Abstract
Background
Cystic lymphangiomas are benign vascular malformations of lymphatic differentiation. They usually occur in childhood and are commonly seen in the head and neck region. Lymphangioma of the gallbladder is extremely rare, and only a handful of cases have been reported in the literature.
Case presentation
A 56-year-old female presented to the outpatient department for evaluation of right upper quadrant abdominal pain which had been bothering her for the past few months. Abdominal ultrasonography revealed an ill-defined septated cystic lesion surrounding the gallbladder (GB) which was initially thought to be a collection. However, contrast-enhanced computed tomography of abdomen showed a well-marginated fluid density lesion in the gall bladder fossa which was insinuating around the gall bladder and was encasing it. No intralesional enhancement was seen after contrast administration. MRI confirmed the well-defined, multiseptated lesion without any solid component in the gall bladder fossa encasing the GB but without any abnormal communication with the biliary tree. Therefore, a final diagnosis of slow flow lymphatic malformation was formulated. The patient underwent exploratory laparotomy, and the mass was resected en bloc with the GB. Histological evaluation was consistent with lymphatic malformation.
Conclusions
GB lymphangioma is a rare entity and is difficult to diagnose. While the imaging characteristics are essentially similar to lymphangiomas elsewhere in the body, the location is peculiar and should warrant a thorough evaluation by the means of CT and more importantly MRI.
Similar content being viewed by others
Background
Lymphangioma is an infrequent congenital anomaly which, as per name, arises from the lymphatics. According to the classification proposed by International Society for the Study of Vascular Anomalies, lymphangioma is a benign lesion of vascular origin showing lymphatic differentiation, rather than a vascular tumor [1]. It is commonly seen in the skin and deeper tissues of the head, neck and axillary region. The rarer sites include the lungs, pleura, pericardium, gastrointestinal tract, hepatobiliary system as well as the kidneys. Lymphangioma of gall bladder (GB) is very rare, and only a few cases have been reported in the literature till date [2,3,4,5,6,7,8]. Cross-sectional imaging plays an important role in accurately diagnosing GB lymphangioma, with magnetic resonance imaging (MRI) and magnetic resonance cholangiopancreatography (MRCP) proving immensely helpful in characterizing the lesion and assessing its relations to adjacent organs. Complete surgical resection remains the treatment of choice with good overall prognosis. This case report aims to reinforce the role of imaging in diagnosis of such unique entity.
Case presentation
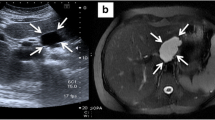
A 56-year-old female presented to the outpatient department for evaluation of right upper quadrant abdominal pain which had been troubling her for the past few months. She did not have any prior history of abdominal trauma or past history of cholecystitis. No history of surgical intervention was present. On general physical examination, the patient was afebrile with normal vital parameters. Abdominal examination revealed a soft abdomen with no guarding or distension. An ultrasound of the abdomen was advised along with few blood tests. Laboratory tests revealed normal hemogram, liver function tests, serum amylase and lipase. Abdominal ultrasonography (USG) showed an ill-defined septated cystic lesion measuring 2.5 × 1.5 × 6 cm, surrounding the gallbladder (GB) without any appreciable mass effect (Fig. 1a, b). No intraluminal calculi were seen in the GB lumen. GB wall thickness was also normal. Contrast-enhanced computed tomography (CECT) abdomen was advised for further evaluation and was performed on a 128 slice scanner both before and after administration of iodinated contrast agent. It showed a well-marginated fluid density lesion in the gall bladder fossa which was insinuating around the gall bladder and was encasing it (Fig. 2a, b). No intralesional enhancement was seen after contrast administration. No focal breach or abnormal wall thickening was seen in the GB, and no intraluminal hyperdensities were noted. CT findings and the insidious nature of her symptomatology raised the possibility of a non-infectious, non-inflammatory etiology, and an upper abdomen MRI was planned for the patient. MRI was performed on a 1.5-Tesla scanner and confirmed the well-defined, multiseptated lesion without any solid component in the gall bladder fossa encasing the GB (Fig. 3a). On MRCP images (Fig. 3b) no abnormal communication with the biliary tree could be elicited. The lesion showed no fat, hemorrhagic or calcific foci. No abnormal vessels or flow voids were seen. Both CT and MRI scans were read by a radiologist with 7 years of experience. A final diagnosis of slow flow vascular malformation was formulated likely of lymphatic origin. The patient underwent an exploratory laparotomy, and the mass was resected en bloc with the GB. Histological evaluation of the cystic mass was consistent with lymphatic malformation (Fig. 4).
A Axial contrast-enhanced computed tomography image shows a low-density multilocular cystic lesion (*) originating from the gallbladder fossa and surrounding the gall bladder (GB). GB wall shows normal thickness and enhancement. B Sagittal contrast-enhanced computed tomography image shows a low-density multilocular cystic lesion (*) with septations (arrow) encasing the gallbladder (GB)
A Axial T2-weighted magnetic resonance image showing a thin multi-septated cystic lesion (*) in gall bladder fossa. Gall bladder (GB) wall appears smooth and normal in thickness. No intraluminal calculi seen. B Magnetic resonance cholangiopancreatography (MRCP) image showing gallbladder (GB) completely encased by lesion (*). No communication is seen with biliary system. CBD common bile duct
Discussion
Lymphatic malformations are benign lesions of vascular origin which were erroneously labeled as lymphangiomas in the past implying that these were tumors. However, these entities show lymphatic differentiation and are vascular malformations, rather than vascular tumors as per the 2018 ISSVA classification of vascular anomalies [1].
The etiopathogenesis of lymphatic malformation has two primary explanations. The first explanation states that it is a congenital abnormality which arises due to improper development of local lymphatics leading to inadequate connections between the lymphatic vessels and subsequently causing sequestration of lymphatic tissue. The other explanation considers secondary causes of lymphatic obstruction and damage as the cause of these malformations and mainly attributes it to trauma, inflammation, surgery and radiation [2, 7, 9]. Lymphatic malformations usually occur in childhood and are located in the head and neck region in majority of the cases (95%). Intraabdominal lymphatic malformations are less common, and GB lymphangioma account for 0.8–1% of all intraabdominal lymphangiomas [8].
GB lymphatic malformation is usually asymptomatic and is diagnosed incidentally in adulthood, as was confirmed by Ohba et al. [2], Kim et al. [8] and Shikano et al. [10] in their studies. However, most of the diagnosed patients are usually symptomatic at some point of time in the disease course, and therefore present to the hospital, similar to our case. Preoperative diagnosis of GB lymphangioma is difficult as it is very rare, and imaging studies such as USG and CT cannot distinguish it from other lesions. On USG, it appears as multicystic and multiseptated collection surrounding the GB without any significant mass effect. CECT shows simple or multilocular cystic lesion with the CT attenuation of water. The septa of the cysts are of uniform thickness. The wall of the cysts may enhance following contrast administration. Follow-up CT studies can demonstrate intralesional hemorrhage, which is common; however, if the hemorrhage is present in the initial scan, it could mimic soft tissue. MRI and MRCP are extremely helpful for making the correct diagnosis. The T1- and T2-weighted MR images can clearly depict the lumen of the GB and the multiseptated cystic mass originating in the gallbladder wall. MRCP is helpful in ruling out the communication with the cystic duct and bile duct [9, 11]. Similar to our study, all the case reports reviewed by us, which had a preoperative diagnosis of lymphangioma [8,9,10, 13], utilized MRI for confirmation.
The common imaging differentials include fluid collections like biloma and abscesses as was reported by Bridda et al. [12], while complications include rupture, infection and torsion. Intracystic hemorrhage has also been reported by Choi et al. [9] and Bridda et al. [12] in their case studies. The standard treatment of choice includes total surgical excision. The preoperative evaluation of cystic mass and its relations with adjacent organs is helpful in choosing the surgical method. Small lesions showing clear fat plans with adjacent organs can be successfully treated by laparoscopic cholecystectomy [13]. En bloc resection is needed if the lesion is adherent to extrahepatic bile ducts and adjacent organs [7, 10]. The incomplete resection may lead to recurrence, but if the lesion is completely resected, long-term prognosis is excellent.
Conclusions
GB lymphangioma is a rare entity and is difficult to diagnose especially to the uninitiated mind. While the imaging characteristics are essentially similar to the lymphangiomas elsewhere in the body, the location is peculiar and should always warrant a thorough evaluation by the means of CT and more importantly MRI. Preoperative diagnosis and assessment of anatomy is of great importance and can prove extremely beneficial to the surgical team in decision making.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- GB:
-
Gall bladder
- MRI:
-
Magnetic resonance imaging
- MRCP:
-
Magnetic resonance cholangiopancreatography
- USG:
-
Ultrasonography
- CECT:
-
Contrast-enhanced computed tomography
References
ISSVA Classification of Vascular Anomalies ©2018 International Society for the study of vascular anomalies. Available at “issva.org/classification”. Accessed 28 Jan 2020
Ohba K, Sugauchi F, Orito E, Suzuki K, Ohno T, Mizoguchi N et al (1995) Cystic lymphangioma of the gall-bladder: a case report. J Gastroenterol Hepatol 10:693–696
Chung JH, Suh YL, Park IA, Jang JJ, Chi JG, Kim YI et al (1999) A pathologic study of abdominal lymphangiomas. J Korean Med Sci 14:257–262
Vu A, Tran P, Houli N, Chan S (2018) First reported case in Australia: a rare case of lymphangioma of the gallbladder. ANZ J Surg 89:7–8
Boskovski MT, Saad A, Israel GM, Salem RR (2012) Lymphangioma of the gallbladder in adults: review of the literature and a case report. J Gastrointest Surg 16:663–668
Woo YS, Joo KR, Kim KY, Oh WT, Kim YH (2007) Unusual presentation of cystic lymphangioma of the gallbladder. Korean J Intern Med 22:197–200
Noh KW, Bouras EP, Bridges MD, Nakhleh RE, Nguyen JH (2005) Gallbladder lymphangioma: a case report and review of the literature. J Hepatobiliary Pancreat Surg 12:405–408
Kim JK, Yoo KS, Moon JH et al (2007) Gallbladder lymphangioma: a case report and review of the literature. World J Gastroenterol 13(2):320–323
Choi JY, Kim MJ, Chung JJ, Park SI, Lee JT, Yoo HS et al (2002) Gallbladder lymphangioma: MR findings. Abdom Imaging 27:54–57
Shikano T, Takeda S, Sakai M et al (2008) Cystic lymphangioma of the gallbladder: report of a case. Surg Today 38:81–84
Ellermeier A, Beland MD (2014) Gallbladder lymphangiomas: rare lesions with characteristic imaging features. Ultrasound Q 30:216–218
Bridda A, Dallagnese L, Frego M (2011) Is laparoscopic cholecystectomy safe for lymphangioma of the gallbladder? A complicated case mimicking subhepatic abscess. Updates Surg 66:1–4
Yang HR, Jan YY, Huang SF, Yeh TS, Tseng JH, Chen MF (2003) Laparoscopic cholecystectomy for gallbladder lymphangiomas. Surg Endosc 17:1676
Acknowledgements
Nil.
Funding
No funding available.
Author information
Authors and Affiliations
Contributions
VG involved in substantial contributions to the conception provided, design of the work and manuscript draft. PG involved in substantial contributions to the conception provided, design of the work, interpretation of the data and substantial revision of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The patient included in this study provided the written informed consent to participate in this research.
Consent for publication
The patient included in this research gave a written and informed consent to publish the data contained within this study.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Garg, V., Gupta, P. Cystic lymphangioma of the gall bladder: common disease at uncommon site. Egypt J Radiol Nucl Med 54, 151 (2023). https://doi.org/10.1186/s43055-023-01103-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-023-01103-z