Abstract
Objectives
To identify differences between two cohorts of adult and pediatric patients affected by Crohn’s disease (CD), with regard to lesion location in the small intestine and colon-rectum, lesion activity, and prevalence of perianal disease (PD), using MRI as the main diagnostic tool.
Methods
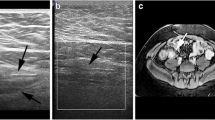
We retrospectively reviewed 350 consecutive MRI examinations performed between 2013 and 2016 in outpatients or inpatients with histologically proven CD, monitored by the Gastroenterology and Pediatric Units of our Hospital. The magnetic resonance enterography (MRE) protocol for adult and pediatric CD patients routinely includes evaluation of nine different intestinal segments (from jejunum to rectum) and of the anal canal. Intestinal activity was also calculated using a validated score. Perianal disease (PD) was staged. Fisher’s exact test was used and the odds ratio (OR) was calculated.
Results
Two hundred and nineteen out of 350 MRI studies (118 adults and 101 children) were included. The prevalence of PD was 34.6% in children and 16.1% in adults (OR = 2.8; p = 0.0017). Pediatric patients showed more frequent rectal involvement (29.7% vs 13.5%, OR = 2.7; p = 0.0045) and higher risk of PD in the presence of rectal disease (p = 0.043; OR = 4.5). In pediatric patients with severe colorectal disease, the prevalence of PD was twofold (86.7% vs 40%; p = 0.072). Using the clinical Montreal classification for lesion location, no significant differences emerged between the two patient populations.
Conclusions
MRI showed a significantly higher prevalence of rectal involvement and perianal disease in the pediatric population. These results may have a relevant clinical impact and deserve further investigation.
Key Points
• To our knowledge, this is the largest morphological comparative study available in the literature using MRI as the main diagnostic tool to compare adult patients and children with Crohn’s disease.
• Our study showed significant differences between adults and children: a higher prevalence of rectal and perianal fistulous disease (PD) in pediatric patients and an increased prevalence of PD in the presence of severe colon-rectum involvement.
• The association of rectal and perianal disease implies a poorer clinical prognosis and a higher risk of disabling complications in pediatric patients.






Similar content being viewed by others
Abbreviations
- CD:
-
Crohn’s disease
- CI:
-
Confidence interval
- DWI:
-
Diffusion-weighted imaging
- HASTE:
-
Half-Fourier acquisition single shot turbo spin echo
- HRMRI:
-
High-resolution magnetic resonance imaging
- MEGS:
-
Magnetic resonance enterography global score
- MRE:
-
Magnetic resonance enterography
- MRI:
-
Magnetic resonance imaging
- OR:
-
Odds ratio
- PD:
-
Perianal disease
- SJH:
-
St. James Hospital
- TrueFISP:
-
True fast imaging with steady-state free precession
- VIBE:
-
Volumetric interpolated breath-hold examination
References
Benchimol EI, Fortinsky KJ, Gozdyra P, Van den Heuvel M, Van Limbergen J, Griffiths AM (2011) Epidemiology of pediatric inflammatory bowel disease: a systematic review of international trends. Inflamm Bowel Dis 17:423–439
Van Limbergen J, Russell RK, Drummond HE et al (2008) Definition of phenotypic characteristics of childhood-onset inflammatory bowel disease. Gastroenterology 135:1114–1122
Vernier-Massouille G, Balde M, Salleron J et al (2008) Natural history of pediatric Crohn’s disease: a population-based cohort study. Gastroenterology 135(4):1106–1113
Goodhand J, Hedin CR, Croft NM, Lindsay JO (2011) Adolescents with IBD: the importance of structured transition care. J Crohns Colitis 5:509–519
Duricova D, Burisch J, Jess T, Gower-Rousseau C, Lakatos PL, ECCO-EpiCom (2014) Age-related differences in presentation and course of inflammatory bowel disease: an update on the population-based literature. J Crohns Colitis 8:1351–1361
Kim HJ, Oh SH, Kim DY et al (2017) Clinical characteristics and long-term outcomes of paediatric Crohn’s disease: a single-centre experience. J Crohns Colitis 11(2):157–164
Duricova D, Fumery M, Annese V, Lakatos PL, Peyrin-Biroulet L, Gower-Rousseau C (2017) The natural history of Crohn’s disease in children: a review of population-based studies. Eur J Gastroenterol Hepatol 29(2):125–134
Herzog D, Fournier N, Buehr P et al (2017) Prevalence of intestinal complications in inflammatory bowel disease: a comparison between paediatric-onset and adult-onset patients. Eur J Gastroenterol Hepatol 29(8):926–931
Jakobsen C, Bartek J Jr, Wewer V et al (2011) Differences in phenotype and disease course in adult and paediatric inflammatory bowel disease--a population-based study. Aliment Pharmacol Ther 34(10):1217–1224
Satsangi J, Silverberg MS, Vermeire S, Colombel JF (2006) The Montreal classification of inflammatory bowel disease: controversies, consensus, and implications. Gut 55(6):749–753
Levine A, Griffiths A, Markowitz J et al (2011) Pediatric modification of the Montreal classification for inflammatory bowel disease: the Paris classification. Inflamm Bowel Dis 17(6):1314–1321
Müller KE, Lakatos PL, Arató A et al (2013) Incidence, Paris classification, and follow-up in a nationwide incident cohort of pediatric patients with inflammatory bowel disease. J Pediatr Gastroenterol Nutr 57:576–582
De Bie CI, Paerregaard A, Kolacek S et al (2013) Disease phenotype at diagnosis in pediatric Crohn’s disease: 5-year analyses of the EUROKIDS Registry. Inflamm Bowel Dis 19(2):378–385
Lee YA, Chun P, Hwang EH, Mun SW, Lee YJ, Park JH (2016) Clinical features and extraintestinal manifestations of Crohn disease in children. Pediatr Gastroenterol Hepatol Nutr 19(4):236–242
Assa A, Amitai M, Greer ML et al (2017) ImageKids study group. Perianal pediatric Crohn’s disease is associated with a distinct phenotype and greater inflammatory burden. J Pediatr Gastroenterol Nutr 65(3):293–298
Schwartz DA, Loftus EV Jr, Tremaine WJ et al (2002) The natural history of fistulizing Crohn’s disease in Olmsted County, Minnesota. Gastroenterology 122:875–880
Panés J, Rimola J (2017) Perianal fistulizing Crohn's disease: pathogenesis, diagnosis and therapy. Nat Rev Gastroenterol Hepatol 14(11):652–664
Hellers G, Bergstrand O, Ewerth S, Holmström B (1980) Occurrence and outcome after primary treatment of anal fistulae in Crohn’s disease. Gut 21:525–527
Zwintscher NP, Shah PM, Argawal A et al (2015) The impact of PD in young patients with inflammatory bowel disease. Int J Colorectal Dis 30(9):1275–1279
Safar B, Sands D (2007) Perianal Crohn’s disease. Clin Colon Rectal Surg 20(4):282–293
Kaur M, Panikkath D, Yan X et al (2016) Perianal Crohn’s disease is associated with distal colonic disease, stricturing disease behavior, IBD-associated serologies and genetic variation in the JAK-STAT pathway. Inflamm Bowel Dis 22(4):862–869
Essary B, Kim J, Anupindi S, Katz JA, Nimkin K (2007) Pelvic MRI in children with Crohn disease and suspected perianal involvement. Pediatr Radiol 37(2):201–208
Haggett PJ, Moore NRN, Shearman JD, Travis SP, Jewell DP, Mortensen NJ (1995) Pelvic and perineal complications of Crohn’s disease: assessment using magnetic resonance imaging. Gut 36:407–410
Levine A, Koletzko S, Turner D et al (2014) ESPGHAN revised Porto criteria for the diagnosis of inflammatory bowel disease in children and adolescents. J Pediatr Gastroenterol Nutr 58(6):795–806
Panes J, Bouhnik Y, Reinisch W et al (2013) Imaging techniques for assessment of inflammatory bowel disease: joint ECCO and ESGAR evidence-based consensus guidelines. J Crohns Colitis 7:556–585
Civitelli F, Casciani E, Maccioni F et al (2015) Use of imaging techniques in inflammatory bowel diseases that minimize radiation exposure. Curr Gastroenterol Rep 17(7):28
Maccioni F, Al Ansari N, Mazzamurro F et al (2014) Detection of Crohn disease lesions of the small and large bowel in pediatric patients: diagnostic value of MR enterography versus reference examinations. AJR Am J Roentgenol 203(5):W533–W542
Church PC, Greer MC, Cytter-Kuint R et al (2017) Magnetic resonance enterography has good inter-rater agreement and diagnostic accuracy for detecting inflammation in pediatric Crohn disease. Pediatr Radiol 47(5):565–575
Gomollón F, Dignass A, Annese V et al (2017) 3rd European evidence-based consensus on the diagnosis and management of Crohn’s disease 2016: Part 1: Diagnosis and medical management. J Crohns Colitis 11(1):3–25
Maccioni F, Viscido A, Broglia L et al (2000) Evaluation of Crohn disease activity with magnetic resonance imaging. Abdom Imaging 25(3):219–228
Rimola J, Ordás I, Rodriguez S et al (2011) Magnetic resonance imaging for evaluation of Crohn’s disease: validation of parameters of severity and quantitative index of activity. Inflamm Bowel Dis 17(8):1759–1768
Tielbeek JA, Makanyanga JC, Bipat S et al (2013) Grading Crohn disease activity with MRI: interobserver variability of MRI features, MRI scoring of severity, and correlation with Crohn disease endoscopic index of severity. AJR Am J Roentgenol 201(6):1220–1228
Steward MJ, Punwani S, Proctor I et al (2012) Non-perforating small bowel Crohn’s disease assessed by MRI enterography: derivation and histopathological validation of an MR-based activity index. Eur J Radiol 81(9):2080–2088
Maccioni F, Bruni A, Viscido A et al (2006) MR imaging in patients with Crohn disease: value of T2- versus T1-weighted gadolinium-enhanced MR sequences with use of an oral superparamagnetic contrast agent. Radiology 238(2):517–530 Erratum in: Radiology. 2013 Aug;268(2):614
Prezzi D, Bhatnagar G, Vega R, Makanyanga J, Halligan S, Taylor SA (2015) Monitoring Crohn’s disease during anti-TNF-alpha therapy: validation of the magnetic resonance enterography global score (MEGS) against a combined clinical reference standard. Eur Radiol 26 (7):2107–2117
Makanyanga JC, Pendsé D, Dikaios N et al (2014) Evaluation of Crohn’s disease activity: initial validation of a magnetic resonance enterography global score (MEGS) against faecal calprotectin. Eur Radiol 24(2):277–287
Parks AG, Gordon PH, Hardcastle JD (1976) A classification of fistula-in-ano. Br J Surg 63:1–12
Morris J, Spencer JA, Ambrose NS (2000) MR imaging classification of perianal fistulas and its implications for patient management. Radiographics 3:623–635
Maccioni F, Viola F, Carrozzo F et al (2012) Differences in the location and activity of intestinal Crohn’s disease lesions between adult and paediatric patients detected with MRI. Eur Radiol 22:2465–2477
Ye BD, Yang SK, Cho YK et al (2010) Clinical features and long-term prognosis of Crohn’s disease in Korea. Scand J Gastroenterol 45:1178–1185
Ruel J, Ruane D, Mehandru S, Gower-Rousseau C, Colombel JF (2014) IBD across the age spectrum: is it the same disease? Nat Rev Gastroenterol Hepatol 11(2):88–98
Weiser M, Simon JM, Kochar B et al (2018) Molecular classification of Crohn’s disease reveals two clinically relevant subtypes. Gut 67:36–42
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Francesca Maccioni.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• retrospective
• observational
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOC 61 kb)
Rights and permissions
About this article
Cite this article
Maccioni, F., Bencardino, D., Buonocore, V. et al. MRI reveals different Crohn’s disease phenotypes in children and adults. Eur Radiol 29, 5082–5092 (2019). https://doi.org/10.1007/s00330-019-6006-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-019-6006-5