Abstract
Background
Persistent Mullerian Duct Syndrome (PMDS) is a type of pseudo-hermaphroditism occurring in males internally due to failure in the Anti Mullerian Hormone (AMH)-dependent sex differentiation pathway. Due to absent Anti Mullerian Hormone (AMH), the adult male has both the Wolffian and Mullerian duct derivatives. Considering the limited information available in the existing literature, malignant transformation in PMDS has rarely been reported.
Case Presentation
In this article we present two cases of PMDS which have complicated in to malignancy with review of literature and histopathological correlation. Both of these patients presented with lower abdominal pain, for which computed tomography of abdomen and pelvis was performed following ultrasound of abdomen and pelvis Both the Wolffian and Mullerian duct derivates were visualized on the above mentioned scans in these genetically confirmed males (46 XY).
Conclusion
Familiarity with PMDS is necessary to diagnose the condition. Hence, in this article, we report recherche presentations of Persistent Mullerian Duct Syndrome which had complicated into malignancies.
Similar content being viewed by others
Background
The uterus, salpinges and/or the upper part of the vagina, referred to as the Mullerian duct derivatives when present in a phenotypical male human being with a 46 XY karyotype is known as Persistent Mullerian Duct Syndrome (PMDS). Its incidence is not accurately determined but has a reputation for being known as a rare condition. This condition is seldom misdiagnosed due to a lack of familiarity with the condition. We report two recherche/rare cases of PMDS to stress the importance of a radiologists’s role in diagnosing this condition. A review of literature showed only about 20 case reports from India including familial cases. Either one or both of these hormones (Anti Mullerian hormone [AMH] and Testosterone) are affected in males with Disorders of sex development (DSD). PMDS belongs to the first category: AMH is either not secreted (deficiency of AMH) or is inactive (due to a defect in the AMH type II receptor), while testosterone is normally produced and metabolized. Even though external virilisation is complete, the Mullerian duct derivatives do not degenerate and are seen side by side with the testes and male excretory ducts (Fig. 1).
On the other hand, for a quick overview on endodermal sinus tumour, it is a type of germ cell tumour (yolk sac tumour) which includes malignant endodermal cells in the testicular parenchyma secreting alpha fetoprotein. It is the most common testicular tumour in children aged less than 3 years, but rarely can occur in adults.
Case presentation
-
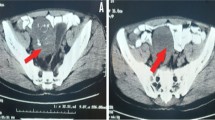
CASE 1: (Fig. 2)
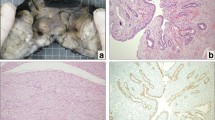
A Ultrasound of the abdomen at the level of the pelvis shows a tubular rudimentary uterus measuring 6 × 1.5 cm (curved arrow) seen adjacent to a large pelvic mass (star). B, C Contrast enhanced abdomen in reformatted coronal (B) and sagittal view (C) at the level of the pelvis shows a large lobulated heterogeneously enhancing mass lesion (star) in the postero superior aspect of the bladder (arrow head) and the rudimentary uterus (right arrow). D, E, F Contrast enhanced abdomen in coronal (D) and axial views (E, F) at the level of the pelvis shows empty scrotal sac (right arrow), prostate gland (star) and the rudimentary uterus (left arrow). G, H Biopsy of pelvic mass lesion from Case1, H and E stained sample showing large endodermal sinus tumour predominantly microcystic with focal solid areas
A 28-year-old male presented clinically with lower abdominal pain and abdominal swelling for the past 6 months. On clinical examination, his vitals were stable and on local examination, there was localised abdominal pain in the pelvis and a palpable mass in the pelvis. The testes were not visualised in the scrotal sac. Baseline blood investigations showed increased levels of lactate dehydrogenase (LDH) and alpha fetoprotein. However, beta human chorionic gonadotropin (Beta-HCG) levels were normal. As a part of radiological investigations, USG Abdomen was performed which showed a rudimentary uterus with a large pelvic mass. The patient was then subjected to a contrast CT abdomen for further evaluation.
CECT (contrast enhanced computed tomography) of Abdomen and pelvis showed an elongated pear shaped structure [6 × 1.5 cm] extending superiorly from the right seminal vesicle towards midline, located posterior to urinary bladder and anterior to rectum with a central fluid filled cavity, lined by enhancing outer layer depicting the rudimentary uterus.
Along with this ,confirming the ultrasound findings, a large well defined heterogeneously enhancing lobulated mass was noted in the pelvis measuring 8.5 × 11.6 × 14 cm [AP × TR × CC] , located posterior to the urinary bladder and anterior to the rectum, sigmoid colon and above the uterus like structure. No evidence of fat/ haemorrhage /calcification was noted within the lesion. With the suspicion of pseudo hermaphroditism, karyotyping was done which showed a genotypically normal male (46 XY).Eventually, biopsy of the mass was performed and sent for histopathology (Fig. 2G and H) which showed an endodermal sinus tumour (EST) (Predominantly cystic with few solid areas) of the undescended testis. This confirms that the patient presented with PMDS which had developed into an endodermal sinus tumour of the testes . Ideally the treatment in PMDS would be orchidopexy and hysterectomy. However, this is a rare case of complicated PMDS who had already developed endodermal sinus tumour of the cryptorchidic testes on arrival to the hospital. He was planned for chemotherapy and debulking laparotomy.
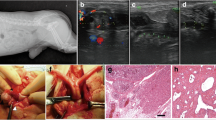
Coronal (A) CT section shows: Right testis is normal in size and position (right arrow). A relatively well defined heterogenous soft tissue density structure of size 3 × 2 cm is noted in the peritoneal cavity (left arrow), in the infraumbilical region, to the left of midline, superior to the urinary bladder. Multiple calcific foci were noted within—The soft tissue density structure most probably represents the left atrophic undescended testis. Large complex cystic lesion (star) with multiple focal enhancing soft tissue densities arising from the left undescended testis-s/o malignant etiology. B, C Axial contrast enhanced CT sections show a large well defined cystic lesion of size 8.5 × 7.4 cm is noted arising from the undescended testis. Multiple focal enhancing soft tissue densities noted in the inner aspect of the cyst wall. Multiple calcific specks noted in the posterior aspect of cyst wall. This is suggestive of malignancy
D, E Seminal vesicles appear bulky (3D) (right arrow), however prostate gland appears normal (E) (left arrow). F, G Contrast enhanced CT sections axial (F) and sagittal (G) views show: An elongated ovoid cystic structure with thick enhancing walls (right arrow) in the superior aspect is seen in the pelvis, posterior to the bladder, deviated to the right. The enhancing superior part could represent the uterine remnant and the thin walled lower part (left arrow) could represent the cervix/upper part of vagina. Urinary bladder (arrow head). Cystic lesion as described in previous (Fig. 3B and C) (star)
A 25 year old male presented to the outpatient department with complaints of lower abdominal pain and burning micturition. On clinical examination, his vitals were stable and left testis was noted not to be present within the scrotal sac. USG (ultrasonogram) abdomen was advised and findings revealed a heteroechoic lesion in the left iliac fossa—? Left testis. In order to confirm the findings, computed tomography (CT) urogram as advised and the findings were astonishing.
The left testis was not visualized within the scrotal sac. Instead, a relatively well defined heterogenous soft tissue density structure of size 3 × 2 cm was noted in the peritoneal cavity, in the infra umbilical region, to the left of midline, posterior to the left rectus muscle and anterior to bowel loops and abutting urinary bladder superiorly. Multiple calcific foci were noted within. This structure was seen to be supplied by the left gonadal artery leaving us with a high suspicion that the soft tissue density structure could most likely probably represent the left atrophic undescended testis.
Adding to this, a large well defined cystic lesion of size 8.5 × 7.4 cm was noted arising from the undescended testis. Multiple focal enhancing soft tissue densities were noted in the inner aspect of the cyst wall and multiple calcific specks were noted in the posterior aspect of cyst wall. This suggested the possibility of malignancy.
What surprised us was an unexpected elongated ovoid cystic structure with thick enhancing walls in the superior aspect that was seen in the pelvis, posterior to the bladder, deviated to the right. The enhancing superior part seemed to represent the uterine remnant and the thin walled lower part the cervix/upper part of vagina that was seen to abut the seminal vesicles inferiorly.
From the supero lateral corners of the uterine remnant, two tubular structures were seen running towards the deep inguinal ring. The right tubular structure was seen to course through the right inguinal canal-probably representing the round ligament/fallopian tubes/ductus deferens and the left tubular structure was seen to end blindly at the left superficial inguinal ring- probably representing the round ligament/fallopian tubes.
However, the right testis was normal in size and position.
Karyotyping was performed which showed a genotypically normal male (46 XY).He was advised biopsy of the lesion arising from the undescended left testis.
Unfortunately, this patient could not be followed up, he did not come back to our hospital but these findings were worth mentioning.
Discussion
So, what is PMDS? An unconventional form of internal pseudohermaphroditism in a genetically and normally virilized male depicted by the presence of Mullerian duct derivatives such as the uterus, fallopian tubes, cervix, vagina is known as PMDS. In other words, this is a rare variety of DSD. Clinically these patients present with normal external genitalia, however have ambiguous genitalia/secondary sexual characteristics [1].
Looking into genetics of PMDS, it is usually inherited in an autosomal recessive manner. Around 85% of the patients have mutation of the MIS gene on chromosome 19p13 or MISR-II gene on chromosome 12q13, while the cause is unknown in 15% of them [2].The main etiology underlying this disorder is the lack of Mullerian inhibiting substance (MIS)/ AMH in the body [3].It is caused either due to a lack in production of Anti Mullerian Hormone[AMH] from immature sertoli cells in newly developed testis (PMDS type I) or resistance to AMH receptor (AMHR2 gene), (PMDS type II) [4].
In the embryogenesis period, that is during early development, the embryonal reproductive tract in either sex consists of both the Mullerian duct and Wolffian ducts. In a male fetus at the 8th week of gestation, testosterone and Mullerian Inhibiting Substance (MIS) are produced from leydig cells and sertoli cells from the recently formed testes. This testosterone helps in differentiation of the Wolffian duct into various structures like epididymis, seminal vesicles and vas deferens. On the other hand, MIS, commonly known as AMH is a glycoprotein homodimer which plays an important role in testicular descent as well in Mullerian duct regression. On the contrary, in females this testosterone absence causes degeneration of the Wolffian duct. With the lack of MIS, Mullerian duct differentiation into female reproductive organs like uterus, fallopian tubes and ovaries occurs [5,6,7].
How can we classify types of PMDS? PMDS can be broadly divided into two types (Fig. 5), a male form and a female form based on anatomical structure. Male form being the more common one (80–90% of cases), is characterized clinically by unilateral cryptorchidism and contralateral inguinal hernia with usually the ipsilateral testis as its content. In case the uterus was also dragged along with it, it would be known as hernia uteri inguinalis. Another variant of this male form is when both the testes are spotted inside the same hernial sac along with the uterus and fallopian tubes, it is known as transverse testicular ectopia which accounts for ~ 10% of the cases. Female form is characterized by bilateral cryptorchidism and uterus fixed to the pelvis with bilateral testes attached to the round ligaments on either side in ovarian positions. Inguinal hernia is not seen in this type. On a side note, mobility of the Mullerian duct derivatives plays an important role, as presence of mobility causes the uterus and fallopian tube to be drawn into the inguinal canal and absence of mobility may block testicular descent [8].
A Female form is characterized by bilateral cryptorchid testes and uterus fixed to the pelvis with bilateral testes attached to the round ligaments on either side. B Male form is characterized by unilateral cryptorchid testis and contralateral inguinal hernia with testis and fallopian tube of the contralateral side in the sac. C Transverse testicular ectopia in which two testes are visualized in the same hernia sac along with the uterus and uterine tubes
In the respective cases discussed above in our article, Case 1 was female form and Case 2 was male form.
How important is the role of radiological scans in recognizing patients with PMDS? Diagnosis of this uncommon entity is usually incidental, as structures derived from Mullerian duct are routinely undetectable in abdominal or scrotal examination, hence radiological investigations like USG, CT, and magnetic resonance imaging (MRI) play an important role in identifying this clinical condition. Patients who present with bilateral undescended testis or unilateral inguinal hernia accompanied by a contralateral cryptorchid testis or unilateral inguinal hernia along with a palpable mass above the normally descended testis must undergo USG, CT or MRI and chromosomal analysis suspecting the presence of Mullerian duct structures. In our case, the first patient had already developed an endodermal sinus tumor. Hence chemotherapy and debulking laparotomy were performed on this patient. In patients with PMDS the risk of malignant transformation into germ cell tumours such as gonadoblastoma is high of 15–40% according to the available current literature [9], hence immediate surgical removal of these structures and the undescended testis (orchidopexy) should be performed to eliminate the risk [10].On the other hand, there is a patient to patient variation regarding fertility in PMDS patients. Even though infertility seems to be a complication in PMDS patients, according to a study by Josso et al. [11], fertility is preserved if the gonads descend into the scrotum.
Looking at the importance of lab value parameters, determination of AMH levels in the serum using a specific test like ELISA can be used as a screening tool in the approach and confirmation of the diagnosis. In patients with PMDS, sexual function is routinely normal, but fertility is a bit compromised, even in treated patients. Discussing further about Case 1 in our article, after using karyotyping and histopathological reports to confirm PMDS, in this patient, EST was observed. The characteristic increase in Alpha feto protein was observed as these are secreted from the malignant endodermal cells. Along with this, Schiller duval bodies were confirmatory of EST in pathological slides. LDH which is expressed on chromosome 12p, linked to the testes as mentioned above, increases in testicular malignancies, hence the spike in our Case1.
A common differential to cryptorchidism in these patients is anorchia, for which AMH serum assay is recommended, however, only this test is not entirely specific in patients with AMH mutations, hence in such cases testosterone assay and thorough ultrasound examination will help in diagnosis. Mixed gonadal dysgenesis is another common differential, where biopsy is necessary to confirm the sex and rule this out. Diagnosing PMDS is challenging as it is complex and anatomically variable.
Management of PMDS includes removal of the Mullerian duct structures as they could hypertrophy and accumulate blood causing pain and discomfort to the patient. They obstruct the prostatic utricle causing recurrent urinary tract infection, stones and voiding disturbances. Removal also reduces the risk of malignancy in these patients from the MDS structures. Subtotal hysterectomies (in order to avoid hormonal problems) and salpingectomies are performed.
Regarding the Wolffian duct structures, orchidopexy to place the testes in the scrotal sac is the main treatment of choice along with preservation of vas to maintain fertility. In case streak gonads are present, or of the testes aren’t mobile, then orchidectomy is treatment of choice. In our patient (Case 1), malignant transformation of the testes was noted, hence we proceeded with debulking laparotomy and chemotherapy.
Conclusion
PMDS is a rare entity in clinical practice with very few cases reported in medical literature. Radiological imaging plays a significant role in establishing the diagnosis which is further confirmed by karyotyping, histopathological and Immunohistochemistry results. Overall, surgery is performed in PMDS in order to prevent infertility or cancer. This motivation behind this article is to bring such rarely reported cases into the light and enlighten clinicians and radiologists for a broader thinking perspective and better diagnosis. Diagnosis could often be arduous due to unfamiliarity with the condition.
Availability of data and materials
Using medsynapse software from our Sri Ramachandra Medical College, Porur, Chennai, India database.
Abbreviations
- PMDS:
-
Persistent Mullerian duct syndrome
- MIS:
-
Mullerian inhibiting substance
- AMH:
-
Anti Mullerian hormone
- DSD:
-
Disorders of sex development
- CECT:
-
Contrast enhanced computed tomography
- Beta:
-
HCG: beta human chorionic gonadotropin
- USG:
-
Ultrasonogram
- CT:
-
Computed tomography
- MISR:
-
Mullerian inhibiting substance receptor
- AMHR:
-
Anti Mullerian hormone receptor
- MRI:
-
Magnetic resonance imaging
- ELISA:
-
Enzyme linked immuno sorbent assay
- EST:
-
Endodermal sinus tumour
- LDH:
-
Lactate dehydrogenase
- MDS:
-
Mullerian duct syndrome
References
Renu D, Rao BG, Ranganath K, Namitha (2010) Persistent Mullerian duct syndrome. Indian J Radiol Imaging 20(1):72–74
Agrawal AS, Kataria R (2015) Persistent Müllerian Duct Syndrome (PMDS): a rare anomaly the general surgeon must know about. Indian J Surg 77(3):217–221
Alharbi KN, Khushaim AO, Alrasheed M, Akhtar M, Neimatallah M (2017) Radiological findings in persistent Müllerian duct syndrome: case report and review of literature. J Radiol Case Rep 11(3):7–14
Picard JY, Cate RL, Racine C, Josso N (2017) The persistent Müllerian duct syndrome: an update based upon a personal experience of 157 cases. Sex Dev 11(3):109–125
Wongprasert H, Somanunt S, De Filippo R, Picard JY, Pitukcheewanont P (2013) A novel mutation of anti-Mullerian hormone gene in Persistent Mullerian Duct Syndrome presented with bilateral cryptorchidism: a case report. J Pediatr Urol 9(4):e147–e149
Hannema SE, Hughes IA (2007) Regulation of Wolffian duct development. Horm Res 67(3):142–151
Nayak VJ, Kamath AS, Krishnappa MH, Bylappa SK (2014) Persistent Mullerian duct syndrome: a case report and review of the literature. Int J Appl Basic Med Res 4(2):125–127
Ferguson L, Agoulnik AI (2013) Testicular cancer and cryptorchidism. Front Endocrinol (Lausanne) 4:32
Cools M, Drop S, Wolffenbuttel K, Oosterhuis J, Looijenga L (2006) Germ cell tumors in the intersex gonad: old paths, new directions, moving frontiers. Endocr Rev 27(5):468–484
Vandersteen DR, Chaumeton AK, Ireland K, Tank ES (1997) Surgical management of persistent Müllerian duct syndrome. Urology 49(6):941–945
Josso N, Belville C, di Clemente N, Picard JY (2005) AMH and AMH receptor defects in persistent Müllerian duct syndrome. Hum Reprod Update 11(4):351–356
Acknowledgements
Dr. K. Jeyakumar, Dr. R. Dhanalakshmi (both of them have been very patient with me, had emotionally and mentally supported me while drafting this article and I would like to acknowledge them for this reason).
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
RR1—RR; RR2—RR; AJ conceptualized, curated the data regarding this patient, went through the methodology, investigated the patient and the data, wrote the original draft, and edited it. RR1 conceptualized, curated the data regarding this patient, performed a formal analysis, supervised and validated the final manuscript. RR2 investigated the patient and the data, supervised and validated the final manuscript. LJ curated the data regarding this patient, investigated the patient and the data, reviewed and edited the original draft. VG curated the data regarding this patient, reviewed and edited the original draft. All authors read and approved the final manuscript. All the authors have agreed to be personally accountable for the author's own contributions.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable, consent to participate has been obtained from participant.
Consent for publication
Consent obtained from participant.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jeyakumar, A., Ramachandran, R., Rangasami, R. et al. Reviewing recherche presentations of persistent Mullerian duct syndrome: case reports. Egypt J Radiol Nucl Med 53, 73 (2022). https://doi.org/10.1186/s43055-022-00752-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-022-00752-w