Abstract
Background
Endothelial injury and systemic inflammation are key determinants of acute respiratory failure (ARF) outcome. We sought to determine if childhood obesity alters the degree of injury and inflammation in (ARF) patients with and without sepsis.
Methods
Plasma markers of endothelial injury (thrombomodulin), thrombosis (plasminogen activator inhibitor, PAI-1), and inflammation (IL-8 and IL-1ra) were measured over 3 days in children with ARF. Weight classification (healthy, overweight, and obesity) was determined by body mass index or weight‐for‐height z scores. Daily biomarker concentration and concentration change over time were compared among weight groups. Secondarily, we stratified by sepsis versus non-sepsis ARF.
Results
Twenty-six percent of the 229 children had obesity. Obesity was associated with longer duration of mechanical ventilation (median of 12 days compared to 7 days in the healthy weight, p = 0.006) and ICU stay (median of 18 days compared to 10 days in the healthy weight, p = 0.01 and compared to 11 days in the overweight, p = 0.02). Thrombomodulin levels were significantly higher in the obesity group on study days 1 and 2. In those with sepsis-associated ARF, thrombomodulin change over time increased most significantly in the obesity group (p = 0.015 for the interaction term of weight group and day on thrombomodulin concentration). There were no weight-based differences for IL-8, IL-1ra, or PAI-1.
Conclusions
Obesity was associated with elevated thrombomodulin, most notably in children with sepsis-associated ARF. This may denote worse endothelial injury in children with obesity and ARF. We found no difference in biomarkers of systemic inflammation among the weight groups.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Childhood obesity affects 14.7 million children and adolescents in the USA [1]. The excess adipose tissue is metabolically active and results in increased release of pro-inflammatory cytokines, including interleukin-1β (IL-1β), IL-6, IL-8, and tumor necrosis factor-α (TNF-α) [2, 3]. Elevated levels of plasminogen activator inhibitor-1 (PAI-1) and thrombomodulin, markers of antifibrinolysis and vascular endothelial dysfunction, respectively, have also been noted with obesity [2]. Chronic, low-grade systemic inflammation and endothelial dysfunction are key drivers for many obesity-associated morbidities and are present in both adults and children with obesity [4, 5].
Pediatric acute respiratory failure (ARF) and its most severe form, pediatric acute respiratory distress syndrome (PARDS), include some of the most critically ill children cared for in the pediatric intensive care unit (PICU). PARDS is characterized by heterogeneous damage to the alveolar-capillary barrier inducing an overly robust inflammatory reaction as well as injury to the pulmonary endothelium [6,7,8,9]. In adults and children with ARDS/PARDS, increased biomarkers of systemic inflammation, including IL-1β, interleukin 1 receptor antagonist (IL-1ra), IL-6, and IL-8, biomarkers of vascular endothelial dysfunction, such as thrombomodulin, and biomarkers of antifibrinolysis, like PAI-1, are associated with higher mortality [6, 10,11,12]. Because many of these biomarkers of ARDS/PARDS severity are the same as those chronically elevated with obesity, it might be inferred that individuals with obesity would have worse clinical outcomes from ARF. However, adult studies have shown similar or even lower mortality from ARF in patients with overweight and obese body habitus, known as the obesity paradox [13, 14]. In a study of plasma biomarkers of inflammation and injury in adults with ARDS, the patients with obesity had a reduced systemic inflammatory response but greater vascular endothelial injury compared to those of a healthy weight [15]. We previously found reduced risk of in-hospital mortality in PARDS patients with obesity compared to those of healthy weight; however, this finding was specific only to those whose PARDS was secondary to an indirect lung injury such as sepsis [16]. This suggests a variable mechanistic response to acute critical illness at the cellular level in children of different body habitus, but such findings have not previously been reported.
The objective of this study was to evaluate whether the degree and timing of systemic inflammation, endothelial injury, and antifibrinolysis in children with ARF differed among patients of different body habitus. In alignment with adult findings, we hypothesized that children with obesity would have lower plasma biomarker levels of systemic inflammation, but higher levels of endothelial injury compared to patients of healthy weight. This finding could be most pronounced in children whose ARF occurred because of sepsis.
Methods and materials
Design, settings, and patients
We performed a secondary analysis of children enrolled in the Genetic Variation and Biomarkers in Children with Acute Lung Injury (R01HL095410, BALI) study, an ancillary study to the Protocolized Sedation vs Usual Care in Pediatric Patients Mechanically Ventilated for Acute Respiratory Failure (RESTORE, HL086622/HL086649) clinical trial [17,18,19,20]. Thirty-one US PICUs participated in RESTORE from 2009 to 2013, and 22 of these also participated in BALI. RESTORE enrolled 2449 children who were 2 weeks to 17 years old receiving invasive mechanical ventilator support for at least 24 h for acute airway and/or parenchymal lung disease; 549 of these subjects were co-enrolled in BALI. A patient’s weight status did not affect their participation in either study.
BALI examined the association of plasma biomarkers with the development of PARDS. Blood samples were obtained after consent, then 24 and 48 h later for a maximum of three samples. In most cases (> 80%) sampling started between day 0 (day of intubation) and day 2, depending on time of consent. Plasma thrombomodulin, PAI-1, IL-8, and IL-1ra were measured using enzyme-linked immunosorbent assays (Thrombomodulin: Asserchrome, Diagnostica Stago; IL-8: #D800C; R&D Systems, Minneapolis, MN; IL-1ra: #DRAOOB, R&D Systems, Minneapolis, MN; PAI-1: #837 Seikisui Diagnostics, Stamford CT) [12, 18, 19, 21]. Assays were done in duplicate following the manufacturer’s protocol.
For this study on body habitus and plasma biomarker levels in children with ARF, we included all BALI subjects between 1 and 17 years old. Those less than 1 year of age were excluded because of growth variability associated with prematurity and variable feeding schedules. Patients without a documented admission height or weight, patients who were underweight, and patients without any biomarker measurements on days 0–3 were excluded.
Measurements and data collection
Weight-for-height (ages 1 to < 2 years) or body mass index (BMI, ages 2–17 years) z scores were calculated using hospital admission height and weight, accounting for patient age and gender based on the Center for Disease Control (CDC) growth charts [22]. Three weight groups were defined based on the 2006 CDC definitions: healthy weight (z-score − 1.89 to + 1.04, 4th to 84th percentile), overweight (z-score + 1.05 to + 1.65, 85th–95th percentile), and obesity (z-score ≥ + 1.65, > 95th percentile) [23].
Other data included age, gender, race, ethnicity, chronic comorbidities, prior pulmonary disease, immune compromised status, etiology of ARF, pediatric risk of mortality-III (PRISM-III) score [24], diagnosis of PARDS during the admission, and clinical outcomes including duration of mechanical ventilation, length of stay, and mortality.
Outcome measures and statistical analysis
Baseline characteristics and clinical outcomes of subjects in each weight group were compared by chi-square test for categorical variables and Kruskal–Wallis test with a post hoc Dunn’s test for multiple pairwise comparisons of continuous variables [25].
The primary outcomes were biomarker concentrations, which were log transformed for all analyses. We evaluated 4 distinct plasma biomarkers: thrombomodulin, PAI-1, IL-8, and IL-1ra, and each biomarker was analyzed separately for association with body habitus. Most patients had 2 or 3 days of plasma biomarker measurements over study days 0 to 3; however, only 13% of the cohort had biomarker measurements on day 0 (day of intubation); therefore, day 0 measurements were excluded from the analysis. On day 0 (n = 30 with 6 overweight and 8 with obesity) IL-8 levels increased significantly from healthy weight to overweight to obesity groups (coeff 2.12, 95%CI 0.14–4.1, p = 0.037 for univariate linear regression test), but no other biomarkers had weight-based differences. There were 119 (52%) subjects with biomarker measurements on day 1, 191 (83%) on day 2, and 181 (79%) on day 3.
We examined the cross-sectional plasma biomarker levels on each day across the three weight groups using a bivariate linear regression with a post-regression linear trend test. To evaluate whether the rate of change in plasma biomarker concentration across days 1 to 3 was different among the three weight groups, linear mixed effects models (LMEMs) were used, including all subjects that had at least 2 days of measurements of a specific biomarker. Covariates included in the multivariate LMEM were weight group, age, ethnicity, PRISM-III score, and sepsis-associated ARF (versus all other etiologies of ARF). These confounders were selected a priori because of known associations with weight status and/or etiology of lung injury. We used the AR(1) (autoregressive 1) covariance structure with a fixed effect of time in all LMEMs. An interaction term between weight group and day represented the slope of biomarker concentration change over time (i.e., across days) for each weight group and was analyzed using the Wald statistic.
As patients with sepsis-associated acute respiratory failure (sepsis ARF) have greater risk of multiple organ failure and death compared to other respiratory failure etiologies, and plasma biomarkers of systemic inflammation and endothelial injury are expectedly much higher in this group [26, 27], we repeated the LMEM analyses stratified by sepsis ARF (n = 50) versus non-sepsis ARF (n = 178). Covariates included in the stratified LMEMs were the same as in the primary analysis. A p value of ≤ 0.05 was considered as being statistically significant in all analyses. All analyses were performed using STATA version 15.1 (StataCorp, College Station, TX).
Results
Of the 549 BALI subjects, 229 met the age inclusion criteria and had no exclusion criteria. Those excluded were 173 subjects who were less than 1 year old, 47 subjects with insufficient or likely erroneous data to calculate a weight-for-height or BMI z-score, 34 who were underweight, and 66 with no biomarkers measured on the study days examined. Those with and without biomarker measurements were similar in demographics, clinical characteristics, and outcomes. In the final cohort of 229 patients, 59% (n = 136) had a healthy weight, 14% (n = 33) had overweight body habitus, and 26% (n = 60) had obesity. For the cross-sectional (individual day) analyses evaluating biomarker concentrations among the weight groups, data from all 229 patients was included. For the change in biomarker concentrations across days analysis, each LMEM included data from 223 to 227 patients so as to include only patients with at least 2 days of measurements of a specific biomarker.
Table 1 compares patient characteristics between the weight groups. There were no significant differences between weight groups regarding age, gender, race, ethnicity, chronic comorbidities, prior pulmonary disease, immune compromised status, diagnosis of PARDS, PRISM-III score, or death. Sepsis was listed as the primary etiology of ARF in 50 (22%) subjects. In a sub-analysis comparing sepsis ARF vs non-sepsis ARF, the proportion of patients in each weight group was not statistically significantly different (p = 0.08). Eighteen percent of the sepsis ARF group died while 9% of the non-sepsis ARF group died (p = 0.07).
In pairwise comparisons, patients with obesity had longer durations of mechanical ventilation (median 12 days) compared to healthy weight patients (median 7 days, p = 0.006), and patients with overweight body habitus (median 8 days, p = 0.04). The ICU length of stay was longer in survivors with obesity (median 18 days) compared to healthy weight survivors (median 10 days, p = 0.01), and patients with overweight body habitus (median 11 days, p = 0.02).
Thrombomodulin
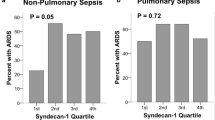
Concentrations of plasma thrombomodulin on each of the 3 days in the various weight groups are shown in Supplemental Figure S1a. Cross-sectional analysis showed that on days 1 and 2 after intubation, the obesity group had a significantly higher log-thrombomodulin concentration than the healthy weight group (day 1 linear regression coefficient 0.33 [95% CI 0.05, 0.62] and day 2 coefficient 0.26 [95% CI 0.05, 0.47]). The linear trend across all days in log-thrombomodulin concentration as weight group increased were also significant on day 1 (p = 0.02) and day 2 (p = 0.01). Day 3 thrombomodulin concentrations were not significantly different between the three weight groups. In the multivariate LMEM of the whole cohort, which considers the change in biomarker concentration across days for each patient, the slope of log-thrombomodulin concentration from day 1 to 3 was not statistically significantly different among the weight groups (Fig. 1a).
Adjusted linear mixed effects models of biomarkers over time in patients of healthy weight, overweight, and obesity body habitus. The left column represents evaluation of the whole cohort (n = 229), the middle column represents patients with sepsis-associated acute respiratory failure (n = 50), and the right column represents patients with non-sepsis acute respiratory failure (n = 179). a–c are plasma thrombomodulin, d–f are plasma PAI-1, g–i are plasma IL-8, and j–l are plasma IL-1ra. The slope of biomarker change over time is statistically significant between weight groups in b (thrombomodulin in the sepsis ARF group)
Cross-sectional concentrations of plasma thrombomodulin on days 1–3 in the sepsis ARF and non-sepsis ARF strata are shown in Supplemental Figs. 2a, b respectively. Overall, thrombomodulin concentrations were statistically significantly higher in the sepsis ARF group versus the non-sepsis ARF group on all three study days, but the weight group was not associated with thrombomodulin concentration on any day within either the sepsis ARF or non-sepsis ARF groups. In the multivariate LMEM of the sepsis ARF subgroup (Fig. 1b), the slope of log-thrombomodulin concentration from day 1 to 3 was significantly different among the weight groups (p = 0.015 for the interaction term of weight group and day), with log-thrombomodulin concentration increasing across days in patients with either overweight or obesity body habitus compared to no change across days in those with healthy weight. In contrast, for the non-sepsis ARF group, the slope of log-thrombomodulin concentration was similar among the weight groups with minimal change across the three study days for all weight groups (Fig. 1c).
PAI-1, IL-8, and IL-1ra
On cross-sectional evaluation for an association between weight group with biomarker concentrations on days 1–3, we found no statistically significant relationship for PAI-1, IL-8, or IL-1ra with weight group on any day for the whole cohort analysis (Supplemental Figure S1, b–d) or for the sepsis ARF or non-sepsis ARF sub-groups (Supplemental Figure S2, c–h)). Similarly, the multivariate LMEMs of the whole cohort, and the sepsis ARF and non-sepsis-ARF strata, showed no association between weight group and change across days in PAI-1, IL-8, or IL-1ra concentrations (Fig. 1d–l).
Discussion
In this BALI cohort, we found that 26% of patients had obesity, and obesity was associated with longer durations of mechanical ventilation and ICU level care. Children with obesity had higher plasma thrombomodulin on study days 1 and 2 compared to children of healthy weight. In patients with ARF from sepsis, children with obesity had a persistent and greater rate of increase in plasma thrombomodulin over time compared to their healthy weight peers. There were no weight-based differences in IL-8, IL-1ra, or PAI-1. Key strengths of this work include this as one of the first evaluations of longitudinal change over time in biomarkers of systemic inflammation, endothelial injury, and antifibrinolysis in children with acute respiratory failure, as well as evaluating of the impact of body habitus on biomarkers of stress during critical illness in children.
The recent COVID-19 pandemic clearly highlighted the importance of obesity as a comorbid condition in patients with acute respiratory failure. High-risk patient populations, including those with obesity, often presented with severe ARDS and mortality rates were high. Autopsies performed on deceased COVID-19 ARDS patients showed that endothelial dysfunction and microvascular thrombi were common findings, suggesting that treatment focused on minimizing endothelial dysfunction in acute respiratory failure is a promising approach to protect vulnerable patients, such as those with obesity [28].
Endothelial dysfunction results in vasoconstriction, inflammation, increased permeability, and coagulopathy. High plasma thrombomodulin indicates the loss of this antithrombotic molecule within the vasculature. In patients with ARF, elevated thrombomodulin infers greater risk of microthrombi development and subsequently an increase in pulmonary dead space ventilation, another strong predictor of poor outcome [29, 30]. Our finding of persistently higher plasma thrombomodulin levels in children with obesity and ARF might indicate a greater risk of microthrombi development and increased pulmonary dead space in those with obesity. This provides a reasonable explanation for adult and pediatric ARF patients with obesity consistently having longer durations of mechanical ventilation than their healthy weight peers [14, 16]. Since the RESTORE trial did not record dead space ventilation, we were not able to correlate thrombomodulin levels to degree of dead space, but it does highlight the need for future investigation.
In contrast to the differential thrombomodulin response among the weight groups, we found no difference in plasma IL-8, IL-1ra, or PAI-1 in children of different body habitus on day 1, 2, or 3 after intubation. Our findings are similar to a recent single-center study in adults with COVID-19 ARF that showed no BMI-based difference in inflammatory cytokine levels over time, including IL-6, IL-8, IL-1ra, or TNF-α. This study did not evaluate biomarkers of endothelial injury or disordered coagulation [31]. A pre-pandemic multicenter ARDS Network study of adults with ARDS also evaluated the association of obesity with biomarker levels of inflammation, endothelial injury, and disordered coagulation. These investigators found that on study day 0, plasma IL-8 decreased as BMI increased. A similar finding on study day 3 was not statistically significant after covariate adjustment. Two other inflammatory biomarkers, TNF-α and IL-6, did not differ between patients of different body habitus. Similar to our results, PAI-1 was no different among the weight groups. That study did not evaluate thrombomodulin [15]. Our findings, in addition to those by the above two adult studies, indicate that despite being chronically inflamed, once a patient becomes critically ill, the systemic inflammatory response may not be greatly influenced by the patients’ body habitus.
Many interventional studies aimed at improving outcomes in ARDS/PARDS have failed to find valuable treatments, likely due to the heterogeneity of the disease and patient population. Phenotyping ARDS/PARDS using clinical, physiologic, and biologic data have identified subgroups of patients with distinct clinical outcomes and treatment responses [27, 32,33,34]. This has prompted a call to arms to perform phenotype-aware trials that consider pathophysiologic pathways of lung injury in various forms of ARDS/PARDS and translate such discoveries into personalized, precision-based therapies [35]. Numerous observational studies in both children and adults reveal great potential for personalized care plans based on treatable traits [36,37,38,39]. Our study evaluated biomarker change over time during the early period of critical illness, a unique analysis in ARDS/PARDS biomarker research, which has typically evaluated a single timepoint or a difference between two timepoints. We identified a distinct pattern in thrombomodulin change among sepsis patients of different body habitus, hinting at a sustained difference in pathobiology that could portend differential response to treatment, if such trajectory analyses are included in future randomized controlled trials. This finding of persistent, elevated thrombomodulin in patients with obesity, in addition to our previous findings of lower biomarkers of alveolar epithelial injury in patients with obesity, indicates that body habitus may be an important phenotype to account for in future PARDS treatment trials [40].
This study has some limitations. Firstly, there is no standard definition for pediatric obesity and different health organizations use different methodologies and cut-off points [41, 42]. We used CDC definitions that divide weight status into patients with healthy weight, overweight, or obesity. More recent studies often sub-divide obesity into 3 severity classes, but our cohort size prevented this level of analysis. Secondly, few patients were enrolled in time to collect biomarker data for day 0 (day of intubation) due to a 24- to 48-h consent window, which prevented us from evaluating weight-based differences on this day. This early period is likely very important in the evaluation of the acute systemic response to critical illness in children of different weights, as it would highlight any rapid changes from chronic inflammation (with obesity) to the more acute response. Thirdly, the strata sizes for the stratified analyses were quite small preventing any investigation on the clinical impact of the weight-based variability in these groups. Future studies of patients with ARF and/or sepsis are necessary to elucidate whether weight-based differences in cellular response have any impact on clinical outcomes.
Conclusion
In summary, we have found that in children with ARF plasma thrombomodulin, a biomarker of endothelial injury, is elevated on days 1 and 2 in children with obesity compared to their healthy weight peers. In children whose ARF is due to sepsis, the rate of rise in plasma thrombomodulin continues at a greater degree in those with obesity, suggesting that the degree of endothelial injury from sepsis and ARF is greater in those with obesity. This pathologic difference may partially explain longer durations of mechanical ventilation in ARF patients with obesity. We did not find an association between body habitus and degree of systemic inflammation or antifibrinolysis. Future studies are needed to better understand the association between childhood obesity, increased endothelial injury and altered respiratory mechanics in children with ARF and/or sepsis.
Availability of data and materials
The RESTORE main trial datasets are publicly available in the NHLBI Biologic Specimen and Data Repositories Information Coordinating Center (BioLINCC) data repository (https://biolincc.nhlbi.nih.gov/studies/restore/), but the BALI datasets are not yet publicly available. We are in the process of preparing the BALI datasets and associated documentation for submission to BioLINCC.
References
Stierman B, Afful J, Carroll M et al (2021) National Health and Nutrition Examination Survey 2017 - March 2020 Prepandemic Data Files Development of Files and Prevalence Estimates for Selected Health Outcomes. National Health Statistics Reports, no 158, Hyattesville
Subramanian V, Ferrante AW (2009) Obesity, inflammation, and macrophages. Nestle Nutr Workshop Ser 63:151–162
Ferrante A (2007) Obesity-induced inflammation : a metabolic dialogue in the language of inflammation. J Int Med 262:408–414
Carolan E, Hogan AE, Corrigan M et al (2014) The impact of childhood obesity on inflammation, innate immune cell frequency, and metabolic MicroRNA expression. J Clin Endocrinol Metab 99(3):E474-8. https://doi.org/10.1210/jc.2013-3529
Visser M, Bouter LM, McQuillan GM, Wener MH, Harris TB (2001) Low-grade systemic inflammation in overweight children. Pediatrics 107(1):e13–e13. https://doi.org/10.1542/peds.107.1.e13. ([cited 2013 Nov 14])
Calfee CS, Gallagher D, Abbott J, Thompson BT, Matthay MA, Network the NA (2012) Plasma angiopoietin-2 in clinical acute lung injury: prognostic and pathogenetic significance. Crit Care Med 40(6):1731–7
Ware LB, Eisner MD, Thompson BT, Parsons PE, Matthay MA (2004) Significance of Von Willebrand factor in septic and nonseptic patients with acute lung injury. Am J Respir Crit Care Med 170(7):766–772
Flori HR, Ware LB, Milet M, Matthay MA (2007) Early elevation of plasma von Willebrand factor antigen in pediatric acute lung injury is associated with an increased risk of death and prolonged mechanical ventilation. Pediatric Critical Care Med 8(2):96–101. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3586228/)
Ware LB, Matthay MA. Acute respiratory distress syndrome. N Engl J Med 2000;342. Available from: http://dx.doi.org/https://doi.org/10.1056/NEJM200005043421806
Zinter MS, Orwoll BE, Spicer AC et al (2017) Incorporating inflammation into mortality risk in pediatric acute respiratory distress syndrome. Crit Care Med 45(5):858–866
Calfee CS, Ware LB, Eisner MD et al (2008) Plasma receptor for advanced glycation end products and clinical outcomes in acute lung injury. Thorax 63(12):1083–1089
Parsons P, Eisner M et al (2005) Lower tidal volume ventilation and plasma cytokine markers of inflammation in patients with acute lung injury. Crit Care Med 33(1):1–6
O’Brien JM, Phillips GS, Ali NA, Lucarelli M, Marsh CB, Lemeshow S (2006) Body mass index is independently associated with hospital mortality in mechanically ventilated adults with acute lung injury. Crit Care Med 34(3):738–44
Akinnusi ME, Pineda LA, El Solh AA (2008) Effect of obesity on intensive care morbidity and mortality: a meta-analysis. Crit Care Med 36(1):151–8
Stapleton RD, Dixon AE, Parsons PE, Ware LB, Suratt BT (2010) The association between BMI and plasma cytokine levels in patients with acute lung injury. Chest 138(3):568–577
Ward SL, Gildengorin V, Valentine SL et al (2016) Impact of weight extremes on clinical outcomes in pediatric acute respiratory distress syndrome. Crit Care Med 44(11):2052–2059
Curley M, Wypij D, Watson R (2015) Protocolized sedation vs usual care in pediatric patients mechanically ventilated for acute respiratory failure: a randomized clinical trial. JAMA 313(4):379–389
Flori H, Sapru A, Quasney MW et al (2019) A prospective investigation of interleukin-8 levels in pediatric acute respiratory failure and acute respiratory distress syndrome. Crit Care 23(1):128
Dahmer MK, Quasney MW, Sapru A et al (2018) Interleukin-1 receptor antagonist is associated with pediatric acute respiratory distress syndrome and worse outcomes in children with acute respiratory failure. Pediatr Crit Care Med 19(10):930–938
Monteiro ACC, Flori H, Dahmer MK et al (2021) Thrombomodulin is associated with increased mortality and organ failure in mechanically ventilated children with acute respiratory failure: biomarker analysis from a multicenter randomized controlled trial. Crit Care 25(1):271
Orwoll BE, Spicer AC, Zinter MS, Alkhouli MF, Khemani RG, Flori HR (2015) Elevated soluble thrombomodulin is associated with organ failure and mortality in children with acute respiratory distress syndrome (ARDS): a prospective observational cohort study. Crit Care 19:435
Kuczmarski RJ, Ogden CL, Guo SS et al (2002) 2000 CDC Growth Charts for the United States: methods and development
Barlow SE (2007) Expert Committee Recommendations Regarding the Prevention, Assessment, and Treatment of Child and Adolescent Overweight and Obesity : Summary Report. Pediatrics 120:S164–S192
Pollack MM, Patel KM, Ruttimann UE (1997) The pediatric risk of mortality III— Acute physiology score (PRISM III-APS): A method of assessing physiologic instability for pediatric intensive care unit patients. J Pediatr 131(4):575–581
Dinno A (2015) Nonparametric pairwise multiple comparisons in independent groups using Dunn’s test. Stata J 15(1):292–300
Khemani RG, Smith L, Lopez-Fernandez YM et al (2019) Paediatric acute respiratory distress syndrome incidence and epidemiology (PARDIE): an international, observational study. Lancet Respir Med 7(2):115–128
Calfee CS, Janz DR, Bernard GR et al (2014) Distinct molecular phenotypes of direct versus indirect ARDS in single and multi-center studies. Chest J 147(6):1539–1548
Nägele MP, Haubner B, Tanner FC, Ruschitzka F, Flammer AJ (2020) Endothelial dysfunction in COVID-19: Current findings and therapeutic implications. Atherosclerosis 314:58–62
Bhalla AK, Belani S, Leung D, Newth CJL, Khemani RG (2015) Higher dead space is associated with increased mortality in critically ill children. Crit Care Med 43(11):2439–45. Available from: http://journals.lww.com/ccmjournal/Fulltext/2015/11000/Higher_Dead_Space_Is_Associated_With_Increased.21.aspx
Matthay MA, Kallet RH (2011) Prognostic value of pulmonary dead space in patients with the acute respiratory distress syndrome. Crit Care 15(5):185. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3334730/
Kooistra EJ, De Nooijer AH, Claassen WJ et al (2021) A higher BMI is not associated with a different immune response and disease course in critically ill COVID-19 patients. Int J Obes 45:687–694
Calfee CS, Delucchi K, Parsons PE et al (2014) Subphenotypes in acute respiratory distress syndrome: latent class analysis of data from two randomised controlled trials. Lancet Respir Med 2(8):611–620
Dahmer MK, Yang G, Zhang M et al (2022) Identification of phenotypes in paediatric patients with acute respiratory distress syndrome: a latent class analysis. Lancet Respir Med 10(3):289–297
Sinha P, Delucchi KL, Chen Y et al (2022) Latent class analysis-derived subphenotypes are generalisable to observational cohorts of acute respiratory distress syndrome: a prospective study. Thorax 77(1):13–21
Narges A, Calfee CS (2022) Phenotyping in acute respiratory distress syndrome: state of: Current Opinion in Critical Care. Curr Opin Crit Care 28(1):1–8
Rizzo AN, Aggarwal NR, Thompson BT, Schmidt EP (2023) Advancing Precision Medicine for the Diagnosis and Treatment of Acute Respiratory Distress Syndrome. J Clin Med 12(4):1563
Flori HR, Zhang M, Xie J, Yang G, Sapru A, Calfee CS, Delucchi KL, Sinha P, Curley MAQ, Dahmer MK (2023) Subphenotypes Assigned to Pediatric Acute Respiratory Failure Patients Show Differing Outcomes. Am J Respir Crit Care Med 208(3):331–333
Beitler JR, Goligher EC, Schmidt M et al (2016) Personalized medicine for ARDS: The 2035 Research Agenda. Intensive Care Med 42(5):756–767
De Luca D (2019) Personalising care of acute respiratory distress syndrome according to patients’ age. Lancet Respir Med 7(2):100–101
Ward SL, Dahmer MK, Weeks HM et al (2020) Association of patient weight status with plasma surfactant protein D, a biomarker of alveolar epithelial injury, in children with acute respiratory failure. Pediatr Pulmonol 55:2730–2736
Ward SL, Quinn CM, Steurer MA, Liu KD, Flori HR, Matthay MA (2018) Variability in pediatric ideal body weight calculation: implications for lung-protective mechanical ventilation strategies in pediatric acute respiratory distress syndrome. Pediatr Crit Care Med 19(12):e643–e652
Ward S, Flori H. Differences in weight classification and dangerous Implications for critically ill children. Obesity Society Obesity Week Annual Conference, Los Angeles 2015;Abstract
Acknowledgements
We thank the study participants and their families and guardians for their participation in this study.
Funding
This study was funded by a K12 grant from the NIH awarded to Dr. Ward (K12HD047349). The parent studies were supported by grants from the NIH awarded to Drs. Dahmer, Flori, and Quasney (R01HL095410) for BALI study and Dr. Curley (U01HL086622, U01 HL086649) for the RESTORE study.
Author information
Authors and Affiliations
Consortia
Contributions
Drs. Ward, Flori, Curley, Liu, and Matthay conceived of and designed the study. Drs. Ward, Flori, Dahmer, Weeks, Sapru, Quasney, and Curley participated in data acquisition and interpretation. Drs. Ward, Flori, Dahmer, and Weeks conducted the data analysis. Dr. Ward prepared the first draft of the manuscript, and all authors revised the draft critically. All authors have approved the final manuscript for publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The legal guardians of all patients enrolled in the parent RESTORE and BALI studies provided informed consent for the enrollment of their child in these studies. Child assent was waived by the Internal Review Boards because eligible subjects were typically sedated during their treatment and study course, rendering them unable to provide assent.
Competing interests
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests:
Drs. Matthay, Flori, Sapru, Curley, Quasney, Dahmer, and Flori reports financial support was provided by the National Heart Lung and Blood Institute. Dr. Ward reports financial support was provided by the National Institute of Child Health and Human Development. Dr. Flori reports a non-financial advisory relationship with Aerogen Pharma and Lucira Health, Inc. Dr. Liu serves as a consultant for Biomerieux, BOA Medical, and Seastar Medical. Dr. Liu reports a relationship with Amgen Inc that includes equity or stocks. Dr. Liu serves on the Editorial Boards of the American Journal of Kidney Diseases, American Journal of Respiratory and Critical Care Medicine, and CJASN, and as a scientific advisor of the NKF Scientific Advisory Board and American Thoracic Society. Dr. Matthay has received grant funding from Roche-Genetech, not associated with the work of this manuscript. Dr. Matthay serves as a consultant for Citrus Pharmaceuticals Johnson & Johnson, Gilead Pharmaceuticals, Plant Therapeutics, Novartis Pharmaceuticals, and AM Pharma.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Supplemental Figure S1. Median and Interquartile range of plasma biomarker concentrations on study days 1, 2 and 3 among patients with healthy weight, overweight, or obesity. Note Y-axes vary for each biomarker. Supplemental Figure S2. Median and Interquartile range of plasma biomarker concentrations on days 1, 2 and 3 among weight groups, stratified by sepsis ARF versus non-sepsis ARF. Note: y-axes vary for each biomarker.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ward, S.L., Flori, H.R., Dahmer, M.K. et al. Inflammatory and coagulant responses after acute respiratory failure in children of different body habitus. Intensive Care Med. Paediatr. Neonatal 1, 16 (2023). https://doi.org/10.1007/s44253-023-00015-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44253-023-00015-0