Abstract
Background
Lymphangiomas are benign vascular tumors arising from the lymphatic system. They commonly affect the head and neck regions. Pancreatic involvement is extremely rare. Even though they are rare, it should be considered as a differential diagnosis for patients who present with pancreatic mass.
Case presentation
We report the case of a 6-year-old African male patient who presented with abdominal mass and dull aching pain of 6 months duration. He was examined and underwent excision, with biopsy showing pancreatic lymphangioma.
Conclusion
These tumors are benign and slow growing and have potential to regress spontaneously. Thus, most literature agrees that surgical interventions should be reserved for symptomatic cases.
Similar content being viewed by others
Introduction
Lymphangiomas are benign congenital tumors of lymphatic vascular origin. They commonly affect head and neck regions. Pancreatic involvement is extremely rare. These tumors are usually congenital but can arise as a result of blockage of lymphatic flow from trauma, fibrosis, inflammation, or radiotherapy. Patients are usually asymptomatic but can present with abdominal pain and mass. We report the case of pancreatic lymphangioma in a 6-year-old male patient presenting with abdominal pain and mass.
Case presentation
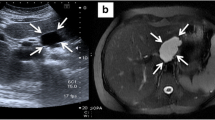
A 6-year-old African male child presented with abdominal mass and dull aching type of abdominal pain of 6 months duration that worsened 1 month before presentation. He had no past medical illness or surgical interventions. He also had no family history of similar illness. Upon our evaluation, the patient was stable. There was an ill-defined, smooth-surface, nontender, fixed, intra-abdominal mass at the center of the abdomen extending to the left upper quadrant measuring about 8 cm × 10 cm. Liver function test, renal function test, pancreatic enzymes, and tumor markers were all in normal range. Abdominal computed tomography (CT) scan showed multiple cystic mass adjacent to each other with no communication between the masses; the largest cyst measured about 8 cm × 7.5 cm × 9.5 cm. The mass was found adjacent to the head of the pancreas with no clear plane between the mass and pancreas (Fig. 1). It was difficult to reach a conclusive diagnosis from the CT scan as there were multiple diagnoses presented to us by the radiologist, including pseudocyst and duodenal duplication, but the senior radiologist raised the possibility of pancreatic lymphangioma. Since the patient had severe abdominal pain, we opted to explore this patient despite diagnostic dilemma.
The patient was operated, with an intraoperative finding of well-capsulated multiloculated cystic mass that was wrapped with pancreatic tissue and no sign of local invasion (Fig. 2). The mass had no invasion to major structures, and so it was gently mobilized from the pancreatic bed, completely excised without spillage, and sent for histopathology evaluation; The result confirms cystic lymphangioma. The patient was discharged improved and is currently on follow-up with smooth postoperative course, and there are no signs of recurrence.
Discussion
Lymphangiomas are benign vascular tumors arising from the lymphatic system [1]. They account for about 5% of tumors in children and are commonly found in the head and neck region [2]. Other sites reported in the literature include pleura, pericardium, groin, bones, liver, spleen, pancreas, colon, omentum, and genital organ [4].
Pancreatic lymphangioma is a very rare tumor accounting for less than 1% of abdominal lymphangioma and less than 0.5% of all cystic pancreatic lesion [3]. These tumors result from lymphangiectasia as a consequence of a blockage of lymphatic flow. This may be associated with congenital malformations or obstructions as a result of an inflammatory process, radiotherapy, surgery, or any abdominal trauma [3]. It is more common in the pediatrics population, which is similar in our case and has a slight female preponderance [1].
These tumor are benign in nature, slowly growing, and usually asymptomatic [6]. Some patients present with abdominal pain and associated abdominal mass [6,7,8], as does our patient.
There are no associated laboratory findings specific to this abnormality. Abdominal imaging such as ultrasound and CT scan assist in the diagnosis and evaluation of such lesions; however, imaging by itself is not 100% specific to differentiate lymphangiomas from other cystic pancreatic lesions such as pseudocysts, cystadenomas, congenital cysts, and ductal carcinomas. Thus, this pathology can be differentiated from other cystic pancreatic lesions by histopathologic examination [3, 9, 10]. On abdominal ultrasound, the typical presentation of lymphangioma is multilocular lesion with homogeneous serous composition that appears anechoic. CT scan revealed a multiloculated cystic mass with fluid attenuation, thin septa within the lesion, and nonenhancing with no solid component or calcification seen. The tumor does not invade adjacent structures, which was similar to our patient’s CT scan.
Pathologically, lymphangioma can be classified as macrocystic, microcystic, or mixed-type lymphangioma. Macrocystic lymphangiomas are greater than 1 cm in diameter and occur in areas with loose connective tissue such as in the abdomen, neck, and axilla, while microcystic lymphangiomas are less than 1 cm in diameter and arise in areas with dense connective tissue such as tongue and lip. The natural history of lymphangioma depends on its histology type. Macrocystic and mixed types can spontaneously regress, while microcystic lymphangioma does not regress. Therefore macrocystic and mixed types can be serially followed in asymptomatic patients with stable tumor [6, 10].
Surgical interventions are reserved for patients with symptomatic pancreatic lymphangioma and for those with diagnostic dilemmas. Excision of the mass is considered to be curative. As there is a high chance of recurrence, the mass should be removed in its entirety [2, 3, 5]. We have also removed the mass as a whole in our case. Some patients might also require extensive pancreatic resections such as Whipple procedure or distal pancreatectomy depending on the size and location of the mass [3].
Conclusion
Pancreatic lymphangioma, even though it is a rare tumor, should be considered as a differential diagnosis in patients who present with cystic pancreatic mass. This tumor is benign and slow growing and has the potential to regress. Thus, surgical interventions should be reserved for symptomatic cases.
Availability of data and materials
All data and materials are available upon request by the Editor-in-Chief.
References
Afzal S, Masroor I, Shafqat G. Pancreatic lymphangioma. J Coll Phys Surg Pak. 2014; 24.
Kouame DKAS et al. Cystic lymphangioma of the pancreas: about a case and literature review. Int J Innov Res Med Sci. 2021;6.
Ray R, Baruah TD, Mahobia HS, Borkar A. Pancreatic lymphangioma: an unusual cause of abdominal lump. Cureus. 2021. https://doi.org/10.7759/cureus.19452.
Viscosi F, Fleres F, Mazzeo C, Vulcano I, Cucinotta E. Cystic lymphangioma of the pancreas: a hard diagnostic challenge between pancreatic cystic lesions-review of recent literature. Gland Surg. 2018;7:487.
Anbardar MH, Soleimani N, Vahedi AA, Malek-Hosseini SA. Large cystic lymphangioma of pancreas mimicking mucinous neoplasm: case report with a review of histological differential diagnosis. Int Med Case Rep J. 2019;12:297.
Ojha S, et al. Pancreatic cystic lymphangioma: case report and literature review. J Curr Surg. 2021;11:24.
Raval M, Goyal P, Shah T. Giant pancreatic lymphangioma with mesenteric extension—a case report. Egypt J Radiol Nucl Med. 2016;47:1207.
Bellido Luque JA, Garcia Reyes A, Nogales Muñoz A. Giant pancreatic cystic lymphangioma. Rev Esp Enferm Dig. 2020. https://doi.org/10.17235/reed.2020.7003/2020.
Abdelkader A, Hunt B, Hartley CP, Panarelli NC, Giorgadze T. Cystic lesions of the pancreas differential diagnosis and cytologic–histologic correlation. Arch Pathol Lab Med. 2020;144:47.
Jayappa SN, Rao P, Tandon AS, Bharathy KGS, Sikora SS. Large cystic lymphangioma of the pancreas: a case report. Ann R Coll Surg Engl. 2018;100:e12.
Acknowledgements
We would like to thank the parents for giving us consent to use both the child’s history and the different pictures. We hope this will add some light to this rare disease. Lastly, we would like to thank the college for allowing us to publish this paper.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
All authors contributed and review of different articles. MT wrote the case presentation and wrote the draft of the case report, GB operated on the patient and compiled different articles pertaining to the case, and AH wrote the final case report and is also following the patient. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Both ethical clearance and consent to participate were approved by the institutional review board of the surgical department for this case report.
Consent for publication
Written informed consent was obtained from the patient’s legal guardian for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Assefa, H.G., Merga, T.G. & Godu, B.G. Cystic pancreatic lymphangioma: a case report. J Med Case Reports 17, 23 (2023). https://doi.org/10.1186/s13256-022-03730-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13256-022-03730-y