Abstract
Background
Inflammatory bowel disease (IBD) is considered as significant cause of morbidity in children with a global rise in its pediatric onset recently. Our study aimed to assess the facility of magnetic resonance enterography (MRE) and diffusion-weighted imaging (DWI) to identify the activity of pediatric IBD in correlation with clinical and endoscopic activity scores. Twenty-four patients of IBD who underwent clinical examination, ileocolonoscopy and MRE and DWI within less than 14 days were prospectively included. For all Crohn’s cases (9/24), the simplified endoscopic activity score for Crohn’s disease (SES-CD) and magnetic resonance enterography global score (MEGS) were acquired, while for all UC (15/24) cases, MRE score and Mayo endoscopic score were calculated. Sensitivity and specificity of MRE for detection disease activity against clinical and endoscopic scores were compared. Pathological reference for disease activity was based on assessment for mucosal inflammatory changes on endoscopic biopsy in all cases.
Results
There was a perfect inter-observer agreement (kappa 0.81–1) regarding wall thickening and mural edema, with substantial agreement (kappa 0.61–0.8) for MRE severity score, mural diffusion restriction, mesenteric edema and vascular congestion, while mural enhancement and for number of active LNs revealed moderate agreement (kappa 0.41–0.6). There was a significant positive correlation between MEGS and SES-CD in Crohn’s cases as well as between Mayo endoscopic score and MRE severity in UC cases (r = 0.970, p > 0.001 and r = 0.544, p = 0.036, respectively). MRE compared to endoscopic findings and clinical activity scores revealed high accuracy (95.8%) with 87.5%, 80%, 96% and 94.1% for sensitivity, specificity, PPV and NPV, respectively.
Conclusion
MR enterography is a noninvasive reliable imaging modality of high accuracy for the diagnosis of pediatric IBD severity compared to endoscopic activity scores and pathological severity.
Similar content being viewed by others
Background
Inflammatory bowel diseases (IBD) include range of conditions generally grouped into ulcerative colitis (UC), Crohn’s disease (CD) and IBD-unclassified (IBD-U) constructed on clinical, laboratory, radiological, endoscopic and histological standards [1]. CD and UC are immunologically mediated chronic inflammatory diseases and considered as significant cause of morbidity in children with a global rise in their pediatric onset recently [2, 3].
CD is a chronic inflammatory transmural disorder which can affect any region of the gastrointestinal tract in a discontinuous distribution [4]. While UC affects the mucosa and submucosa in continuous manner and limited to the colon, it frequently starts in the rectum [5].
Accurate assessment of the extent of pediatric IBD is crucial to detect the ideal treatment strategies, mostly depending on endoscopy which is an invasive procedure with poor patient compliance [2]. MR enterography (MRE) is extensively used to evaluate disease activity, penetrating complications, surgical planning and follow-up [6].
Pediatric MRE is the imaging gold standard for IBD assessment and preferable over CT enterography owing to its excellent resolution and absence of ionizing radiation exposure [7, 8]. MR enterography-based scores have high accuracy for evaluating CD luminal activity, but till now no available CT enterography-based authorized scores for grading activity [9]. Also MRE can detect transmural disease not amenable to endoscopic assessment [10].
Multiple MRE scores were developed to assess CD activity, but magnetic resonance enterography global score (MEGS) allows better imitate of the disease activity as it includes the extra-enteric manifestations and the longitudinal disease extent [2, 11, 12].
Diffusion-weighted imaging (DWI) is a fast functional MR technique with wide acceptance in imaging of IBD as it depends on molecular motion and can illustrate inflammatory lesions in IBD [13, 14] also, DWI is fit for children, owing to quicker image acquisition [15].
With recent concerns around the accumulation of gadolinium in the brain after MRI scans, few studies have discussed the efficacy of DWI to substitute contrast-enhanced MRE for identifying the activity of IBD [15, 16].
To the best of our knowledge, no studies have precisely compared the diagnostic accuracy and inter-observer agreement of both MRE and DWI in detecting activity of pediatric IBD against endoscopic and clinical activity scores with pathological reference standard.
We aimed to estimate the capability of MRE to categorize the activity of pediatric IBD in correlation with clinical, endoscopic and pathological activity score as reference standard and to assess the utility of DWI for the recognition of inflammation.
Methods
Patients
The institutional review board has approved the study and informed consent was obtained from all patients. We included IBD children aged less than 18 years old with clinically suspected relapse and cases with recently diagnosed IBD. All patients underwent clinical examination, ilio-colonoscopy with biopsies and histopathological results (reference standard), contrast-enhanced MR enterography and diffusion-weighted imaging with an interval of 2 weeks or less. No treatment specific IBD was given between the examinations. We excluded 16 patients from the study, six children were diagnosed as nonspecific colitis, two patients had no available endoscopic data, five patients had > 2 weeks interval between MRE and ileocolonoscopy, and the last three patients were excluded due to image quality degradation (especially in DWI) caused by bowel peristalsis or large amount colonic gas. Lastly, 24 patients [11 boys and 13 girls] with pathologically proved UC (15/24) and CD (9/24) were prospectively included in the study in the period from April 2021 to May 2022.The flowchart of the study is illustrated in (Fig. 1).
Clinical, endoscopic and histological assessment
The clinical severity was evaluated employing Pediatric Ulcerative Colitis Activity Index parameters (PUCAI) as well as Pediatric Crohn’s Disease Activity Index parameters in UC and CD patients, respectively. Ileocolonoscopy was performed to assess disease activity within less than 14 days from MRE and DWI. The endoscopic findings of 24 patients were scored by expert gastroenterologist using Simple Endoscopic Score for Crohn’s disease (SES-CD) and the Mayo endoscopic score of ulcerative colitis to assess the severity [17, 18]. Mayo Endoscopic Score of (0) showed inactive UC, (1) mild UC in the form of mild friability or erythema, (2) moderate UC comprised severe erythema, friability with erosive areas and (3) severe UC involved spontaneous hemorrhage and ulcerations [17]. The SES-CD of (0–2) indicted inactive disease, (3–9) mild activity, (9–12) moderate or (≥ 12) severe activity [18].
Specialist pathologist evaluated the severity of the disease on endoscopic biopsy using Geboes scoring system for assessing UC and Scoring system for histological assessment of CD.
MRE technique
Patient preparation
All children had MRI at 1.5-T [Ingenia®, Philips Healthcare]. Children fasted 4–6 h prior to MRI examination then followed by ingestion of a hyperosmolar oral contrast agent (water mixed with Mannitol 20%) for proper small bowel distension.
MRE
Children were examined in supine position with phased-array body coils. Pre-contrast MRI sequences included T1-weighted imaging (T1-WI) and FSE (fast spin echo) T2-WI with fat suppression. Also, half-Fourier single-shot turbo spin-echo (HASTE) and TRUFI (true free-induction steady-state-free precession) sequences were obtained in coronal and axial planes with the following parameters: slice thickness 4 mm; shortest TE/TR; FOV 350–450; matrix 256 × 256; flip angle 50°. Coronal and axial fat saturated 3D VIBE (volumetric interpolated breath-hold examination) T1 gradient-echo sequence were acquired before and after injection of contrast agent, gadolinium diethylene-triamine penta acetic acid (Gd-DTPA) at a dose of 0.5 mmol/kg using an automated MR injector.
DWI
DWI was obtained before contrast injection consuming fat-suppressed single-shot echoplanar sequence with b values (b = 100, 600 and 800 s/mm2). The following acquisition parameters were utilized; slice thickness 5 mm, slice gap 1 mm; TE = 70 ms, number of excitations (NEX) 3 and matrix 124 × 120,
Image analysis
MRE
The MR images were interpreted by two radiologists (with 25- and 8-year experience) who were blinded to patients’ clinical scores and endoscopic data. For easier detection of disease extent, the bowel loops were subdivided into eight regions: the jejunum, ileum, terminal ileum and ileocecal junction, ascending colon, transverse colon, descending colon, sigmoid colon and rectum. Independently, each reviewer analyzed the MRE images and reviewed the MRI findings [19];
-
i-
Bowel wall inflammation; wall thickening, qualitative evaluation of mural edema on T2-weighted fat-suppressed images; grade 1, 2 or 3 if it was similar to muscles, liver, spleen, respectively, qualitative evaluation of the mural enhancement on T1-weighted fat-suppressed images; grade 1, 2 or 3 if enhancement was similar to that of muscles, splenic parenchyma, aorta, respectively, length of the affected segment and stricture.
-
ii-
The penetrating disease features; sinus tracts, abscesses, mesenteric edema, engorged vasa recta (comb sign), perianal fistulas and number of active lymph nodes (LN); active if exceeded 5 mm with contrast enhancement.
-
iii-
The exrta-enteric findings: sacroilitis, cholangitis and GB stone.
Guided by MEGS [2, 12, 20], each reviewer separately categorized CD patients into three subgroups; mild, moderate and severe activity with scores (score 6–7), (score 8–13) and (score 14–18), respectively.
To date, there is no validated MRE scoring system for UC, so guided by the recorded MRE and DWI data [21] and radiologists’ judgment, each radiologist classified 15 UC patients into three subgroups; mild, moderate and severe activity.
DWI
Each reviewer independently assessed DWI and ADC images to exclude T2-shine through and confirm the restricted diffusion. High signal intensity at high b value with corresponding low ADC signal (true diffusion restriction) is considered as an active lesion of IBD.
The MRE and DWI findings were compared with the clinical, endoscopic scores and histopathological activity.
Statistical analysis
The statistical analysis of data was performed by using SPSS program (Statistical package for social science version 20). Qualitative data were illustrated using number and percent. Quantitative data were illustrated using median for nonparametric data and mean, standard deviation for parametric data. Significance of the obtained results was considered at the (0.05) level. In the weighted kappa statistic (K), 95% confidence interval (CI) with percentage agreement was done to assess the proportion of agreement for both reviewers for bowel wall inflammation, penetrating disease and extraintestinal findings as well as the MEGS. Kappa agreement was with kappa (0.01–0.20: Slight agreement, 0.21–0.40: Fair agreement, 0.41–0.60: Moderate agreement, 0.61–0.80: Substantial agreement and 0.81–0.99: Perfect agreement). The accuracy, sensitivity and specificity of the MRE scoring for each reviewer were calculated. The correlation between MRE severity, clinical and endoscopic activity scores was assessed by Spearman’s rank estimation.
Results
Patients’ characteristics and clinical manifestations
Twenty-four patients with pathologically proved UC (15/24) and CD (9/24) were prospectively included with mean age 13.27 ± 3.53 and 13.78 ± 3.67 years, respectively. For Crohn’s, two-thirds (66.7%) were males and one-third (33.3%) were females with reversed relation in UC. There was no statistically significant difference between UC and CD concerning sex, age, period of disease and treatment. Clinico-epidemiologic features and disease presentation are illustrated in (Table 1).
Endoscopic findings
Mayo endoscopic score of ulcerative colitis, SES-CD and simplified score for CD are illustrated in (Tables 2, 3, 4). SES-CD revealed that the allocation of involved segments was mostly ilium (77.7%) and right-sided colon (44.4%). The simplified score for CD per highest segment involved revealed that the median score for size of ulcers, ulcerated surface, and affected surface were 1.1, 1.4 and 1.3, respectively, while the presence of narrowing was 0.89 and total score median was 6. Mild disease was detected in 33.3% of cases, whereas inactive disease, moderate and severe disease each correspond to 22.2% of cases.
Histopathological findings
The overall score of Geboes scoring system for assessing ulcerative colitis histological activity was mainly moderate disease in ten cases (66.7%), mild in four cases (26.7%) and severe disease in one case (6.7%). In CD cases, histopathologic severity was assessed according to pathologist decision as follows; no detected cases in remission (0.0%), whereas mild, moderate and severe disease each correspond to (33.3%) of cases.
MRE findings
There was almost perfect inter-observer agreement (kappa 0.81–1) concerning mural edema and wall thickening, substantial agreement (kappa 0.61–0.8) for MRE severity score, mesenteric edema, mural diffusion restriction, and disease extent and moderate agreement (kappa 0.41–0.6) for mural enhancement (Table 5).
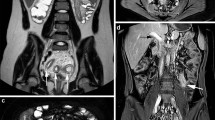
Statistically significant difference was revealed among UC and CD regarding mural edema (higher values were observed in moderate UC). There was also statistically significant difference concerning small bowel affection, it was detected in all CD patients and in six cases (40%) of UC representing backwash ileitis (p = 0.006), and large bowel involvement was detected in all UC patients and in six cases (66.7%) of CD (p = 0.04). Haustral loss was detected in eight cases (53.3%) of UC and not detected in CD patients (p = 0.009). No patient had small bowel obstruction, fistula or abscess formation. Demonstrative CD and UC cases are shown in (Figs. 2 and 3).
Ten-year-old girl with Crohn’s disease (mild activity according to MEGS): Axial T2-weighted image with fat saturation (A) revealed mild wall thickening of the terminal ileum (5mm) and mild hyperintensity (mural edema). Axial T1 post-contrast weighted image with fat saturation (B) revealed mild mural enhancement. Axial DWI (C) and corresponding ADC map (D) revealed mural diffusion restriction. Coronal T2-weighted image with fat saturation (E) revealed mild wall thickening and mural edema of terminal ileum and ileocecal region along length less than 10 cm
Thirteen-year-old girl with ulcerative colitis with moderate activity: Axial T2-weighted image with fat saturation (A) revealed wall thickening (7 mm) and moderate hyperintensity (mural edema) of ascending and descending colon. Axial T1 post-contrast weighted image with fat saturation (B) revealed marked mural enhancement. Axial DWI (C) and corresponding ADC map (D) revealed marked mural diffusion restriction
Our results revealed very good sensitivity, specificity, PPV, NPV and accuracy of mural diffusion restriction on DWI 100%, 80%, 76.2%, 100% and 90.5%, respectively, with higher accuracy, sensitivity and specificity compared to mural edema, with higher sensitivity and similar specificity compared to wall thickening (Table 6).
Correlation between endoscopic, clinical and MRE scores
Rationality of clinical, endoscopic and MRE scores/findings in recognition of severity of IBD utilizing pathology as the gold standard were compared in (Table 6). Wall thickening and MRE severity score revealed higher accuracy as (95.8%) with 87.5%, 80%, 96% and 94.1% for sensitivity, specificity, PPV and NPV, respectively. The Endoscopic activity score revealed higher specificity (87.5%) and less sensitivity (85%) compared to MRE scores.
Our results revealed significant positive moderate and very high correlation between MRE score and clinical scores among total cases and CD cases, respectively (r = 0.489 and 0.806, p = 0.015 and 0.009, respectively), while there was nonsignificant low correlation between both scores among UC cases (r = 0.291, p = 0.292) (Fig. 4).
There was significant positive correlation between MRE score and endoscopic scores in all groups with moderate correlation among total cases and UC cases, respectively (r = 0.559 and 0.544, p = 0.005 and 0.036, respectively) and very high correlation in CD cases (r = 0.790, p < 0.001) (Fig. 5).
Also, there was significant positive correlation between MRE score and pathological scores in all groups with very high correlation among total cases and CD cases, respectively (r = 0.814 and 0.878, p < 0.001 and 0.002, respectively) and high correlation in UC cases (r = 0.775, p = 0.001) (Fig. 6).
Discussion
Pediatric MRE is the optimal imaging method for detection IBD activity and has been progressively more utilized in the assessment of IBD in the last decade [22]. MRE is predicted to have better impact via detection of transmural disease not willing to endoscopic evaluation [10, 23].
Our MRE results revealed perfect inter-observer agreement concerning mural edema and wall thickening, substantial agreement for MRE severity score, mural diffusion restriction, vascular congestion and disease extent. There was statistically significant difference between UC and CD regarding mural edema. That was in line with previous meta-analysis study, revealing that mural thickening and DWI are characteristic for active inflammation [24]. Also, another retrospective study showed moderate to good inter-observer agreement for the inflammatory MRE features in CD patients [25].
Another recent study concluded similar results, they revealed that focal mural enhancement with wall thickening, mural edema and restricted diffusion were moderately correlated to CD [19]. Also similar results were conducted by another study, compared to MRE results in CD cases with surgically excised small bowel strictures and confirmed the presence of mural inflammation and damage [26].
Our results revealed that MRE severity score and wall thickening had higher accuracy for detection disease severity. This is in concordance with another study which considered mural thickening the primary imaging biomarkers of active inflammation on MRE in children with CD [27].
Pediatric UC is often more extensive at diagnosis than adults UC, it may present as pancolitis in 60% of patients [28]. Our results confirmed that MRE can detect terminal ileal changes in children with UC. The abnormal inflammation of the terminal ileum detected radiologically or endoscopically in UC patients is named as backwash ileitis [29], this ileitis occurs mainly in cases with extensive colitis [30].
Our results revealed substantial inter-observer agreement for mural diffusion restriction on DW images with higher sensitivity, specificity and accuracy than mural edema detected on MRE, that was in concordance with another study which revealed very good sensitivity, specificity, PPV, NPV and accuracy of diffusion compared to contrast-enhanced MRI as 90%, 98%, 90%, 98% and 96%, respectively [14]. Also few other studies revealed similar results with good performance of DWI compared to contrast-enhanced MRE [13, 13].
Our results also confirmed that DWI can accurately detect inflamed bowel segments, that was in line with previous study which considered increased wall thickness and restricted diffusion were the better predictors of active inflammation [31].
The strength in our study is besides the perfect inter-observer agreement concerning mural edema and wall thickening with substantial inter-observer agreement for MRE severity score, mural diffusion restriction and disease extent, our results revealed high accuracy MRE compared to endoscopic findings and clinical activity scores with significant positive correlation. Thus, MRE provides an applicable adequate radiological assessment to predict severity of pediatric IBD. Incorporating the DWI analysis in the MRE score may supply additional data with consequent clinical management especially in situations when IV contrast agents are contraindicated.
Our study has few limitations; firstly, the relatively small number of the patients. However, the number of our cases is greater than that in previous studies [20, 21]. Secondly, in the single-center design of our study, further multicenter studies could add more data. Thirdly, DWI interpretation was based on qualitative analysis without quantitative DWI analysis. Future further studies with quantitative evaluation could be helpful.
Conclusions
The magnetic resonance enterography is a reliable noninvasive imaging modality for diagnosis of pediatric IBD. MRE revealed significant positive very high correlation with clinical score, SES-CD and pathology activity among CD patients, while MRE revealed significant positive correlation only with Mayo endoscopic score and pathology activity among UC patients.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- CD:
-
Crohn’s disease
- DWI:
-
Diffusion-weighted imaging
- MRE:
-
Magnetic resonance enterography
- MEGS:
-
Magnetic resonance enterography global score
- SES-CD:
-
Simplified endoscopic activity score for Crohn’s disease
- UC:
-
Ulcerative colitis
References
Thurgate LE, Lemberg DA, Day AS, Leach ST (2019) An overview of inflammatory bowel disease unclassified in children. Inflamm Intest Dis 4(3):97–103
Zheng X, Li M, Wu Y, Lin X, Zhang Z, Zheng W et al (2020) Assessment of pediatric Crohn’s disease activity: validation of the magnetic resonance enterography global score (MEGS) against endoscopic activity score (SES-CD). Abdom Radiol 45:3653–3661
Deepak P, Axelrad JE, Ananthakrishnan AN (2019) The role of the radiologist in determining disease severity in inflammatory bowel diseases. Gastrointest Endosc Clin 29(3):447–470
Harrington SG, Johnson MK, Greer MLC, Gee MS (2020) Pearls and Pitfalls in MR Enterography Interpretation for Pediatric Patients. In: Seminars in Ultrasound, CT and MRI. Elsevier. pp 462–71
Kaushal P, Somwaru AS, Charabaty A, Levy AD (2017) MR enterography of inflammatory bowel disease with endoscopic correlation. Radiographics 37(1):116–131
Guglielmo FF, Anupindi SA, Fletcher JG, Al-Hawary MM, Dillman JR, Grand DJ et al (2020) Small bowel Crohn disease at CT and MR enterography: imaging atlas and glossary of terms. Radiographics 40(2):354–375
Miles A, Bhatnagar G, Halligan S, Gupta A, Tolan D, Zealley I et al (2019) Magnetic resonance enterography, small bowel ultrasound and colonoscopy to diagnose and stage Crohn’s disease: patient acceptability and perceived burden. Eur Radiol 29(3):1083–1093
Puylaert CAJ, Tielbeek JAW, Bipat S, Stoker J (2015) Grading of Crohn’s disease activity using CT, MRI, US and scintigraphy: a meta-analysis. Eur Radiol 25(11):3295–3313
Sturm A, Maaser C, Calabrese E, Annese V, Fiorino G, Kucharzik T et al (2019) ECCO-ESGAR Guideline for Diagnostic Assessment in IBD Part 2: IBD scores and general principles and technical aspects. J Crohn’s Colitis 13(3):273–284
Greer MLC (2018) Paediatric magnetic resonance enterography in inflammatory bowel disease. Eur J Radiol 102:129–137
Prezzi D, Bhatnagar G, Vega R, Makanyanga J, Halligan S, Taylor SA (2016) Monitoring Crohn’s disease during anti-TNF-α therapy: validation of the magnetic resonance enterography global score (MEGS) against a combined clinical reference standard. Eur Radiol 26(7):2107–2117
Maccioni F, Bencardino D, Buonocore V, Mazzamurro F, Viola F, Oliva S et al (2019) MRI reveals different Crohn’s disease phenotypes in children and adults. Eur Radiol 29(9):5082–5092
Seo N, Park SH, Kim K-J, Kang B-K, Lee Y, Yang S-K et al (2016) MR enterography for the evaluation of small-bowel inflammation in Crohn disease by using diffusion-weighted imaging without intravenous contrast material: a prospective noninferiority study. Radiology 278(3):762–772
Khachab F, Loundou A, Roman C, Colavolpe N, Aschero A, Bourlière-Najean B et al (2018) Can diffusion weighting replace gadolinium enhancement in magnetic resonance enterography for inflammatory bowel disease in children? Pediatr Radiol 48(10):1432–1440
Dubron C, Avni F, Boutry N, Turck D, Duhamel A, Amzallag-Bellenger E (2016) Prospective evaluation of free-breathing diffusion-weighted imaging for the detection of inflammatory bowel disease with MR enterography in childhood population. Br J Radiol 89(1060):20150840
Watson T, McHugh K (2019) Paediatric bowel imaging special issue. Eur J Radiol 118:65
Kerur B, Litman HJ, Stern JB, Weber S, Lightdale JR, Rufo PA et al (2017) Correlation of endoscopic disease severity with pediatric ulcerative colitis activity index score in children and young adults with ulcerative colitis. World J Gastroenterol 23(18):3322
Daperno M, D’Haens G, Van Assche G, Baert F, Bulois P, Maunoury V et al (2004) Development and validation of a new, simplified endoscopic activity score for Crohn’s disease: the SES-CD. Gastrointest Endosc 60(4):505–512
Bruining DH, Zimmermann EM, Loftus EV Jr, Sandborn WJ, Sauer CG, Strong SA et al (2018) Consensus recommendations for evaluation, interpretation, and utilization of computed tomography and magnetic resonance enterography in patients with small bowel Crohn’s disease. Gastroenterology 154(4):1172–1194
Makanyanga JC, Pendsé D, Dikaios N, Bloom S, McCartney S, Helbren E et al (2014) Evaluation of Crohn’s disease activity: initial validation of a magnetic resonance enterography global score (MEGS) against faecal calprotectin. Eur Radiol 24(2):277–287
Schooler GR, Hull NC, Mavis A, Lee EY (2019) MR imaging evaluation of inflammatory bowel disease in children: where are we now in 2019. Magn Reson Imaging Clin 27(2):291–300
Ng SC, Shi HY, Hamidi N, Underwood FE, Tang W, Benchimol EI et al (2017) Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet 390(10114):2769–2778
Erden A, Kuru Öz D, Gürsoy Çoruh A, Erden İ, Özalp Ateş FS, Törüner M (2019) Backwash ileitis in ulcerative colitis: Are there MR enterographic features that distinguish it from Crohn disease? Eur J Radiol 110:212–218
Church PC, Turner D, Feldman BM, Walters TD, Greer M, Amitai MM et al (2015) Systematic review with meta-analysis: magnetic resonance enterography signs for the detection of inflammation and intestinal damage in Crohn’s disease. Aliment Pharmacol Ther 41(2):153–166
Church PC, Greer M-LC, Cytter-Kuint R, Doria AS, Griffiths AM, Turner D et al (2017) Magnetic resonance enterography has good inter-rater agreement and diagnostic accuracy for detecting inflammation in pediatric Crohn disease. Pediatr Radiol 47(5):565–575
Barkmeier DT, Dillman JR, Al-Hawary M, Heider A, Davenport MS, Smith EA et al (2016) MR enterography–histology comparison in resected pediatric small bowel Crohn disease strictures: can imaging predict fibrosis? Pediatr Radiol 46(4):498–507
Gale HI, Sharatz SM, Taphey M, Bradley WF, Nimkin K, Gee MS (2017) Comparison of CT enterography and MR enterography imaging features of active Crohn disease in children and adolescents. Pediatr Radiol 47(10):1321–1328
Siow VS, Bhatt R, Mollen KP (2017) Management of acute severe ulcerative colitis in children. Semin Pediatr Surg 26(6):367–372
Bousvaros A, Antonioli DA, Colletti RB, Dubinsky MC, Glickman JN, Gold BD et al (2007) Differentiating ulcerative colitis from Crohn disease in children and young adults: report of a working group of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition and the Crohn’s and Colitis Foundation of America. J Pediatr Gastroenterol Nutr 44(5):653–674
Paine ER (2014) Colonoscopic evaluation in ulcerative colitis. Gastroenterol Rep 2(3):161–168
Barber JL, Lozinsky AC, Kiparissi F, Shah N, Watson TA (2016) Detecting inflammation in the unprepared pediatric colon: how reliable is magnetic resonance enterography? Pediatr Radiol 46(5):646–652
Acknowledgements
Not applicable.
Funding
This study did not receive funding.
Author information
Authors and Affiliations
Contributions
All authors have read and approved the manuscript. Study concept and design was proposed by GAS and AAA. SIA and GAS helped in database search. GAS and AAA contributed to image analysis and interpretation of data. Clinical assessment was done by SIA, AM and MAS. AM was involved in endoscopic analysis. GAS and AM helped in revision of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate:
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. The study was approved by the Institutional review board of Mansoura University (Approval No: MS.17.12.37). A written informed consent was obtained from all patients.
Consent for publication
The participants in the study were informed and consented the possibility of research publication.
Competing interests
The authors declare that they have no competing interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Saleh, G.A., Razek, A.A.K.A., Awad, S.I. et al. The role of magnetic resonance enterography and diffusion-weighted imaging in pediatric inflammatory bowel disease compared to endoscopic and clinical activity scores: pilot study. Egypt J Radiol Nucl Med 54, 204 (2023). https://doi.org/10.1186/s43055-023-01148-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-023-01148-0