Abstract
Background
Chronic obstructive pulmonary disease [COPD] is a very common disease in developing as well as in developed countries. Using CT has a growing interest to give a phenotypic classification helping the clinical characterization of COPD patients. So, the aim of the present study was to evaluate whether there was a significant correlation between quantitative computed tomography lung analysis and pulmonary function tests in chronic obstructive pulmonary disease patients.
Results
The study included 50 male patients with a mean age of 62.82 years ± 8.65 years standard deviation [SD]. Significant correlation was found between the pulmonary function tests [FEV1 and FEV1/FVC ratio], and all parameters of quantitative assessment with – 950 HU [the percentage of low-attenuation areas (% LAA)]. Pulmonary function tests according to GOLD [Global Initiative for Chronic Obstructive Lung Disease] guidelines revealed that 4% had normal pulmonary function, 8% had mild obstructive defect, 32% had moderate obstructive defect, 26% had severe obstructive defect, and 30% had very severe obstructive defect.
Conclusion
Automated CT densitometry defining the emphysema severity was significantly correlated with the parameters of pulmonary function tests and providing an alternative, quick, simple, non-invasive study for evaluation of emphysema severity. Its main importance was the determination of the extent and distribution of affected emphysematous parts of the lungs especially for selecting the patients suitable for the lung volume reduction surgery.
Similar content being viewed by others
Background
Chronic obstructive pulmonary disease [COPD] is a very common disease in developing as well as developed countries. This is due to several factors: among them, the different smoking habits, air pollution, and occupational exposure. However, it is a heterogeneous disease, and pulmonary function tests alone could not explain the disease heterogeneity [1].
The chronic obstructive pulmonary disease (COPD) includes two phenotypically related diseases: emphysema and chronic bronchitis [2]. The main pathological changes in COPD patients include inflammation and deficient gas exchange. Emphysema is considered parenchymal-predominant pathology, which is characterized by abnormal over-distension of the alveoli and irreversible destruction of the supporting structures. These changes lead to almost permanent damage to gaseous exchange [3]. Chronic bronchitis is an airway-predominant disease [4]. The emphysematous phenotype is mainly associated with severe form of the disease [5]. It is important to define whether the pathological changes are airway-predominant or parenchymal-predominant pathology. This will affect the management plane by applying specific therapies to prevent airway remodeling or parenchymal destruction [6].
Pulmonary function tests can be used to assess the severity of COPD. COPD cases with FEV1/FVC less than 70% revealed respiratory dysfunction [7]. However, PFTs have several limitations including inability of some patients to do such tests due to their poor clinical condition, weakness, or associated disorders affects tests results [8, 9].
The marked disease heterogeneity hinders the clinical classification, where the available clinical staging systems could not allow enough information for prognosis and adequate follow-up. Thus, using CT has a growing interest to give a phenotypic classification helping the clinical characterization of COPD patients [1].
Han et al. suggested that CT could discriminate between patients with the same results of spirometry [10]. CT is widely used, not only for the assessment of anatomical and structural elements of the chest but also for the assessment of functional parameters including lung density and volume. Especially, with the recent MDCT technology, faster volumetric data can be easily obtained and used for volume evaluation [11]. Until now, the volumetric CT emphysema quantification is not part of the routine CT study of the chest in COPD patients. The visual evaluation methods are highly subjective depending on the radiologist and his level of experience [1].
CT quantification evaluates the emphysema severity and provides a simple way to classify COPD subjects to subgroups characterized by predominant emphysema, mixed emphysema and air trapping, and predominant air trapping [12].
Furthermore, it provides local information essentially needed for planning of surgical interventional or systemic treatment for COPD patients [13]. It has been reported that CT quantification of emphysema may predict COPD severity [14]. CT provides densitometric measurements that are highly reproducible and have been correlated with macroscopic measurements of emphysema [15, 16].
The emphysema extent is generally assessed by using parameters of CT densitometry such as the relative lung area with attenuation coefficients below a predefined threshold. Another method is percentile of the frequency-attenuation distribution using the nth cut-off percentile in the attenuation distribution curve, which provides the density value in Hounsfield units [HU] under which n% of the voxels is distributed [17, 18]. Quantitative emphysema evaluation will be a main feature for serial follow-up of COPD patients [19].
The aim of this study was to determine whether there was a significant correlation between quantitative CT lung analysis and pulmonary function in chronic obstructive pulmonary disease patients.
Methods
Patient population
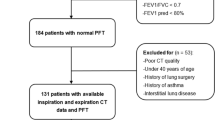
This prospective study was conducted at radio-diagnosis and chest departments of university hospital during the period between March 2016 and April 2017 and included 50 male patients with considered clinical diagnosis of COPD. All patients were over the age of 40 with 2 or more of the following: dyspnea, chronic cough, chronic sputum production, recurrent lower respiratory tract infection, history of risk factors, e.g., Tobacco smoke, occupational dusts, and chemicals, and family history of COPD. Prior to the investigation, all patients gave a written consent after full explanation of the procedure. After excluding bronchial asthma, bronchiectasis, interstitial pulmonary fibrosis patients were subjected to the following tests.
Pulmonary function tests [PFTs]
FEV1, FVC, and FEV1/FVC ratio were done using Master screen spirometry. Pulmonary function tests expressed as percentages of the predicted values based on age, sex, height, and weight. They were completed within 1 week before or after MDCT scanning. COPD subjects were staged according to GOLD guidelines [20]. In patients with FEV1/FVC < 0.70:
-
GOLD 1: Mild FEV1 ≥ 80% predicted
-
GOLD 2: Moderate 50% ≤ FEV1 < 80% predicted
-
GOLD 3: Severe 30% ≤ FEV1 < 50% predicted
-
GOLD 4: Very severe FEV1 < 30% predicted
Computed tomography
High-resolution MDCT acquisition parameters
HRCT techniques were done using Toshiba MSCT 16 channels. No I.V contrast was given. Scans were obtained during full inspiration in supine position, with the following parameters: 120–140 kv, 120–160 mAs, 5 mm collimation, and a pitch of 1.5/1 with a standard reconstruction algorithm. Scan volumes were extended craniocaudally from the thoracic inlet to the level of the diaphragm and were acquired in one breath-hold period.
Quantitative lung analysis
Special lung analysis CT algorithm was used for quantitative assessment by using machine-based lung analysis software. Acquired images were sent to Vitrea workstation, VITAL IMAGES, MN, USA, in Toshiba office; Heliopolis, Cairo, using Lung Density Software ;Version 6.7 to be processed, manipulated, and reconstructed. Selecting lung density analysis preset, the lungs were automatically segmented from chest wall, mediastinum, airways, and vessels. The software automatically analyzed the density distribution of the lungs. Attenuation in the lung was expressed in Hounsfield units (HU). The 15th percentile density (PD15), i.e., the HU value below which 15% of the lung attenuation values, were distributed. The density mask technique was applied by using threshold cut-off value of – 950 HU. This level was chosen because it correlated best to the emphysematous changes in the lungs by Wang et al. [21]. The percentage of the lung volume with attenuation below the cut-off value – 950 HU (RA-950) were calculated for the entire lungs (right, left, and both lungs), as well as separately for the upper (right, left, and both) and lower lobes (right, left, and both) of the lungs as well as PD15 for the entire lungs using the volumetric scan. Data were expressed in the form of tables and histograms [Figs. 1 and 2].
Male patient 65 years old, chronic heavy smoker. Pulmonary function tests showed very severe obstructive pulmonary disease. a–d HRCT (axial, sagittal, and coronal images) revealed hyperinflated chest, mild bilateral diffuse emphysematous changes predominately the right upper lobe. e–g Images after applying density mask revealed emphysematous areas as black areas while normal lung density as gray. More pronounced bilateral diffuse emphysematous changes, more evident at the right upper lobe (Right upper lobe low density index 48.4%) and to a lesser degree, left upper lobe (left upper lobe low density index 33.1%). h, i Lung density histogram showing distribution of voxel density with respect to the whole lung volume: x-axis represents density range expressed in HU, whereas y-axis scales the relative number of voxels as a percentage of total lung volume. Evaluation of the histogram allowed quantification mean lung density (MLD), 15% percentile value (P15), and relative volume of parenchyma with density lower than – 950 HU. LAV, low attenuation volume. PD15% for right lung is 59, left lung 74, and both lungs 66. N.B: both upper lobes more emphysematous than both lower lobes as regarding the low-density index that of both upper lobes was 41.2%while that of both lower lobes was 25.7%
Male patient, 45 years old, chronic heavy smoker. a–c HRCT images with subtle bilateral diffuse emphysematous changes. d–f After applying density mask, image segmentation. g Lung density histogram. Although pulmonary function tests were normal, there were bilateral emphysematous changes with both lower lobes more emphysematous than both upper lobes as regarding the low-density index that of both lower lobes was 18.2%while that of both upper lobes was 15.7%, and the left lung is more emphysematous than the right lung. Findings revealed more pronounced bilateral diffuse emphysematous changes, more pronounced at the left lower lobe (left lower lobe low-density index 19.9%), and to a lesser degree left upper lobe(left upper lobe low-density index 18.5%)
Statistical analysis
Statistical analysis was done. The results presented as mean ± SD for patient characteristics, quantitative CT parameters, and pulmonary function parameters. Pearson’s correlation was done between data of pulmonary function tests and quantitative CT parameters. A value of p < 0.05 was considered statistically significant. Multiple comparisons (post hoc test) were done between groups following ANOVA test in order to determine which groups differ from each other. The mean difference was significant at the 0.05 level.
Results
Demographic and clinical characteristics
Fifty males presenting with chronic obstructive lung disease were included in the study. Their ages ranged from 45 to 79 years with a mean age of 62.82 years ± 8.65 years. All patients in this study had positive smoking history.
Pulmonary function tests
Pulmonary function tests revealed that 2(4%) had normal pulmonary function, and obstructive defects were found to be mild 4(8%), moderate 16(32%), severe 13 (26%), and very severe 15(30%).
Correlation of quantitative CT parameters of emphysema with pulmonary function tests
Pearson’s correlation test revealed that there was highly significant negative correlation between FEV1/FVC ratio and all right, left, and both upper and lower lung density parameters (p < 0.01 and r ≥ 0.4). Also, there was significant negative correlation between FEV1 and all right, left, and both lungs as well as right lower density parameters (p < 0.05 and r < 0.4) except for that of right, left and both upper, left and both lower lung density index being highly significant negative correlation (p < 0.01 and r ≥ 0.4). While FVC was not significantly correlated with all right, left, and both upper and lower lung density parameters except for that of right, left, and both upper lung density index being significant negative correlation (p < 0.05 and r < 0.4) (Table 1).
On the other hand, there was highly significant positive correlation between pulmonary function tests (FEV1, FEV1/FVC ratio) and right, left, and both lungs PD15% (p < 0.01 and r ≥ 0.4) while FVC showed significant positive correlation with left lung PD15% only (p < 0.05 and r < 0.4).
Difference between groups
For multiple statistical comparisons between different study groups using post hoc test (
Table 2). The mean difference was significant at the 0.05 level. Table 2 revealed statistical significant difference between very severe grade and other grades of emphysema regarding (Rt.U.LDI.percent, RT. PD15.percent, Lt.LLDI.percent, Lt.U.LDI.percent, and bothU.LDIpercent).
Discussion
COPD is a common heterogenous disease in which spirometric results are not sufficient to explain these heterogeneities. Han et al. [10] reported that CT could be a valuable modality to differentiate between patients of COPD especially those with the same spirometric results. Temizoz et al. [11] found that MDCT and measurement of CT pixel attenuation values were good methods for quantifying emphysema. Bakker et al. [22] also reported the importance of quantitative CT measurement in assessment of degree and distribution of emphysema.
Muller et al. were the first to describe and verify pathologically the density mask technique, in which CT pixels with attenuation below a certain threshold value [initially – 910 HU] were identified as emphysema [23]. Madani et al. [24] revealed that the most appropriate HU to be used in the density mask method is − 960 or – 970 HU.
The threshold value – 950 HU showed the best correlation to demonstrate degree of emphysema [25]. Gevenois et al. reported that the strongest pathologic correlation with emphysema at macroscopic and microscopic level had been established at a threshold of [− 950 HU] in a 1-mm non-contrast enhanced high-resolution CT images [26]. According to the study done by Wang et al., the threshold of − 950 HU is optimal for CT densitometry analysis of emphysema when the CT examinations are obtained at full inspiration [21]. In the current study, the density mask method was applied to the entire lung as well as to each individual lobe, and we used [− 950 HU] as % LAA for quantifying emphysema.
In the present study, the CT examination was done without the use of intravenous contrast material administration because non-enhanced volumetric CT study is a standard technique for COPD imaging as intravenous contrast material affects the attenuation values of the imaged organs [18]. In our study, all examinations were acquired in full inspiration. No expiratory CT examination was performed; it is consistent with Gevenois et al. who showed that expiratory quantitative CT is not as precise as inspiratory CT in measuring lung emphysema. Moreover, the patients having difficulty breathing can tolerate inspiratory CT more than expiratory CT [26].
Pulmonary function tests (PFT) parameters although, commonly used in assessment and classification of COPD cases, could not detect the heterogeneous changes of the disease process or the early abnormalities [12]. In the present study, two cases with normal PFT showed decreased mean lung density [MLD] which was correlated with their clinical signs.
In the present study, we found significant relationship between the pulmonary function tests (FEV1 and FEV1/FVC ratio), and all parameters of quantitative assessment with – 950 HU (%LAA) agreed with different studies [21, 24]. Highly significant negative correlation was detected between FEV1/FVC ratio, and all lung density parameters (p < 0.01 and r ≥ 0.4) also, between FEV1 and right, left, and both upper, left, and both lower lung density index (p < 0.01 and r ≥ 0.4). There was significant negative correlation between FEV1 and all lung density parameters (p < 0.05 and r < 0.4). While FVC was not significantly correlated with all lung density parameters except for that of right, left, and both upper lung density index being significant negative correlation (p < 0.05 and r < 0.4).
When studying the correlation between emphysema extent and pulmonary function, Saitoh et al. found a strong correlation when the upper lobes are predominantly affected, Matsuo et al. showed that a strong correlation between predominant lower lobes involvement and FVC, FEV1 [27, 28]. However, in the current study, we could not observe obvious difference in correlation coefficients between the upper lobes and the lower lobes. Nevertheless, we observed that the mean LAA% values of the right and left upper lungs were slightly higher than those of the right and left lower lung lobes.
The CT lung analysis adds extra information for diagnosis particularly in debatable circumstances [3]. The use of quantitative MDCT analysis provides more accurate estimates of the COPD severity and disease distribution [29]. An alternative method to quantification of emphysema, based on the frequency histogram of lung attenuation, estimates the CT attenuation at a given percentile along the histogram. The 15th percentile threshold is used to assess the variations of emphysema cases rather than changes in the lung volume [13, 30]. It was evident that the percentile method is more powerful for follow-up of emphysema [22].
In our study, we found that there was highly significant positive correlation between pulmonary function tests (FEV1, FEV1/FVC ratio) and right, left and both lungs PD15% (p < 0.01 and r ≥ 0.4) while FVC showed significant positive correlation with left lung PD15% only (p < 0.05 and r < 0.4).
The lung density analysis is superior to expiratory CT methods because it provides information about the whole lung. In addition, it appears that lung density analysis will allow for new horizons in providing information about lung parenchyma, lung density and density distribution, and additionally, the subthreshold values’ percentage in emphysematous patients. Yet, lung density analysis has its own limitations: one of them is that its effectiveness is based on co-operation of the patient. For example, incomplete inspiration results in minimal decrease in lung density and misinterpretation [3].
Conclusion
Automated CT densitometry defining the emphysema severity was significantly correlated with the parameters of pulmonary function tests and providing an alternative dependable quick, simple non-invasive study for evaluation of emphysema severity. Its main importance was the determination of the extent and distribution of affected emphysematous parts of the lungs especially for selecting the patients suitable for the lung volume reduction surgery.
We recommended that CT quantification of emphysema to be a part of the routine chest CT study in COPD patients.
Availability of data and materials
All data are available at the corresponding author who has the authority to respond if there is any query.
Abbreviations
- FVC:
-
Forced vital capacity
- FEV1/FVC:
-
The ratio of forced expiratory volume in 1 second over forced vital capacity
- HU:
-
Hounsfield units
- GOLD:
-
Global Initiative for Chronic Obstructive Lung Disease
- MDCT:
-
Multi-detector computed tomography
- COPD:
-
Chronic obstructive pulmonary disease
- PFTs:
-
Pulmonary function tests
References
Mohsen LA, Gawad EA, Ibrahiem MA (2014) CT quantification of emphysema: is semi-quantitative scoring a reliable enough method? Egypt J Radiol Nucl Med 45:673–678
Global Initiative for Chronic Obstructive Lung Disease: Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease (Updated 2016). Available at: http://www.goldcopd.org/guidelines-global-strategy-for-diagnosis-management.html (accessed January 2016).
Nhue LD and Beek YC: Chronic obstructive pulmonary disease: emphysema revisited, chronic obstructive pulmonary disease - Current Concepts and Practice, Dr. Kian-Chung Ong (Ed.), ISBN: 978-953-51-0163-5, InTech, Available from:http://www.intechopen.com/books/chronic.obstructive-pulmonary-disease-current-concepts-and-practice/chronic-obstructive-pulmonary-disease-emphysema-revisited (2012).
Patel B, Make B, Coxson HO et al (2006) Airway and parenchymal disease in chronic obstructive pulmonary disease are distinct phenotypes. Proc Am Thorac Soc 3:533
Boschetto P, Quintavalle S Zeni E et al. (2006),: Association between markers of emphysema and more severe chronic obstructive pulmonary disease. Thorax 61:1037–1042
Grenier PA (2005) Detection of altered lung physiology. Eur Radiol 15:42–47
Vogelmeier CF, Criner GJ, Martinez FJ, Anzueto A, Barnes PJ, Bourbeau J et al (2017) Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 report. GOLD executive summary. Am J Respir Crit Care Med 195:557–582
Topalovic M, Laval S, Aerts JM, Troosters T, Decramer M, Janssens W (2017) Automated interpretation of pulmonary function tests in adults with respiratory complaints. Respiration 93:170–178
Al-Ashkar F, Mehra R, Mazzone PJ. Interpreting pulmonary function tests: recognize the pattern, and the diagnosis will follow. Cleve Clin J Med 2003;70:866, 868, 871-873, passim
Han MK, Agusti A, Calverley PM, Celli BR, Criner G, Curtis JL et al (2010) Chronic obstructive pulmonary disease phenotypes: the future of COPD. Am J Respir Crit Care Med 182:598–604
Temizoz O, Etlik O, Emin M, Uzun K, Arslan H, Harman M et al (2007) Detection and quantification of the parenchymal abnormalities in emphysema using pulmo-CT. Comput Med Imag Grap 31:542–548
Schroeder JD, McKenzie AS, Zach JA, Curran-Everett D, Stinson DS, Newell JD et al (2013) Relationships between airflow obstruction and quantitative CT measurements of emphysema, air trapping and airways in subjects with and without COPD. AJR Am J Roentgenol 201:460–470
Heussel CP, Herth FJ, Kappes J, Hantusch R, Hartlieb S, Weinheimer O et al (2009) Fully automatic quantitative assessment of emphysema in computed tomography: comparison with pulmonary function testing and normal values. Eur Radiol 19:2391–2402
Desai SR, Hansell DM, Walker A, MacDonald SL, Chabat F, Wells AU (2007) Quantification of emphysema: a composite physiologic index derived from CT estimation of disease extent. Eur Radiol 17:911–918
Ley-Zaporozhan J, Ley S, Weinheimer O, Iliyushenko S, Erdugan S, Eberhardt R et al (2008) Quantitative analysis of emphysema in 3D using MDCT: influence of different reconstruction algorithms. Eur J Radiol 65:228–234
Akira M, Toyokawa K, Inoue Y, Arai T (2009) Quantitative CT in chronic obstructive pulmonary disease: inspiratory and expiratory assessment. AJR 192:267–272
Matsuoka S, Yamashiro T, Washko GR, Kurihara Y, NakajimaY, Hatabu H (2010) Quantitative CT assessment of chronic obstructive pulmonary disease. RadioGraphics 30:55–66
Mets OM, de Jong PA, van Ginneken B, Gietema HA and Lammers JW. Quantitative computed tomography in COPD: possibilities and limitations. Lung .2012; 190: 133 –145.
Atta H, Seifeldein GS, Rashad A, Elmorshidy R (2015) Quantitative validation of the severity of emphysema by multi-detector CT. Egypt J Radiol Nucl Med 46:355–361
Global Initiative for Chronic Obstructive Lung Disease: Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease, http://www.goldcopd.org/guidelines-global-strategy-for-diagnosis-management.html/; 2018 [accessed January 2018].
Wang Z, Suicheng G, Leader JK, Kundu S, Tedrow JR, Sciurba FC et al (2013) Optimal threshold in CT quantification of emphysema. Eur Radiol 23:975–984
Bakker ME, Stolk J, Putter H et al (2005) Variability in densitometric assessment of pulmonary emphysema with computed tomography. Investig Radiol 40:777–783
Muller NL, Staples CA, Miller RR et al (1988) Density mask”an objective method to quantitate emphysema using computed tomography. Chest 94:782–787
Madani A, Zanen J, de Maertelaer V, Gevenois PA (2006) Pulmonary emphysema: objective quantification at multi-detector row CT--comparison with macroscopic and microscopic morphometry. Radiology 238:1036–1043
Lee YK, Oh YM, Lee JH, Kim EK, Lee JH, Kim N et al (2008) Lung 186:157–165
Gevenois PA, De Vuyst P, de Maertelaer V, Zanen J, Jacobovitz D, Cosio MG et al (1996) Comparison of computed density and microscopic morphometry in pulmonary emphysema. Am J Respir Crit Care Med 154:187–192
Saitoh T, Koba H, Shijubo N, Tanaka H, Sugaya F (2000) Lobar distribution of emphysema in computed tomographic densitometric analysis. Investig Radiol 35:235–243
Matsuo K, Iwano S, Okada T, Koike W, Naganawa S (2012) 3DCT lung volumetry using multidetector row computed tomography: pulmonary function of each anatomic lobe. J Thorac Imaging 27:164–170
Galbán CJ, Han MK, Boes JL, Chughtai KA, Meyer CR, Johnson TD et al (2012) Computed tomography-based biomarker provides unique signature for diagnosis of COPD phenotypes and disease progression. Nat Med 18:1711–1715
Dirksen A (2008) Monitoring the progress of emphysema by repeat computed tomography scans with focus on noise reduction. Proc Am Thorac Soc 5:925–928
Acknowledgements
Not applicable.
Ethics approval and consent to participate
The study was approved from the ethical committee of Faculty of Medicine, Beni-Suef University (FWA00015574). Data were collected after obtaining informed written consent of all cases.
Funding
No funding resources.
Author information
Authors and Affiliations
Contributions
SA carried out statistical analysis, drafted and edited the paper. MH contributed to the data collection, shared in image analysis and interpretation. AS shared in design and drafting of the manuscript. MM carried out clinical assessments. All contributing authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Consent for publication
All patients included in this research gave written informed consent to publish the data contained within this study.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Abd elsalam, S.M., Hafez, M., Mohmed, M.F. et al. Correlation between quantitative multi-detector computed tomography lung analysis and pulmonary function tests in chronic obstructive pulmonary disease patients. Egypt J Radiol Nucl Med 51, 160 (2020). https://doi.org/10.1186/s43055-020-00281-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-020-00281-4