Abstract
Background
In critically ill cases, CRRT is a renal replacement intervention. The most common reason why CRRT terminates prematurely (non-electively) is clotting in the extracorporeal circuit, more especially in the filter.
Aim of work
To determine the frequency of thrombotic and hemorrhage complications throughout CRRT, the role of antithrombin III level monitoring, the type of anticoagulation, and the dose and laboratory tests utilized to monitor it.
Method
The study was carried out on 58 children who were undergoing CRRT. The children underwent a comprehensive history-taking, assessment, CRRT prescription parameters and alterations, vascular access data, anticoagulation type, dose, and adjustment, as well as monitoring of antithrombin III levels. Furthermore, any extracorporeal circuit clotting or bleeding was documented.
Results
Of the 58 sessions that were examined, 25 (43.1%) resulted in filter clotting. The indication was cured in 16 cases (27.6%), 8 cases (13.8%) resulted in the patient’s mortality, and 9 cases (15.5%) had life-threatening bleeding. The remaining 33 cases (56.9%) were not terminated with filter clotting. Forty-one (70.7%) of studied sessions used unfractionated heparin as anticoagulation, 22.4% used heparin-protamine, 5.2% was not anticoagulated, and one circuit (1.7%) was anticoagulated using regional citrate.
Filter clotting incidence was significantly related to activated partial thromboplastin time (a PTT) value at the end of sessions (P value = 0.000), and platelets count after 4 h of session initiation (P value = 0.048). Antithrombin III levels pre-heparin infusion less than 80 were found in patients who received higher doses of a heparin bolus dose, median dose 35 (IQR 20–35), this relation is statistically significant (P value = 0.042).
Conclusion
In the 58 cases that were examined, the incidence of bleeding was 32.8%; however, 19% of the cases were not severe. The incidence of filter clotting was 43.1% in the study group. a PTT value at the end of sessions, and platelets count after 4 h could be predictors of thrombotic complications during CRRT, antithrombin III deficiency before sessions is a predictor of filter clotting.
Similar content being viewed by others
Background
CRRT is a renal replacement intervention that is designed to preserve the physiologic plasma constituents and volume in critically ill patients. Medication administration is disrupted by extracorporeal circuit failures [1].
Clotting in the extracorporeal circuit, particularly the filter, is the primary cause of premature (non-elective) termination of CRRT. Inadequate anticoagulation is the primary cause of short-lived circuits [2].
In addition to anticoagulation, the case’s circumstance involves prothrombotic states and hemodynamics, vascular access, or circuits [3].
The maintenance of circuit patency typically necessitates anticoagulation [4]. A subtle equilibrium between clotting and bleeding is achieved through appropriate anticoagulation. RCA and unfractionated heparin are among the agents employed [4].
Unfractionated heparin is the most frequently employed anticoagulant on a global scale. It enhances antithrombin III, thereby inhibiting factors Xa and IIa. APTT is employed to monitor the anticoagulant impact [4].
RCA is contingent upon the citrate’s administration via the extracorporeal circuit to attach to calcium and avoid thrombosis, in conjunction with a concurrent calcium infusion to the case [2].
Methods
This investigation aimed to validate the incidence of thrombotic complications and bleeding in minors undergoing CRRT, as well as the effectiveness of various anticoagulation approaches and the value of the antithrombin III level monitoring. This observational cross-sectional study encompassed 58 children, aged up to 13 years, who were admitted to the intensive care units of Cairo University Pediatrics Hospital. CRRT was required for the children owing to the progression of AKI in conjunction with acute severe illness, AKI complicating an acute renal disease, acute necessity for renal replacement in a critically ill child with known/previous CKD, or non-renal indications including metabolic disorders and poisoning.
A comprehensive history and examination were conducted on all patients, which included their age, vital data (blood pressure, respiratory rate, heart rate), indications for CRRT, system malfunctions and supports, and conditions linked with thrombotic tendency or bleeding. The prescription and setup of CRRT were documented. Laboratory monitoring, adjustment, type, and dose of anticoagulation were documented. It tracked the antithrombin III levels before and after the heparin infusion throughout the sessions.
The trends of circuit pressures, requirements for blood flow rate and ultrafiltration, filter coagulation, and the management of any bleeding complications. The coagulation status, filter status (clotted or not), and duration and reason for session termination were all documented.
Sample size calculation
Eighty-five patients were included. This takes into consideration the CRRT volume at the hospital, as well as achieving a statistical power of 80% at an alpha error of 0.05 regarding primary outcomes, on the assumption of 30% developing events and the most significant risk factors having a baseline incidence of 15% and an odds ratio of 4.
Statistical analysis
The data was gathered, revised, encoded, and entered into the Statistical Package for Social Science (IBM SPSS) version 23. When parametric, quantitative data was displayed as the mean, standard deviations, and ranges. When the data was non-parametric, the median and interquartile range (IQR) were employed. In addition, qualitative variables were stipulated as proportions and numerical values.
The chi-square test and/or Fisher exact test were employed to compare the qualitative data of the groups when the expected count in any cell was less than 5 [5].
The Mann–Whitney test was implemented for non-parametric distributions, while the independent t-test was implemented to compare two independent groups with quantitative data and parametric distribution [6].
The margin of error accepted was 5%, and the confidence interval was established at 95%.
P value < 0.05: Significant (S).
Results
Unfractionated heparin was the most common anticoagulation used (41, 70.7%), followed by heparin protamine (13, 22.4%) in cases with a high risk of bleeding, where protamine was administered intravenously, 3 cases were not anticoagulated (5.2%), one session used regional citrate anticoagulation (1.7%).
Nineteen cases had FFP transfusion (32.8%), and 39 (67.2%) did not receive plasma (Table 1).
Table 1 shows activity percentages of antithrombin III, normal activity (80–120) was found in 38 (66.7%) of cases before starting heparin, antithrombin deficiency (activity less than 80) was found in 19 cases (33.3%) before heparin start. After 6 h of heparin infusion, 45 (78.9%) had normal activity (80–120), and it was less than 80 in 12 cases (21.1%). The cause of antithrombin III diminished activity was not investigated in this study, whether congenital or acquired, it was just observed and documented. Thrombotic manifestations were not reported, as well as this diminished activity was not attributed to certain diseases (Table 2).
In the 58 cases that were examined, 25 (43.1%) were complicated by filter clotting. Of these, 17 (29.3%) were effectively resolved, and the CRRT’s indication was healed. The remaining 8 (13.8%) were resolved without resolution of the indication.
Sixteen of the remaining 33 unclotted filters resulted in case cure, 9 in life-threatening bleeding, and 8 in inpatient mortality.
Among the 19 cases complicated with bleeding, the majority (14, 73.7%) received unfractionated heparin as anticoagulation, and 4 (21.1%) had used heparin protamine, but this relation was not statistically significant (P value = 0.908), the bleeding incidence was higher when a median dose of heparin was 30, compared to non-bleeders in which median dose was 20.
A statistical significance was found between the incidence of bleeding and FFP transfusion, which was indicated before starting sessions to correct coagulopathy in certain cases (P value = 0.024), 10 (52.6%) of bleeding occurred in sessions in which FFP was transfused, this points to the augmentation of action of heparin and higher risk of bleeding in circuits received FFP, as further inactivation of clotting factors (prothrombin, factor X, factor IX) occurs by heparin, leading to further bleeding.
Table 3 also shows that the highest PTT values at the end were associated with the risk of bleeding, median of 60 (IQR 50–75) seconds in the bleeding group; however, no statistical significance was found (P value = 0.229) (Table 4).
The majority of cases among circuits not complicated with filter clotting used heparin as anticoagulation (23, 69.7%), and less incidence of clotting was found when a higher bolus dose was used (median 27.5 IQR 20–35); however, no statistical significance was found regarding this finding (P value = 0.817, 0.326).
APTT values at the end of sessions and incidence of filter thrombosis were highly significant statistically (P value = 0.000), the more the PTT values the less the risk of clotting, (median a PTT at the end in clotted circuits was 49, and 67 in non-clotted circuits), means that the circuits were properly heparinized.
Platelet sum after 4 h of CRRT initiation and frequency of filter thrombosis showed a statistical significance (P value = 0.048), the more the platelet count after 4 h, the higher the risk of filter clotting. Platelet counts were documented prior to sessions, mild thrombocytopenia (less than 80) was found in 36 cases, moderate thrombocytopenia (40–80) in 17 cases, severe thrombocytopenia less than 40 in 5 cases, platelet drop also was attributed to heparin-induced thrombocytopenia.
Pressure drop and TMP at the end of sessions were statistically significant with the incidence of filter clotting (P values = 0.001 and 0.002 consecutively) (Figs. 1, 2, 3, and 4).
The median duration of sessions was 45 IQR (24–48) in cases with AT III less than 80 and 48 (IQR 24–72) in sessions with normal AT III values. AT III values less than 80 were found in patients who received higher doses of heparin bolus dose, median dose 35(IQR 20–35), this relation is statistically significant (P value = 0.042), the majority of cases (21, 55.3%) terminated without filter clotting, showed normal AT III values, means that AT III deficiency before sessions is a predictor of filter clotting as it interferes with proper heparinization (Table 5).
AT III values less than 80 were found in 15.8% of cases complicated with life-threatening bleeding, 8 cases (42.1%) of AT III values less than 80 terminated with filter clotting, and 6 cases (31.6%) with AT III values less than 80 received FFP. No statistical significance was found regarding these relations (P values > 0.05).
Discussion
The primary focus of larger, high-quality studies has been on optimum anticoagulation. However, CRRT is intricate, and filter life is influenced via a circuit, vascular access, and management factors [7].
Anticoagulation is typically necessary to preserve circuit patency and should be administered at a low dose to prevent hemorrhage difficulties [4].
RCA and unfractionated and low molecular weight heparin are among the agents employed [4].
In 2021, Kang et al. performed a study on 31 cases at high risk of bleeding to examine the efficacy and safety of RCA after CRRT. The cases were categorized into two groups: the RCA group (n = 17) and the no anticoagulation group (NA, n = 14). The study showed that RCA treatment considerably improves the clinical condition of cases at high risk of bleeding after CRRT, while also effectively and safely prolonging the filter life and preventing coagulation incidences.
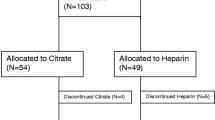
In 2017, Raymakers-Janssen et al. performed a study on infants who received CRRT with the smallest filter in the PICU between November 2011 and November 2016 [8]. Citrate and heparin were administered in accordance with a rigorous protocol. Their primary endpoint was the circuit survival time. The median circuit survival time with heparin was 46.5 h, whereas it was 72 h with citrate (p < 0.001). The median circuit survival time with heparin was 21 h (IQR 14.5–27.5), whereas it was 45.2 h (IQR 37.5–52.8) with citrate (p < 0.001). This statistical significance suggests that the survival time of the circuit is significantly boosted by the use of regional citrate, which should lead to an improvement in the efficiency of CRRT in comparison to heparin.
The present study cannot be linked with this investigation, as only one circuit was anticoagulated with RCA.
In terms of hemorrhage or filter thrombotic complications, this study exhibited no significant difference in the outcome of sessions among the various methods used for anticoagulation (P value = 0.908, 0.817, consecutively). This discovery is in accordance with the clinical guideline established by Zhang et al. [9], which recommends that CRRT be performed without anticoagulation in patients with a contraindication to citrate and an elevated bleeding risk. Nevertheless, the efficacy of CRRT which is not anticoagulated remains inconsistent. The aim of that systematic review was to evaluate the safety and efficacy of CRRT which is free of anticoagulants. The filter’s lifespan and the risk factors for filter failure were the primary outcomes [10].
The anticoagulation-free and systemic heparin groups did not exhibit a significant difference in the filter’s lifespan. The RCA protocol appears to be preferable to the anticoagulation-free protocol (p = 0.53) in terms of filter lifespan (p < 0.001). Nevertheless, the conventional coagulation parameters exhibited subpar predictive performance for filter failure, necessitating the use of anticoagulants prior to CRRT [11, 12].
The optimum anticoagulation approach for seriously ill cases with an elevated bleeding risk may be RCA, provided that it is closely monitored.
The primary outcome of the 2022 study conducted by Zhang et al. was the development and validation of a model to anticipate the adequate filter lifespan in anticoagulation-free CRRT cases (≥ 24 h) [13]. The development cohort consisted of 170 patients. In 80 cases, the filter longevity was adequate. APTT was one of thirteen variables that were independent predictors of sufficient filter lifespan in a logistic regression analysis.
This is in accordance with the results of the current study, which showed a statistically significant link between the value of APTT at the conclusion of a session and filter thrombosis in heparinized circuits (P value = 0.000). Sessions that were not complicated by filter clotting had a median APTT value of 67 s, while the median APTT value until the filter clotting event happened was 49 s. This discovery is also in accordance with the findings of Matthew et al. [4].
Conclusion
The incidence of bleeding was 32.8% among the 58 cases that were studied, although it was not severe in 19%. The incidence of filter clotting was 43.1% in the study group. The heparin bolus dose also influenced antithrombin III levels before CRRT. The majority of cases (21, 55.3%) terminated without filter clotting and exhibited normal AT III values. This suggests that AT III deficiency prior to sessions is a predictor of filter clotting, as it interferes with proper heparinization.
Circuit survival and filter clotting were strongly correlated a PTT values at the end of sessions, and platelet values after 4 h of starting sessions.
Availability of data and materials
Data are available whenever requested.
Abbreviations
- AKI:
-
Acute kidney injury
- APTT:
-
Activated partial thromboplastin time
- CKD:
-
Chronic kidney disease
- CRRT:
-
Continuous renal replacement therapy
- IQR:
-
Interquartile range
- RCA:
-
Regional citrate anticoagulation
- SPSS:
-
Statistical Package of Social Sciences
References
Ayman, Claudio (2020) Anticoagulation in continuous renal replacement therapy. Current opinion in nephrology and hypertension 8(6):701–707
Claure-Del Granado R, Macedo E, Soroko S, Kim Y, Chertow GM, Himmelfarb J, Ikizler TA, Paganini EP, Mehta RL (2014) Anticoagulation, delivered dose and outcomes in CRRT: the program to improve care in acute renal disease (PICARD). Hemodial Int 18(3):641–649
Ronco C, Ricci Z (2015) Pediatric continuous renal replacement: 20 years later. Intensive Care Med 41(6):985–993
Matthew R, Wilson, R (2017) Campbell Tait. In: Handbook of pharmacogenomics and stratified medicine 3:67–102
Chan YH (2003b) Biostatistics 103: Qualitative Data –Tests of Independence. Singapore Med J 44(10):498–503
Chan YH (2003a) Biostatistics102: Quantitative Data – Parametric & Non-parametric Tests. Singapore Med J 44(8):391–396
Brain M, Winson E, Roodenburg O, McNeil J (2017) Non anti-coagulant factors associated with filter life in continuous renal replacement therapy (CRRT): a systematic review and meta-analysis. BMC Nephrol 18(1):69
Raymakers-Janssen PAMA, Lilien M, van Kessel IA, Veldhoen ES, Wösten-van Asperen RM, van Gestel JPJ (2017) Citrate versus heparin anticoagulation in continuous renal replacement therapy in small children. Pediatr Nephrol 32(10):1971–1978
Zhang W, Bai M, Yu Y, Chen X, Zhao L, Chen X (2021) Continuous renal replacement therapy without anticoagulation in critically ill patients at high risk of bleeding: a systematic review and meta-analysis. Semin Dial 34(3):196–208. https://doi.org/10.1111/sdi.12946. Epub 2021 Jan 5 PMID: 33400846
Kakajiwala A, Jemielita T, Hughes JZ, Windt K, Denburg M, Goldstein SL, Laskin B (2017) Membrane pressures predict clotting of pediatric continuous renal replacement therapy circuits. Pediatr Nephrol 32(7):1251–1261
Raina R, Sethi S, Khooblall A, Kher V, Deshpande S, Yerigeri K, Pandya A, Nair N, Datla N, McCulloch M, Bunchman T, Davenport A (2022) Non-anticoagulation pediatric continuous renal replacement therapy methods to increase circuit life. Hemodial Int 26(2):147–159. https://doi.org/10.1111/hdi.13003. Epub 2022 Jan 5 PMID: 34989465
Wang AY, Bellomo R (2018) Renal replacement therapy in the ICU intermittent hemodialysis, sustained low-efficiency dialysis or continuous renal replacement therapy? Curr Opin Crit Care 24(6):437–442
Zhang W, Bai M, Zhang L, Yu Y, Li Y, Zhao L, Yue Y, Li Y, Zhang M, Fu P, Sun S, Chen X (2022) Development and external validation of a model for predicting sufficient filter lifespan in anticoagulation-free continuous renal replacement therapy patients. Blood Purif 51(8):668–678
Acknowledgements
NA.
Funding
The Faculty of Medicine at Cairo University was responsible for the manuscript’s composition, data acquisition, analysis, and interpretation, as well as the study’s design. All authors read and approved the final manuscript.
Author information
Authors and Affiliations
Contributions
The patient data concerning the CRRT indications, the session prescription, and the anticoagulation procedure employed was analyzed and interpreted by FF and HM. SK, YA, and NM conducted the statistical analysis and were instrumental in the manuscript's composition. The final manuscript was reviewed and endorsed by all authors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The research ethics committee (REC), Faculty of Medicine, Cairo University has reviewed and authorized the study.
Consent for publication
NA.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fadel, F.I., Bazaraa, H.M., Anis, S.K. et al. Anticoagulation methods used and role of antithrombin III level monitoring in children on continuous renal replacement therapy: an observational cross-sectional study. Egypt Pediatric Association Gaz 72, 59 (2024). https://doi.org/10.1186/s43054-024-00298-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43054-024-00298-8