
Cardiac magnetic resonance imaging (CMR) is the gold standard for the noninvasive assessment of LV volumes and LVEF and playing an important role as a part of the multimodality imaging for better diagnosis of cardiotoxicity and understanding the mechanism of CRCD. Thus, CMR can evaluate changes over time in morphological, functional and tissue characterization parameters so detect early myocardial affection [30, 34].
During follow-up of the chemotherapy included in this study, the LVEF tended to decrease at 2 months, followed by a significant reduction at 4 months after initiation of chemotherapy. This finding is consistent with another study conducted on breast cancer patients treated with trastuzumab and also found that the LVEF started to decrease at 3 months, followed by a significant reduction at 6 months after initiation of therapy [35].
CMR allows myocardial tissue characterization through the use of recent myocardial T1 and T2 mapping techniques. They allow quantitative assessment of diffuse myocardial tissue alteration [36].
An increased native T1 indicates the presence of diffuse myocardial fibrosis and edema. An increased T2 is useful for the diagnosis of acute inflammatory processes such as myocarditis [37].
Our study analyzed T1 and T2 mapping CMR in breast cancer patients treated by chemotherapy (Herceptin) trastuzumab. Furthermore, the predictive value of CMR for early identification of CTRCD was analyzed.
The tissue characterization parameters (native T1 and T2 maps) showed significant elevation among our cohort of patients during second follow-up after initiation of chemotherapy. The elevation in native T1 map at 4 months was also reported by Haslbauer et al., who reported a significant elevation in native T1 map within 4 months after initiation of chemotherapy and remained elevated until > 12 months. The same group found also a significant elevation in T2 map within 4 months after initiation of chemotherapy which was followed by later recovery. They assumed that native T1 map is the most effective predictor of chemotherapy-induced cardiotoxicity, while T2 map is considered the second valid predictor of early cardiotoxicity [38]. This observation is similar to our findings, as we found significant elevation in T2 map after 4 months among breast cancer patients.
Our study confirms and extends the knowledge about the value of T2 and T1 to detect chemotherapy-related myocardial injury. Interestingly, we found a more pronounced increase in T1 compared to T2 in our patients with chemotherapy. This finding is most likely related to the fact that we performed the first follow-up CMR 2 months after chemotherapy initiation, which was followed by 4-month follow-up, whereas Galán-Arriola et al. performed weekly CMR [39]. We presume that we imaged the patients at a later time point of myocardial injury when T2 had already normalized, but T1 was still elevated. Similar to Galán-Arriola et al., we observed that the T1 increase was paralleled by a LV dysfunction quantified by reduction of LVEF.
Myocardial fibrosis due to collagen deposition from acute or chronic disease is associated with several forms of cancer treatment, including the administration of anthracycline chemotherapy and trastuzumab. Increases in interstitial fibrosis can impair both LV diastolic and systolic function. Pathological myocardial fibrosis due to cancer therapy tends to be diffuse [40], while LGE may detect focal areas of myocardial fibrosis. Quantitative assessment of interstitial myocardial fibrosis using mapping techniques shows increased native T1 and extracellular volume (ECV) fraction measures. ECV fraction measures are obtained by acquiring T1 assessments before and after GBCA administration and accounting for heart rate and serum hemoglobin [41].
In our study, diffuse myocardial fibrosis could be detected at each follow-up by calculating ECV fraction at basal, mid-ventricular and apical segments. We found significant ECV fraction elevation at the apical segments at first follow-up, but significant elevation at more and variable LV segments at second follow-up 4 months post-chemotherapy initiation compared to the baseline study. This is matched with Muehlberg et al. found; ECV was higher at the end of chemotherapy than at baseline and 48 h after the first dose of anthracyclines, because of the loss in LV mass [42]. In the animal model proposed by Hong et al., no detectable changes in LVEF and native T1 were observed after 6 weeks, while ECV changed significantly within the first three weeks. Therefore, ECV could serve as an early marker of myocardial damage [43].
In a study of women with breast cancer treated with anthracyclines ± trastuzumab, the presence of myocardial edema was demonstrated through T2 mapping in 49% of the sample from 1 to 4 months after the start of therapy [44]. Our study shows similar results with elevated T2 values gradually from first to second follow-up. The values of T2 mapping are sensitive to myocardial edema which may be represented early before elevation of T1 mapping and ECV values.
The pattern, incidence and prognostic significance of LGE in patients receiving chemotherapeutic agents are not matching between the degree of cardiac toxicity and dose of therapeutic regimen. One group was studied by retrospective and prospective methods shows that the presence of LGE in the context of established cardiomyopathy in patients during and at end of therapy with anthracyclines and trastuzumab with no significant interval changes among follow-ups [45, 46].
The pattern of LGE shows different non-specific patterns include subepicardial or myocarditis-like, and the incidence ranged between 94 and 100%. A study included 10 patients with non-Hodgkin lymphoma, showed new or progressive midmyocardial LGE in 30% of patients 3 months after fulfillment of therapy which represent early myocardial damage, while preserved LVEF [47].
Limitations of study
Limitations of the study include the small sample size and short follow-up duration. Therefore, studies with larger cohorts and longer follow-up are recommended for the validation of our findings.
Conclusion
Echocardiography is mandatory as a guideline in evaluation of the cardiac function before the initiation of the chemotherapeutic regimen of breast cancer patients and follow-up as an available widespread non-cost diagnostic tool. But the early prediction of the cardiotoxic effects of the chemotherapy by T1 and T2 mapping will guide the management, planning and the outcome of the patient life.
Availability of data and materials
The data are available on a reasonable request.
Abbreviations
- ACE:
-
Angiotensin-converting enzyme
- CMR:
-
Cardiac magnetic resonance
- CTRCD:
-
Cancer therapy-related cardiac dysfunction
- ECV:
-
Extracellular volume
- EF:
-
Ejection fraction
- GBCA:
-
Gadolinium-based contrast agent
- HER-2:
-
Human epidermal growth factor II
- LGE:
-
Late gadolinium enhancement
- MRI:
-
Magnetic resonance imaging
- TTE:
-
Trans-esophageal echocardiography
- 3D:
-
Three dimensional
References
Liu J et al (2022) Understanding myocardial metabolism in the context of cardio-oncology. Heart Fail Clin 18(3):415–424
Montera MW et al (2022) Brazilian Society of Cardiology Guideline on Myocarditis–2022. Arquivos Brasil Cardiol 119:143–211
Celeste LEN, Maia MR (2021) Cuidados de enfermagem relacionados à cardiotoxicidade envolvendo drogas como a antraciclinas e anticorpo monoclonais no tratamento oncológico. Rev PubSaúde 5:905
Nishino M, Hatabu H, Stephen Hodi F (2019) Imaging of cancer immunotherapy: current approaches and future. Radiology 290:9–22
Jeong D et al (2019) MRI in cardio-oncology: a review of cardiac complications in oncologic care. J Magn Resonance Imaging 50(5):1349–1366
Jacobs JEJ et al (2022) Predictability of cardiotoxicity: experience of a Belgian cardio-oncology clinic. Int J Cardiol 363:119–122
Zamorano JL et al (2016) ESC Position Paper on cancer treatments and cardiovascular toxicity developed under the auspices of the ESC Committee for Practice Guidelines: The Task Force for cancer treatments and cardiovascular toxicity of the European Society of Cardiology(ESC). Eur Heart J 37(36):2768–2801
Caron J, Nohria A (2018) Cardiac toxicity from breast cancer treatment: can we avoid this? Curr Oncol Rep 20(8):1–8
Ferreira de Souza T et al (2018) Anthracycline therapy is associated with cardiomyocyte atrophy and preclinical manifestations of heart disease. JACC Cardiovasc Imaging 11(8):1045–1055
Seidman A, Hudis C, Pierri MK et al (2002) Cardiac dysfunction in the trastuzumab clinical trials experience. J Clin Oncol 20:1215–1221
Pedersen S et al (2022) Cardiotoxicity in metastatic melanoma patients treated with BRAF and MEK inhibitors in a real-world setting. Acta Oncol 61(1):45–51
Dong J, Chen H (2018) Cardiotoxicity of anticancer therapeutics. Front Cardiovasc Med 5:9
Fallah-Rad N et al (2011) The utility of cardiac biomarkers, tissue velocity and strain imaging, and cardiac magnetic resonance imaging in predicting early left ventricular dysfunction in patients with human epidermal growth factor receptor II–positive breast cancer treated with adjuvant trastuzumab therapy. JACC 57:2263–2270
Onitilo AA, Engel JM, Stankowski RV (2014) Cardiovascular toxicity associated with adjuvant trastuzumab therapy: prevalence, patient characteristics, and risk factors. Ther Adv Drug Saf 5(4):154–166
Nolan MT, Thavendiranathan P (2019) Automated quantification in echocardiography. Cardiovasc Imaging 12(6):1073–1092
Halliday BP, Senior R, Pennell DJ (2021) Assessing left ventricular systolic function: from ejection fraction to strain analysis. Eur Heart J 42(7):789–797
Tsai T-H et al (2019) Calcitriol attenuates doxorubicin-induced cardiac dysfunction and inhibits endothelial-to-mesenchymal transition in mice. Cells 8(8):865
Pedrizzetti G et al (2016) Principles of cardiovascular magnetic resonance feature tracking and echocardiographic speckle tracking for informed clinical use. J Cardiovasc Magn Resonance 18(1):1–12
Kanngiesser LM et al (2022) Serial assessment of right ventricular deformation in patients with hypoplastic left heart syndrome: a cardiovascular magnetic resonance feature tracking study. J Am Heart Assoc 11(9):e025332
Alam S et al (2019) To study the usefulness and comparison of myocardial strain imaging by 2D and 3D echocardiography for early detection of cardiotoxicity in patients undergoing cardiotoxic chemotherapy. Indian Heart J 71(6):468–475
Oikonomou EK et al (2019) Assessment of prognostic value of left ventricular global longitudinal strain for early prediction of chemotherapy-induced cardiotoxicity: a systematic review and meta-analysis. JAMA Cardiol 4(10):1007–1018
Writing Committee Members et al (2010) ACCF/ACR/AHA/NASCI/SCMR 2010 expert consensus document on cardiovascular magnetic resonance: a report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents. Circulation 121(22):2462–2508
Klug G, Metzler B (2013) Assessing myocardial recovery following ST-segment elevation myocardial infarction: short-and long-term perspectives using cardiovascular magnetic resonance. Expert Rev Cardiovasc Ther 11(2):203–219
Ferreira VM et al (2012) Non-contrast T1-mapping detects acute myocardial edema with high diagnostic accuracy: a comparison to T2-weighted cardiovascular magnetic resonance. J Cardiovasc Magn Resonance 14(1):1–12
Messroghli DR et al (2017) Clinical recommendations for cardiovascular magnetic resonance mapping of T1, T2, T2* and extracellular volume: a consensus statement by the Society for Cardiovascular Magnetic Resonance (SCMR) endorsed by the European Association for Cardiovascular Imaging (EACVI). J Cardiovasc Magn Resonance 19(1):1–24
Löffler AI, Salerno M (2018) Cardiac MRI for the evaluation of oncologic cardiotoxicity. J Nucl Cardiol 25(6):2148–2158
Jordan JH et al (2016) Anthracycline-associated “T1 mapping characteristics are elevated independent of the presence of cardiovascular comorbidities in cancer survivors.” Circul Cardiovasc Imaging 9(8):e004325
Zhuang B et al (2018) Prognostic value of T1 mapping and extracellular volume fraction in cardiovascular disease: a systematic review and meta- analysis. Heart Fail Rev 23(5):723–731
Houbois CP, Thavendiranathan P, Wintersperger BJ (2020) Cardiovascular magnetic resonance imaging: identifying the effects of cancer therapy. J Thorac Imaging 35(1):12–25
Yu AF, Chan AT, Steingart RM (2019) Cardiac magnetic resonance and cardio-oncology. J Am Coll Cardiol 73(7):792–794
Maraldo MV et al (2022) An integrated approach to cardioprotection in lymphomas. Lancet Haematol 9:445–454
De Baat EC et al (2021) Update in imaging of cancer therapy-related cardiac toxicity in adults. Open Heart 8(1):e001506
Mavrogeni SI et al (2019) Cardio-oncology, the myth of Sisyphus, and cardiovascular disease in breast cancer survivors. Heart Fail Rev 24(6):977–987
Hundley WG, Jordan JH (2018) When left ventricular extracellular volume fraction changes after anthracyclines: is it due to a change in the numerator, denominator, or both? American College of Cardiology Foundation Washington, DC, pp 1056–1058
Jafari F et al (2021) The role of cardiac magnetic resonance imaging in the detection and monitoring of cardiotoxicity in patients with breast cancer after treatment: a comprehensive review. Heart Fail Rev 26(3):679–697
Upshaw Jenica N et al (2020) Comprehensive assessment of changes in left ventricular diastolic function with contemporary breast cancer therapy. JACC Cardiovasc Imaging 13(Part2):198–210
Cau R et al (2020) Early diagnosis of chemotherapy-induced cardiotoxicity by cardiac MRI. Eur J Radiol 130:109158
Haslbauer JD et al (2019) CMR imaging biosignature of cardiac involvement due to cancer-related treatment by T1 and T2 mapping. Int J Cardiol 275:179–186
Galán-Arriola C et al (2019) Serial magnetic resonance imaging to identify early stages of anthracycline-induced cardiotoxicity. J Am Coll Cardiol 73(7):779–791
Iyer NR et al (2022) Markers of focal and diffuse nonischemic myocardial fibrosis are associated with adverse cardiac remodeling and prognosis in patients with hypertension. The REMODEL study. Hypertension 79:1804–1813
Messroghli DR et al (2017) Clinical recommendations for cardiovascular magnetic resonance mapping of T1, T2, T2* and extracellular volume: a consensus statement by the Society for Cardiovascular Magnetic Resonance (SCMR) endorsed by the European Association for Cardiovascular Imaging (EACVI). J Cardiovasc Magn Reson 19(1):75
Muehlberg F, Funk S, Zange L et al (2018) Native myocardial T1 time can predict development of subsequent anthracycline-induced cardiomyopathy. ESC Heart Fail 5:620–629
Hong J et al (2017) Early detection and serial monitoring of anthracycline-induced cardiotoxicity using T1-mapping cardiac magnetic resonance imaging: an animal study. Sci Rep 7:2663
Thavendiranathan P, Walls M, Giri S et al (2012) Improved detection of myocardial involvement in acute inflammatory cardiomyopathies using T2 mapping. Circ Cardiovasc Imaging 5:102–110
Wadhwa D et al (2009) Trastuzumab mediated cardiotoxicity in the setting of adjuvant chemo- therapy for breast cancer: a retrospective study. Breast Cancer Res Treat 117:357–364
Fallah-Rad N, Lytwyn M, Fang T, Kirkpatrick I, Jassal DS (2008) Delayed contrast enhancement cardiac magnetic resonance imaging in trastuzumab induced cardiomyopathy. J Cardiovasc Magn Reson 10:5
Lunning MA et al (2013) Cardiac magnetic resonance imaging for the assessment of the myocadium following doxorubicin-based chemotherapy. Am J Clin Oncol. https://doi.org/10.1097/COC.0b013e31829e19be. http://journals.lww.com/amjclini-caloncology. Accessed 1 Nov 2013
Acknowledgements
We would thank our supporting team help us in the study.
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Contributions
MAM was involved in writing, revision and editing. ASE was involved in revision and editing. AFZ was involved in data collection and statistics. TEE was involved in data collection and writing. MFA was involved in writing and editing. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the institutional review board of the Faculty of Medicine, Minia University, Egypt.
Consent for publication
Written informed consent was obtained from all subjects (patients) in this study.
Competing interests
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mourad, M.A., Ebrahim, A.S., Ziady, A.F. et al. Chemotherapy-induced cardiotoxic effect in breast cancer patients treated with trastuzumab (Herceptin) by MRI. Egypt J Radiol Nucl Med 54, 207 (2023). https://doi.org/10.1186/s43055-023-01150-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-023-01150-6