Abstract
Background
The dyslipidemia and changes in D-dimer values that occur in children with severe sepsis remain unidentified.
Objective
The current research aimed to explore the relationship between D-dimer and lipid profile values, including total cholesterol (TC), lipoproteins, apolipoprotein A-V (Apo A-5), triglycerides (TG), and in-hospital nonsurvival in children with severe sepsis or septic shock in pediatric intensive care.
Study design
The study design is as follows: prospective cohort study.
Participants
Children with severe sepsis or septic shock who were admitted to the intensive care unit of a university pediatric hospital.
Intervention
Vital signs, sepsis assessment, pediatric sequential organ failure assessment (PSOFA) score, high-density lipoprotein (HDL), Apo A-5, TG, low-density lipoprotein (LDL), TC, D-dimer, mortality outcome, and pediatric risk of mortality (PRISM) III score were evaluated.
Outcomes
The primary outcome was in-hospital nonsurvival.
Results
The nonsurvivors had significantly higher D-dimer levels than the survivors, with a significant cutoff level of 0.87 μg/mL (AUC: 0.85, sensitivity: 93.3%, PVN: 90.6%, accuracy: 79.0%, PVP: 72.5%, and specificity: 64.7%). D-dimer was inversely correlated with WBC count and positively correlated with patient age, PRISM III score, PSOFA score, and INR. However, nonsurvivors had higher TG levels and lower TC, HDL, LDL, and Apo A-5 levels than survivors, but this variation was insignificant. Apo A-5 levels were inversely correlated with HDL and positively correlated with TG levels.
Conclusions
This study suggests that D-dimer is a promising biomarker for severe sepsis in children, with a mortality cutoff level of 0.87 μg/mL. However, lipid profiles are not predictors of sepsis-related mortality.
Similar content being viewed by others
Background
In critical care settings, patients experience energy deficits and significant metabolic changes during their initial hospitalization in the pediatric intensive care unit (PICU). Septicemia can result in an abnormal immunological response, causing tissue damage and organ failure. Why some patients react severely to similar illnesses like sepsis while others do not is still a mystery [1,2,3].
One of the key features of sepsis is a disturbance in physiologically localized coagulation activity, which is a component of disseminated intravascular coagulation (DIC). Coagulopathy releases varying amounts of D-dimer due to concurrent coagulation activation and inhibition of natural anticoagulants and fibrinolysis. D dimer reflects the complex nature of the inappropriate body response to septicemia, leading to multisystem failure and higher mortality [4,5,6]. Therefore, we studied the association between the levels of D-dimer and in-hospital nonsurvival associated with sepsis in children.
Total cholesterol (TC) and lipoproteins are integral components of protection against inflammation or infection. They are responsible for regulating the generation of cytokines during an inflammatory reaction and suppressing the body’s response. They are required for the efficient functioning of both the adaptive and innate immune systems during an infection. Furthermore, lipoproteins are essential for the hepatic use of bioactive lipids for physiological defense [7,8,9].
Sepsis has the potential to induce dyslipidemia, a condition that is closely linked with sepsis-induced mortality. Nevertheless, these findings have only been reported in adult sepsis studies [10,11,12,13]. Recent interest has focused on assessing dyslipidemia in patients with sepsis due to reports of abnormal TC and lipoprotein levels in adults suffering from severe acute inflammatory diseases. According to the conclusions of these studies on adult patients, appropriate levels of TC, lipoproteins [low-density lipoprotein (LDL) and high-density lipoprotein (HDL)], apolipoproteins such as apolipoprotein A-V (Apo A-5), and triglycerides (TG) are required to fight infection successfully, but excess or deficient levels are detrimental [10,11,12,13].
Based on current knowledge, the impact of dyslipidemia and D-dimer values on children with severe sepsis remains undetermined. Hence, the current research attempted to investigate the relationship between D-dimer values as a coagulation indicator, lipid profile, and in-hospital nonsurvival in pediatric patients with severe sepsis/septic shock.
Methods
Criteria for patient inclusion and exclusion
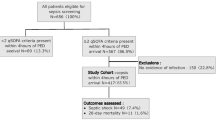
This prospective cohort study included 60 hospitalized patients exhibiting severe sepsis or septic shock in the PICU of a university tertiary hospital in conjunction with the clinical pathology department. It was executed between May 16, 2022, and April 30, 2023. Upon admission, we assessed the lipid profiles of consecutive patients ranging in age from 28 days to 16 years. Our patients were consecutively selected based on the diagnostic criteria, as outlined in Surviving Sepsis Campaign Worldwide Strategies 2020 [14] and the International Pediatric Sepsis Collaborative Committee (IPSCC 2005) [8]. Three factors were considered to be indicative of severe sepsis: (1) having at least two age-related systemic inflammatory response syndrome (SIRS) criteria (2) having an invasive infection that is confirmed or suspected; and (3) having cardiovascular dysfunction, acute respiratory distress syndrome (ARDS), or at least two non-cardiovascular organ dysfunctions. Septic shock was the term used to describe the subgroup of patients with cardiovascular dysfunction, which included hypotension, vasopressor treatment, or impaired perfusion. We excluded patients with known dyslipidemia, severe malnutrition, or end-stage disease (liver, renal, etc.). Patients receiving lipid containing parenteral nutrition upon admission or those recently receiving chemotherapy or steroid treatment were excluded.
Data collection
Data on patient age, sex, vital signs, sepsis assessment, including 24-h pediatric sequential organ failure assessment (PSOFA) [15, 16], and pediatric risk of mortality (PRISM) III [16, 17] were evaluated. Respiratory and circulatory care, feeding, drugs, transfusions, and surgical procedures were recorded on a daily basis. The outcome of interest was in-hospital nonsurvival, and our patients were divided into survivor and nonsurvivor groups. Using a Sysmex automatic cell counter (model XN 330), full blood counts were carried out. The coagulation process profile was assessed using a Sysmex automated blood-coagulation analysis tool, model CS 2100. On the Roche Cobas 8000 auto analyzer, c702 module, using spectrophotometry, tests for liver and kidney function, calcium, magnesium, and phosphorus levels were performed (Roche Diagnostics, Switzerland). C-reactive protein (CRP) was tested using the immunoturbidimetric technique on a Roche Cobas 8000 autoanalyzer, c702 module. Procalcitonin was measured by electrochemiluminescence on a Roche Cobas 8000 autoanalyzer using the e 602 module. We assessed the levels of TC, lipoproteins (LDL and HDL), Apo A-5, D-dimer, and TG.
Determination of lipid profile and D-dimer levels
A blood sample was taken from each patient upon admission. The lipid levels were measured according to the manufacturer’s recommendations. We tested LDL, HDL, TC, and TG levels using a Roche Cobas 8000 autoanalyzer, c702 module, by spectrophotometry. The APO-5 test blood sample was collected and separated in a plain sample vacutainer tube. The sample was centrifuged at 3000 rpm for 20 min after being left at room temperature, and the resultant serum was kept at – 20 °C. Shanghai Sunred Biological Technology Co., Ltd., China, provided the test kit (catalogue no. 201–12-5981). In accordance with the producer’s recommendations, we determined apolipoprotein A-V levels using a standard curve after an enzyme-linked immunosorbent assay (ELISA). The kit applies a double-antibody sandwich ELISA to analyze the value of serum APO-5 in each specimen. D-dimer was tested in patients’ citrated plasma using the immunoturbidimetric technique on a Roche Cobas 8000 autoanalyzer, c702 module, utilizing the manufacturer’s dedicated reagents.
Statistical analysis
To manage the present study’s data, SPSS version 23 was used. The mean plus standard deviation (SD) was employed for quantitative variables, but for qualitative variables, numbers and percentages were employed. Student’s “t” test compares the means of two distinct groups. Mann–Whitney test determined the difference between quantitative variables in two data groups that were not regularly distributed. To determine the relationship between the two groups, we used the chi-square test (χ 2). If one cell is less than 5, the Fisher exact test is performed instead of the chi-square test. A test for the correlation coefficient was used to compare several variables in a linear correlation that was either positive or negative. The ROC curve for the prognostic performance of TC, Apo A-5, lipoproteins, TG, and D-dimer in detecting PICU mortality associated with sepsis. The results that are significant have a probability value of ≤ 0.05. The value of probability > 0.05 denotes insignificant findings.
Results
The current study included 60 patients (38 had septic shock and 22 had severe sepsis), and thirty patients (50%) died. Age, baseline respiratory rate, PRISM III score, international normalized ratio (INR), PSOFA score, CRP, and mechanical ventilation requirements of the nonsurvivors were significantly higher than those of the survivors, as shown in Table 1.
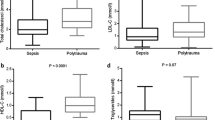
Nonsurvivors had higher TG levels and lower TC, HDL, LDL, and APO-5 levels than survivors, but this variation was insignificant. Additionally, they had significantly higher D-dimer levels than survivors, as demonstrated in Table 2.
The predictive performance of lipid profile and D-dimer for PICU mortality due to sepsis is shown in Table 3. Only D-dimer was shown to have a significant result, and the threshold (cutoff) level of D-dimer was 0.87 μg/mL (area under the curve (AUC): 0.85, sensitivity: 93.3%, predictive value negative (PVN): 90.6%, accuracy: 79.0%, predictive value positive (PVP): 72.5%, and specificity: 64.7%). However, lipid profile levels were not a significant prognostic factor for PICU mortality due to sepsis (Table 3).
D-dimer levels were inversely correlated with white blood cell (WBC) counts and positively correlated with patient age, PRISM III score, PSOFA score, and INR. APO A-5 levels were inversely correlated with HDL and positively correlated with TG, as shown in Table 4.
The ROC curve for the prognostic performance of APO A-5 and D-dimer for detecting sepsis-related in-hospital nonsurvival is shown in Fig. 1.
The ROC curve for the prognostic performance of lipid profile and procalcitonin for detecting sepsis-related in-hospital nonsurvival is shown in Fig. 2.
Discussion
In this unique study, our objectives were to identify the influence of lipid profile values and D-dimer levels, a coagulation indicator, on the prognosis of children with severe sepsis/septic shock. Significant variations in cholesterol and lipoprotein levels have been noticed during systemic inflammatory response conditions in adults [10,11,12,13, 18,19,20,21,22]. We concluded that nonsurvivors had significantly higher D-dimer levels than survivors and that D-dimer was inversely correlated with leucocyte count and positively correlated with patient age, PRISM III score, PSOFA score, and INR. The mortality cutoff value of D-dimer was 0.87 μg/mL (AUC: 0.85, sensitivity: 93.3%, PVN: 90.6%, accuracy: 79.0%, PVP: 72.5%, and specificity: 64.7%), indicating that D-dimer is a promising biomarker of severe sepsis. However, nonsurvivors of sepsis had higher TG levels and lower TC, HDL, LDL, and Apo A-5 levels than survivors, but this variation was insignificant. Lipid profile values are not reliable predictors of sepsis-related mortality.
Our findings are consistent with the study by Bermudes et al. [3], in which they found no significant differences in lipid profile alterations between sepsis survivors and nonsurvivors on the first day of PICU admission. Similarly, Maile and colleagues [23] failed to establish a significant correlation between HDL and mortality in adult patients. In addition, no significant difference in the levels of TG was observed between patients with sepsis, whether they survived or not, and healthy controls, according to Sharma et al. [24]. In contrast, Barlage et al. [10] observed that the lipid profile was significantly lower in nonsurvivors and predicted sepsis-associated fatality. According to Lee et al. [13], TC and CRP are inversely related, and lower TG levels are associated with sepsis mortality. Yildiz et al. [25] also observed reduced total cholesterol and lipoproteins, especially HDL, in neonates with sepsis compared with the control group and found an inverse relationship between inflammatory markers and HDL and TC levels. According to Wang et al. [26], serum Apo A-5 levels were significantly reduced in nonsurvivors and had predictive value for sepsis-associated multiorgan dysfunction in children. Ngaosuwan et al. [27] reported that children with sepsis had considerably greater absolute values of serum Apo A-5 than adult patients with sepsis and that Apo A-5 levels were significantly reduced in those who did not survive and were correlated with septic shock.
Our research revealed insignificant results regarding the reliability of the lipid profile in predicting death in children with severe sepsis. This might be explained by the characteristics of our study’s participants: presenting with severe sepsis, high PRISM III and PSOFA scores, and a mortality rate of 50%. The lipoproteins are vital throughout the infection recovery period. The relationship between lipoproteins and mortality is due to previous comorbid medical conditions or an indicator of disease progression [23].
Our study indicates that nonsurvivors had significantly higher D-dimer levels than survivors, and a threshold of 0.87 μg/mL was statistically significant as a predictor of mortality from sepsis, with good sensitivity (93.3%) and average specificity (64.7%). D-dimer has been shown to be inversely correlated with leucocyte count and to have a positive correlation with patient age, PRISM III score, PSOFA score, and INR. Our findings are comparable to those of Wang and colleagues [28], who recognized an association between D-dimer and PICU mortality with a threshold value of 1.53, 65% sensitivity, and 77% specificity. Jhang et al. [29] found that children experiencing septic shock had increased D-dimer levels, particularly in those who did not survive.
Although Foaud et al. [30] studied D-dimer levels in pediatric patients treated for trauma rather than sepsis, they found comparable results with the same sensitivity (90%) and higher specificity (100%). The discrepancies in cutoff values and specificity might be attributed to changes in sample size and participant demographics in different studies. Additionally, patients presenting with sepsis with higher D-dimer levels have a higher risk of death [31].
Sepsis can involve various procoagulant and fibrinolytic mechanisms, resulting in significant variation in the blood components of the immune reaction as well as the development of distinct forms of coagulopathies. This disparity affects key factors such as blood coagulation stimulation, suppression of natural anticoagulants, and fibrinolysis suppression. Coagulation indicators can be helpful in identifying the extent and/or form of coagulopathy that develops during sepsis. D-dimer represents a potential marker for identifying the various clinical forms of septicemia. Furthermore, D-dimer could potentially determine which patients would benefit from anti-inflammatory or anticoagulant treatments [5, 6, 32, 33].
D-dimer values are correlated with inflammatory biomarkers, including interleukins 6 and 8. The onset of DIC, particularly in sepsis, involves activation of the coagulation process and fibrin degradation. Such undesired events can dramatically increase the likelihood of multisystem organ failure and death [29, 34]. Patients with normal D-dimer levels had a lower mortality risk than those with abnormal levels, according to Lyngholm et al. [35].
Conversely, Semeraro et al. [36, 37] found that a correlation exists between reduced levels of D-dimer and decreased survival rates in patients with sepsis. These contradictory results should not be viewed as evidence that D-dimer is an unreliable marker of sepsis severity. Instead, they reflect its uniqueness in the context of different illnesses and infections.
The current study’s limitations included a relatively small number of participants, which precluded the demonstration of significant differences in lipid profile alterations. Additionally, the lack of a control group represents another limitation. Finally, since our study was conducted in a single tertiary center, the general applicability of the results may be limited by patient characteristics, financial resources, healthcare legislation, and staff quality.
The lessons learned from this research are that D-dimer fulfills the desired standards for a sepsis prognostic marker. D-dimer level is a good predictor of sepsis-related death. Regarding the lipid profile, nonsurvivors exhibit higher TG and lower TC, HDL, LDL, and Apo A-5 levels than survivors, but this disparity is statistically insignificant. Therefore, it is not advisable to rely on lipid profile values as predictors of sepsis-related mortality.
To our knowledge, the present research is one of the few published studies to date pertaining to the early assessment of lipid profiles and coagulation biomarkers (D-dimer) in patients with sepsis in this age group. The results of this study are pragmatic for clinical purposes and provide a foundation for future multicenter studies worldwide to further evaluate D-dimer and lipid profiles in pediatric patients with sepsis.
Conclusions
The current investigation suggests that D-dimer levels of nonsurvivors of severe sepsis are higher than those of survivors, with a mortality cutoff of 0.87 μg/mL (AUC: 0.85, sensitivity: 93.3%, and specificity: 64.7%), thereby establishing D-dimer as a promising biomarker for severe sepsis in children. Moreover, D-dimer levels were inversely correlated with the leucocyte count and positively correlated with patient age, PRISM III score, PSOFA score, and INR. However, it is worth noting that nonsurvivors exhibit higher TG and lower TC, HDL, LDL, and Apo A-5 levels than survivors, but this disparity is statistically insignificant. The lipid profiles are not predictors of sepsis-related mortality.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- Apo A-5:
-
Apo lipoprotein A-V
- ARDS:
-
Acute respiratory distress syndrome
- AUC:
-
Area under the curve
- CRP:
-
C-reactive protein
- DIC:
-
Disseminated intravascular coagulation
- ELISA:
-
Enzyme-linked immunosorbent assay
- HDL:
-
High-density lipoprotein
- INR:
-
International normalized ratio
- IPSCC:
-
International Pediatric Sepsis Collaborative Committee
- LDL:
-
Low-density lipoprotein
- PICU:
-
Pediatric intensive care unit
- PRISM:
-
Pediatric risk of mortality
- PSOFA:
-
Pediatric sequential organ failure assessment
- PVN:
-
Predictive value negative
- PVP:
-
Predictive value positive
- SIRS:
-
Systemic inflammatory response syndrome
- TC:
-
Total cholesterol (TC)
- TG:
-
Triglycerides
- WBC:
-
White blood cells
References
Delgado AF, Okay TS, Leone C, Nichols B, Del Negro GM, Vaz FA (2008) Hospital malnutrition and inflammatory response in critically ill children and adolescents admitted to a tertiary intensive care unit. Clinics (Sao Paulo) 63(3):357–362. https://doi.org/10.1590/s1807-59322008000300012. PMID:18568246;PMCID:PMC2664228
Calder PC, Jensen GL, Koletzko BV, Singer P, Wanten GJ (2010) Lipid emulsions in parenteral nutrition of intensive care patients: current thinking and future directions. Intensive Care Med 36(5):735–749. https://doi.org/10.1007/s00134-009-1744-5. Epub 2010 Jan 14. PMID: 20072779; PMCID: PMC2850535
Bermudes ACG, de Carvalho WB, Zamberlan P, Muramoto G, Maranhão RC, Delgado AF (2018) Changes in lipid metabolism in pediatric patients with severe sepsis and septic shock. Nutrition 47:104–109. https://doi.org/10.1016/j.nut.2017.09.015. Epub 2017 Oct 12 PMID: 29429528
Engelmann B, Massberg S (2013) Thrombosis as an intravascular effector of innate immunity. Nat Rev Immunol 13(1):34–45. https://doi.org/10.1038/nri3345. Epub 2012 Dec 7 PMID: 23222502
Semeraro N, Ammollo CT, Semeraro F, Colucci M (2012) Sepsis, thrombosis and organ dysfunction. Thromb Res 129(3):290–295. https://doi.org/10.1016/j.thromres.2011.10.013. Epub 2011 Nov 5 PMID: 22061311
Meini S, Sozio E, Bertolino G, Sbrana F, Ripoli A, Pallotto C et al (2021) D-Dimer as biomarker for early prediction of clinical outcomes in patients with severe invasive infections due to Streptococcus pneumoniae and Neisseria meningitidis. Front Med (Lausanne) 15(8):627830. https://doi.org/10.3389/fmed.2021.627830. PMID:33937280;PMCID:PMC8081958
Hofmaenner DA, Kleyman A, Press A, Bauer M, Singer M (2022) The many roles of cholesterol in sepsis: a review. Am J Respir Crit Care Med 205(4):388–396. https://doi.org/10.1164/rccm.202105-1197TR. PMID:34715007;PMCID:PMC8886946
Goldstein B, Giroir B, Randolph A, International Consensus Conference on Pediatric Sepsis (2005) International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. Pediatr Crit Care Med 6(1):2–8. https://doi.org/10.1097/01.PCC.0000149131.72248.E6. PMID: 15636651
Amunugama K, Pike DP, Ford DA (2021) The lipid biology of sepsis. J Lipid Res 62:100090. https://doi.org/10.1016/j.jlr.2021.100090. Epub 2021 Jun 1. PMID: 34087197; PMCID: PMC8243525
Barlage S, Gnewuch C, Liebisch G, Wolf Z, Audebert FX, Glück T et al (2009) Changes in HDL-associated apolipoproteins relate to mortality in human sepsis and correlate to monocyte and platelet activation. Intensive Care Med 35(11):1877–1885. https://doi.org/10.1007/s00134-009-1609-y. Epub 2009 Aug 8 PMID: 19669126
Lekkou A, Mouzaki A, Siagris D, Ravani I, Gogos CA (2014) Serum lipid profile, cytokine production, and clinical outcome in patients with severe sepsis. J Crit Care 29(5):723–727. https://doi.org/10.1016/j.jcrc.2014.04.018. Epub 2014 Apr 24 PMID: 24891152
Trinder M, Genga KR, Kong HJ, Blauw LL, Lo C, Li X, Cirstea M, Wang Y, Rensen PCN, Russell JA, Walley KR, Boyd JH, Brunham LR (2019) Cholesteryl ester transfer protein influences high-density lipoprotein levels and survival in sepsis. Am J Respir Crit Care Med 199(7):854–862. https://doi.org/10.1164/rccm.201806-1157°C. PMID: 30321485
Lee SH, Park MS, Park BH, Jung WJ, Lee IS, Kim SY, Kim EY, Jung JY, Kang YA, Kim YS, Kim SK, Chang J, Chung KS (2015) Prognostic implications of serum lipid metabolism over time during sepsis. Biomed Res Int 2015:789298. https://doi.org/10.1155/2015/789298. Epub 2015 Aug 17. PMID: 26351639; PMCID: PMC4553311
Weiss SL, Peters MJ, Alhazzani W, Agus MSD, Flori HR, Inwald DP et al (2020) Surviving sepsis campaign international guidelines for the management of septic shock and sepsis-associated organ dysfunction in children. Pediatr Crit Care Med 21(2):e52–e106. https://doi.org/10.1097/PCC.0000000000002198. PMID: 32032273
Ferreira FL, Bota DP, Bross A, Mélot C, Vincent JL (2001) Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA 286(14):1754–1758. https://doi.org/10.1001/jama.286.14.1754. PMID: 11594901
Lalitha AV, Satish JK, Reddy M, Ghosh S, George J, Pujari C (2021) Sequential organ failure assessment score as a predictor of outcome in sepsis in pediatric intensive care unit. J Pediatr Intensive Care 10(2):110117. https://doi.org/10.1055/s-0040-1714705. Epub 2020 Jul 30. PMID: 33884211; PMCID: PMC8052111
Pollack MM, Ruttimann UE, Getson PR (1988) Pediatric risk of mortality (PRISM) score. Crit Care Med 16(11):1110–1116. https://doi.org/10.1097/00003246198811000-00006. PMID: 3048900
Barlage S, Fröhlich D, Böttcher A, Jauhianen M, Müller HP, Noetzel F et al (2001) ApoE-containing high density lipoproteins and phospholipid transfer protein activity increase in patients with a systemic inflammatory response. J Lipid Res 42:281–290
Gordon BR, Parker TS, Levine DM, Saal SD, Wang JC, Sloan BJ et al (2001) Relationship of hypolipidemia to cytokine concentrations and outcomes in critically ill surgical patients. Crit Care Med 29:1563–1568
Lüthold S, Berneis K, Bady P, Müller B (2007) Effects of infectious disease on plasma lipids and their diagnostic significance in critical illness. Eur J Clin Invest 37:573–579
Levels JH, Pajkrt D, Schultz M, Hoek FJ, van Tol A, Meijers JC et al (2007) Alterations in lipoprotein homeostasis during human experimental endotoxemia and clinical sepsis. Biochim Biophys Acta 1771:1429–1438
Hudgins LC, Parker TS, Levine DM, Gordon BR, Saal SD, Jiang XC et al (2003) A single intravenous dose of endotoxin rapidly alters serum lipoproteins and lipid transfer proteins in normal volunteers. J Lipid Res 44:1489–1498
Maile MD, Sigakis MJ, Stringer KA, Jewell ES, Engoren MC (2020) Impact of the preillness lipid profile on sepsis mortality. J Crit Care 57:197–202. https://doi.org/10.1016/j.jcrc.2020.01.016. Epub 2020 Jan 14. PMID: 32182565; PMCID: PMC7391410
Sharma NK, Ferreira BL, Tashima AK, Brunialti MKC, Torquato RJS, Bafi A, Assuncao M, Azevedo LCP, Salomao R (2019) Lipid metabolism impairment in patients with sepsis secondary to hospital acquired pneumonia, a proteomic analysis. Clin Proteomics 16(16):29. https://doi.org/10.1186/s12014-019-92522. PMID:31341447;PMCID:PMC6631513
Yildiz B, Ucar B, Aksit A, Aydogdu SD, Colak O, Colak E (2009) Diagnostic values of lipid and lipoprotein levels in late onset neonatal sepsis. Scand J Infect Dis 41(4):263–267. https://doi.org/10.1080/00365540902767056. PMID: 19221931
Wang C, Cui Y, Miao H, Xiong X, Dou J, Shao L, Tang X, Zhang Y (2020) Apolipoprotein A-V is a novel diagnostic and prognostic predictor in pediatric patients with sepsis: a prospective pilot study in PICU. Mediators Inflamm 13(2020):8052954. https://doi.org/10.1155/2020/8052954. PMID:32322166;PMCID:PMC7157801
Ngaosuwan K, Houngngam N, Limpisook P, Plengpanich W, Khovidhunkit W (2015) Apolipoprotein A-V is not a major determinant of triglyceride levels during human sepsis. J Crit Care 30(4):727–731. https://doi.org/10.1016/j.jcrc.2015.03.026. Epub 2015 Apr 8 PMID: 25896654
Wang G, Liu J, Xu R, Liu X (2022) Elevated plasma D-dimer levels are associated with the poor prognosis of critically ill children. Front Pediatr 23(10):1001893. https://doi.org/10.3389/fped.2022.1001893. PMID:36210933;PMCID:PMC9537732
Jhang WK, Park SJ (2021) Evaluation of sepsis-induced coagulopathy in critically ill pediatric patients with septic shock. Thromb Haemost 121(4):457–463. https://doi.org/10.1055/s-0040-1718736. Epub 2020 Oct 29 PMID: 33124023
Foaud HM, Labib JR, Metwally HG, El-Twab KM (2014) Plasma D-dimer as a prognostic marker in ICU admitted Egyptian children with traumatic brain injury. J Clin Diagn Res 8(9):PC01-6. https://doi.org/10.7860/JCDR/2014/9489.4784. Epub 2014 Sep 20. PMID: 25386495; PMCID: PMC4225947
Rodelo JR, De la Rosa G, Valencia ML, Ospina S, Arango CM, Gómez CI et al (2012) D-dimer is a significant prognostic factor in patients with suspected infection and sepsis. Am J Emerg Med 30:1991–1999. https://doi.org/10.1016/j.ajem.2012.04.033
Seymour CW, Kennedy JN, Wang S, Chang CH, Elliott CF, Xu Z et al (2019) Derivation, validation, and potential treatment implications of novel clinical phenotypes for sepsis. JAMA 321:2003–2017. https://doi.org/10.1001/jama.2019.5791
Dhainaut JF, Yan SB, Joyce DE, Pettilä V, Basson B, Brandt JT et al (2004) Treatment effects of drotrecogin alfa (activated) in patients with severe sepsis with or without overt disseminated intravascular coagulation. J Thromb Haemost 2:1924–1933. https://doi.org/10.1111/j.1538-7836.2004.00955.x
Wang X, Zhang Q, Yan Y, Yang Y, Shang X, Li Y (2021) Clinical significance of pro-inflammatory cytokines and their correlation with disease severity and blood coagulation in septic patients with bacterial coinfection. Shock 56:396–402. https://doi.org/10.1097/SHK.0000000000001735
Lyngholm LE, Nickel CH, Kellett J, Chang S, Cooksley T, Brabrand M et al (2019) Negative D-dimer identifies patients at low risk of death within 30 days: a prospective observational emergency department cohort study. QJM 112:675–680. https://doi.org/10.1093/qjmed/hcz140
Semeraro F, Colucci M, Caironi P, Masson S, Ammollo CT, Teli R et al (2018) Platelet drop and fibrinolytic shutdown in patients with sepsis. Crit Care Med 46:e221–e228. https://doi.org/10.1097/CCM.0000000000002919
Semeraro F, Ammollo CT, Caironi P, Masson S, Latini R, Panigada M et al (2019) Low D-dimer levels in sepsis: good or bad? Thromb Res 174:13–15. https://doi.org/10.1016/j.thromres.2018.12.003
Acknowledgements
We would like to thank patients’ families for their willingness to participate in this study.
Funding
Nil.
Author information
Authors and Affiliations
Contributions
MAA, TAA, WII, EGB, and IAI conceived the study, participated in the study’s design, assisted in data collection, and participated in checking, analyzing and interpreting the data and drafting the manuscript. WII did the laboratory investigations and analyzed the results and interpreted the revealed data. MAA, TAA, IAI, and EGB analyzed and interpreted the laboratory measurements. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by Zagazig University Institutional Review Board (ZU-IRB # 9464/15–5-2022). The IRB approved that it is within the ethical guidelines as outline in the Declaration of Helsinki. The patients’ parents provided written informed consent to participate in this study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Abdelaziz, T.A., Mohamed, M.A.A., Ismail, W.I. et al. A prospective cohort study of severe sepsis-induced dyslipidemia and changes in D-dimer levels in children: do they affect the prognosis?. Egypt Pediatric Association Gaz 71, 93 (2023). https://doi.org/10.1186/s43054-023-00240-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43054-023-00240-4