Abstract
Background
Colorectal cancer (CRC) ranks third in cancer incidence globally and is the second leading cause of cancer-related mortality. The nucleoside diphosphate kinase 1 (NME1) and netrin 1 receptor (DCC) genes have been associated with resistance against tumorigenesis and tumor metastasis. This study investigates the potential association between NME1 (rs34214448 G > T and rs2302254 C > T) and DCC (rs2229080 G > C and rs714 A > G) variants and susceptibility to colorectal cancer development.
Methods
Samples from 232 colorectal cancer patients and 232 healthy blood donors underwent analysis. Variants were identified using polymerase chain reaction-restriction fragment length polymorphism (PCR–RFLP) methodology. Associations were assessed using odds ratios (OR), and the p values were adjusted with Bonferroni test.
Results
Individuals carrying the G/T and T/T genotypes for the NME1 rs34214448 variant exhibited a higher susceptibility for develop colorectal cancer (OR = 2.68, 95% CI: 1.76–4.09, P = 0.001 and OR = 2.47, 95% CI: 1.37–4.47, P = 0.001, respectively). These genotypes showed significant associations in patients over 50 years (OR = 2.87, 95% CI: 1.81–4.54, P = 0.001 and OR = 2.99, 95% CI: 1.54–5.79, P = 0.001 respectively) and with early Tumor-Nodule-Metastasis (TNM) stage (P = 0.001), and tumor location in the rectum (P = 0.001). Furthermore, the DCC rs2229080 variant revealed that carriers of the G/C genotype had an increased risk for develop colorectal cancer (OR = 2.00, 95% CI: 1.28–3.11, P = 0.002) and were associated with age over 50 years, sex, and advanced TNM stages (P = 0.001).
Conclusions
These findings suggest that the NME1 rs34214448 and DCC rs2229080 variants play a significant role in colorectal cancer development.
Similar content being viewed by others
Introduction
Colorectal cancer (CRC) is ranked as the third most diagnosed cancer globally and contributes significantly to cancer-related mortality worldwide [1]. According to Globocan 2022, the incidence of CRC in Mexico in 2022 showed a ratio of 12.2 per 100,000 individuals, with a mortality ratio of 6.3 per 100,000 inhabitants [1]. The development of CRC involves a multifactorial combination of events, including genetic alteration and epigenetic changes, leading to abnormalities in the normal colonic mucosa. Inactivation of tumor suppressor genes through deletion or mutation in the remaining allele plays a significant role in cancer progression and metastasis [2]. The process of metastasis itself is complex and includes several stages, the molecular regulation of which remains poorly understood. Tumor suppressor genes as nucleoside diphosphate kinase 1 (NME1) and netrin 1 receptor (DCC) are crucial in the development of metastasis [3, 4].
The NME1 gene, located on chromosome 17q21, consists of 6 exons and encodes the NME1 protein, also known as NME1-H1 or NM23-H1, which is member of a family of 10 NME1 genes [5]. Numerous research studies have demonstrated that NME1 functions as a metastasis suppressor gene, exhibiting suppressive activity across a wide range of human cancers. NME1 is involved in various processes, including transcription, regulation of deoxyribonucleic acid (DNA) replication, and cell differentiation, both in normal and tumorigenic cells [6, 7]. Additionally, NME1, along with TP53 and MDM2, plays a significant role in the ERK and K-RAS signaling pathways. Changes in NME1 expression levels result in decreased activation of the ERK signaling pathway [8].
The DCC gene, composed of 29 exons, is located on chromosome 18q21. It encodes the Netrin 1 receptor, a transmembrane receptor belonging to the immunoglobulin superfamily. Neurons abundantly express DCC and plays roles in promoting cell survival and axon regeneration [9]. Research indicates that this gene functions as both a tumor suppressor and a metastasis suppressor. It is involved in various cellular processes including cell division, migration, apoptosis, cell cycle arrest, cell differentiation, embryonic development, and metastasis. Studies suggest that loss of heterozygosity (LOH) and other alterations in DCC are linked with poor differentiation, metastasis, and an unfavorable prognosis in CRC [10,11,12,13].
The impact of NME1 rs34214448 (c.-5 + 989G > T) and rs2302254 (c.-128C > T) variants, as well as DCC rs2229080 (c.-601G > C) and rs714 A > G (intronic) variants on cancer susceptibility, prognosis, or survival has been investigated across various cancers types, including esophageal, gastric adenocarcinoma, gallbladder, breast, cervicouterine, ovarian, leukemia, and colorectal cancer [14,15,16,17,18,19,20,21,22]. However, only two studies have been conducted on the NME1 rs34214448 variant in the Caucasian population [18, 23] and the DCC rs2229080 variant in the Indian population for colorectal cancer [24].
This study aims to investigate, for the first time, the allele and genotype distribution of the NME1 gene (rs2302254) and the DCC gene (rs2229080 and rs714) variants; and to assess their potential association of NME1 (rs34214448 and rs2302254) and the DCC (rs2229080 and rs714) of this gene variants with the clinicopathological characteristics and the development of CRC in Mexican patients.
Materials and methods
Study population
This study protocol underwent evaluation by the Scientific Research Committee of the Mexican Social Security Institute (IMSS) and was approved with the register number: R-2018–1305-001. All procedures were conducted in accordance with national and international ethical standards. Informed consent forms were obtained from each participant, both patients and controls, before the commencement of the study, authorizing their participation and the collection of blood samples. A total of 464 individuals were included in the study: 232 patients diagnosed with sporadic colorectal adenocarcinoma, confirmed through clinical features and histological examination, according with the Clinical Practice Guidelines on Colon and Rectal Cancer, as well as the clinicopathologic criteria from the Hospital de Especialidades del IMSS in Guadalajara, Mexico. Patients were enrolled in a non-probabilistic consecutive manner during consultation at this institution between 2018 to 2022. Clinical stages of CRC were based on Tumor-Nodule-Metastasis (TNM) classification system. Blood samples were collected during clinical visits before the initiation of chemotherapy or radiotherapy. The control group comprised 232 unrelated subjects (109 men and 123 women), with negative findings for malignancy upon colonoscopy. For both groups the age was matched. Exclusion criteria for both patients and controls included a diagnosis of autoimmune or inflammatory bowel disease (Crohn’s disease and ulcerative colitis), as well as a known history of hereditary cancer. The entire study population resided in the metropolitan area of Guadalajara, Mexico, and all belonged to the mixed-race category. Clinical information, including age, sex, smoking and drinking habits, family history, symptoms, and clinicopathological characteristics, was obtained by consulting hospital medical records.
Genotyping
Genomic DNA from peripheral blood lymphocytes was isolated using the Miller, Dykes & Polesky, method [25]. The rs34214448 (G > T) and rs2302254 (C > T) variants of NME1 gene and rs2229080 (G > C) and rs714 (A > G) of DCC gene, were genotyped by polymerase chain reaction–restriction fragment length polymorphism (PCR–RFLP) method. For NME1 (rs34214448) variant was performed using the forward primer F: 5´- CCC ACC GTT TAT TGG CTA G-3´ and the reverse primer 5´- CAA CCC CCT TCA TTT TAC AA-3´ [17] and for NME1 rs2302254 variant with the forward primer 5´- CGC GAA CGA AGG AAG TGA GTC A-3´ and reverse primer 5´- GCC GCC AGC ACC CGA AAC-3´ [25]. For DCC (rs2229080) variant was performed using the forward primer F: 5´- ATT TGG AAG ACT TAT TCT TCC-3´ and the reverse primer 5´- CGG TAA ATT CCA AGT CCC TCG GTT GGA GC-3´ and for DCC rs714 variant with the forward primer 5´- TGC ACC ATG CTG AAG ATT GT-3´ and reverse primer 5´- AGT ACA ACA CAA GGT ATG TG-3´ [21]. PCR reaction for NME1 (rs34214448 and rs2302254) and DCC (rs2229080 and rs714) variants was performed for 35 cycles in a 10 μL volume containing 100 ng DNA, 10X buffer (500 mM KCl, 100 mM Tris–HCl, and 0.1% Triton™ X-100), 2.0 mM MgCl2, 200 mM dNTPs, 1 pM of each primer, and 2U Taq DNA Polymerase (Thermo Fisher Scientific, USA) according to the following amplification program: initial denaturation at 94 °C for 5 min, 32 cycles of denaturation at 94 °C for 30 s, annealing at 58℃ for (rs34214448), 62℃ for (rs2302254), 58℃ for (rs2229080) and 56℃ for (rs714) respectively for 30 s, and extension at 72 °C for 30 s followed by final extension at 72 °C for 10 min. Five microliters of each PCR products were digested using 5U of the next restriction enzymes: NME1 rs34214448 (EcoRI) and rs2302254 (BanII) and for DCC rs2229080 and rs714 (MspI) (New England Biolabs, USA) according to the manufacturer’s instructions and finally separated in a 6% polyacrylamide gels. Genotypes was identified according to described by [17, 21, 26]. To ensure the quality of the genotyping processes, approximately 10% of the randomly samples were reprocessed, and the results were found to be 100% consistent.
Statistical analysis
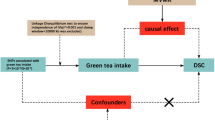
The T-student test was used to compare the means of age between patients and controls. Non-parametric Chi-square test was used to calculate the Hardy–Weinberg Equilibrium (HWE) of each variant and for demographic variables (age, sex, alcohol, and tobacco status) between the groups. Genotypic and allelic frequencies were calculated by direct counting for each group. Odds ratio (OR) and respective 95% confidence intervals (CI) analyses were used to associate genotypic and allelic frequencies with demographic and clinicopathological characteristics. A binary logistic regression analysis was performed to evaluate the confounding variables. The T-student, Chi-square, and Logistic regression tests were conducted using SPSS v.28.0 software (SPSS Inc., Chicago, IL, USA), while odds ratios and CIs were calculated using Epi Info. A significance level of P < 0.05 was considered statistically significant for the analyzed parameters. Additionally, the Bonferroni test was employed as an adjustment method to correct values (P < 0.0125).
Results
Demographic and clinical features of the study groups
The demographic, clinical, and anatomopathological information of CRC patients and healthy control subjects enrolled is presented in Table 1. The CRC group comprised 232 patients (134 male and 98 female), while the control group consisted of 232 healthy subjects (109 male and 123 female). All participants were efficiently genotyped for NME1 (rs34214448 G > T and rs2302254 C > T) and DCC (rs2229080 G > C and rs714 A > G) variants. The mean ages were 60.73 years (range 40 to 92) and 62.45 years (range 43 to 92) for the CRC and control group, respectively. Significant differences (P = 0.001) were observed in the smoking and drinking status between the two groups. Regarding clinical and pathological characteristics, 70.2% had stage III-IV tumors, 32.7% had metastases, and 53.45% had tumors located in the rectum.
NME1 and DCC variants in CRC patients and control subjects
In the control group, all four analyzed SNPs was found to be in Hardy–Weinberg Equilibrium (HWE) (p > 0.05). HWE for the NME1 rs34214448 and rs2302254 variants were X2 = 0.043 (P = 0.83) and X2 = 1.808 (P = 0.17), respectively. While the HWE for the DCC rs2229080 and rs714 variants were X2 = 1.887 (P = 0.16) and X2 = 1.048 (P = 0.30), respectively. Frequencies of the NME1 rs34214448 and DCC rs2229080 variants exhibited significant differences between CRC patients and control individuals (Table 2). The NME1 rs34214448 genotype G/T was observed in 62.07% (144/232) of the CRC patients and 44.83% (104/232) of the controls, indicating a statistically significant difference (OR = 2.68; 95% CI = 1.76–4.09, P = 0.001). Likewise, the genotype T/T was found in 15.9% (37/232) of the CRC patients and 12.5% (29/232) of the controls, indicating a statistically significant difference (OR = 2.47; 95% CI = 1.37–4.47, P = 0.001). When considering the dominant allelic interaction pattern of G/T + T/T versus G/G, the T allele demonstrated a statistically significant correlation with CRC (OR = 2.06; 95% CI = 1.38–3.07, P = 0.001). Furthermore, there were significant differences in allele frequencies between the groups; individuals carrying the T allele showed an elevated predisposition to CRC (OR = 1.65; 95% CI = 1.26–2.15, P = 0.001). Concerning to NME1 rs2302254 C > T variant no statistical significance was observed between the groups.
For the DCC rs2229080 G > C variant, significant differences were observed between patients versus control individuals for the G/C genotype (OR = 2.00; 95% CI = 1.28–3.11, p = 0.002). When considering a dominant pattern of allelic interaction (G/C + C/C vs. G/G), the C allele showed an association with CRC (OR = 1.94; 95% CI = 1.27–3.2, p = 0.002). Regarding to rs714 G > C variant in the DCC gene, no statistical significance was observed between the groups.
NME1 and DCC genotypes analysis by clinicopathological characteristics
The association between genotypes NME1 rs34214448 and rs2302254 and DCC rs2229080 and rs714 with clinicopathological characteristics are shown in Tables 3, 4, 5 and 6. Individuals over the age of 50 carrying the T/T and G/T genotypes of NME1 rs34214448 variant are more susceptible to developing CRC (OR = 2.99, 95% CI = 1.54–5.79, P = 0.001, and OR = 2.87, 95% CI = 1.81–4.54, P = 0.001 respectively). Women with the G/T genotype have a significantly higher risk of developing CRC (OR = 3.05, 95% CI = 1.59–5.81, P = 0.001). Furthermore, the dominant GT + TT vs G/G model indicates an increased susceptibility in women to develop CRC (OR = 2.94, 95% CI = 1.57–5.50, P = 0.001).
The analysis of disease development reveals that women in early TNM stages (I + II) who carry the G/T genotype are more susceptible to developing CRC (OR = 2.79, 95% CI = 1.26–4.80, P = 0.002). Based on tumor location analysis, individuals with the T/T genotype are more susceptible to developing tumors in the rectum (OR = 4.00; 95% CI = 2.00–8.01, P = 0.001) (see Table 3). We found statistical significance only in female patients carrying T/T genotype of NME1 rs2302254 variant (OR = 6.57; 95% CI = 3.14–13.76, P = 0.001). Regarding age, TNM stage, and tumor location no statistical association was observed (Table 4).
For the DCC rs2229080 variant, individuals over 50 carrying the G/C genotype demonstrated a higher susceptibility to develop CRC (OR = 2.50, 95% CI = 1.52–4.10, P = 0.001). This association was also observed with the dominant GC + CC vs G/G model of inherited disease (OR = 2.28, 95% CI = 1.40–3.72, P = 0.001). Patients in advanced TNM stages (III + IV) and carrying the G/C genotype exhibit greater susceptibility to developing CCR (OR = 2.54, 95% CI = 1.52–4.25, P = 0.001). No statistically significant differences were observed in the analysis of tumor location (Table 5). Furthermore, no statistical association was found for the DCC rs714 variant when comparing sex, age, TNM stage, and tumor location among groups (Table 6).
Multivariable logistic regression analysis with confounding variables
The results of the multiple logistic regression analysis are shown in Table 7 including confounding variables. Statistical significance was observed for tobacco and alcohol use in the presence of the two variants associated in NME1 (rs34214448) and DCC (rs2229080) (OR = 2.10; 95% CI = 1.30–3.37; P = 0.002 and OR = 2.06; 95% CI = 1.23–3.46; P = 0.006, respectively), suggesting that these variables increase the risk and susceptibility of developing CRC.
Discussion
Colorectal cancer is a complex disease influenced by multiple factors such as genetics, epigenetics, and environmental factors. Variants in two genes linked to CRC, NME1 (rs34214448 and rs2302254), and DCC (rs2229080 and rs7124), have been examined in various cancer types and populations, yielding inconsistent findings.
In this study conducted in the Mexican population, there is a clear increase in CRC incidence among individuals over the age of 50 (87.93%). This finding has been previously reported in other studies and aligns with global statistics [27, 28]. Significant statistical differences were observed between the groups in terms of tobacco and alcohol use. These results are consistent with those reported by Tsong et al. in 2007 and Minami et al. in 2022, which highlighted the important role that alcohol and tobacco consumption play in the development of colorectal carcinogenesis in the Chinese population, demonstrating that individuals who consume more than 7 alcoholic drinks a week present a high risk up to 72% over non-drinkers, similarly, it was observed that smokers present an increased risk of rectal cancer over non-smoking individuals [29, 30]. Yang LP et al. in 2021 found a significant increase among CRC patients who smoked, especially with left laterality, also associated with a longer duration and higher rate of smoking, with the risk being up to 55% higher in non-smokers [31]. In another study, Huang et al. in 2022, referred smoking is associated not only with the development of CRC, but also with a high risk of mortality in this entity, being 1.11 times higher than non-smoking patients. This risk was also present in patients who smoked more than 12 cigarettes per day or for more than 30 years [32]. In the study carried out by Botteri, it is also mentioned that the risk of CRC increases linearly with the intensity and duration of smoking and was also mainly associated with variants in BRAF and microsatellite instability rather than with variants in KRAS or TP53 [33].
The NME1 gene was the first identified metastasis suppressor gene. Low expression of NME1 has been linked to metastasis in various tumors, including melanoma, breast cancer, prostate cancer, and colorectal cancer. However, the mechanism responsible for this association is not fully understood [14, 34]. The most extensively studied variants within the promoter region of the NME1 gene are rs16949649 and rs2302254, which have been associated with low expression [35]. However, the rs34214448 variant, located in intron 1, has been implicated in possible modifications of post-transcriptional processes [35].
Analysis of genotypic and allelic frequencies for the NME1 rs34214448 G > T variant revealed significant differences (P = 0.001). The G/T and T/T genotypes were found to be significantly associated with an increased risk of CRC; this could confirm their role as a risk factor for CRC susceptibility.
Additionally, females over 50 years old showed an association with early TNM stages (I and II), and the rectum location was detected most frequently in these patients. These findings are the first reported among Mexican patients with CRC. However, Stremitzer S, et al. (2015) reported a similar association with recurrence-free survival (RFS) in patients with resected colorectal liver metastases [18]. Furthermore, our findings align with prior research on cervical neoplasia [14], lung cancer [35], breast cancer [21], and gastric cancer [15]. No significant differences were observed for the rs2302254 variant of the NME1 gene; however, it has been associated with other cancers [15, 36,37,38].
DCC is a transmembrane protein that belongs to the immunoglobulin superfamily. It has been identified as a potential tumor suppressor gene located on chromosome 18q21. DCC is expressed in normal tissues as colonic mucosa, however, in CRC samples analyzed the protein has been missing. DCC plays an essential role in directing cell invasion through the basement membrane, making it a crucial component in the pathological progression of human cancer [19, 39].
DCC deletions have been found in 20–75% of CRC, and gene alterations are linked to cancer and metastasis [39]. The most extensively studied DCC variants are rs714, rs4078288, and rs7504990, which are situated in an intronic region and could affect expression levels. Meanwhile, the rs2229080 variant is a missense mutation found in exon 3 that replaces Arg (CGA) to Gly (GGA), at codon 201 of DCC protein [9]. This variation has been linked to decreased expression regulation and has been clinically associated with advanced cancer stages, a poor prognosis, and increased susceptibility to CRC [19, 40]. Bakshi et al. have reported that the presence of the C allele is a protective factor in breast cancer and found that the ribonucleic acid (RNA) secondary structure of wild-type alleles enhances their stability [9].
Significant differences were observed between groups regarding the rs2229080 G > C variant. The G/C genotype was found to be significantly associated with an increased risk of developing colorectal cancer, indicating that it is a genetic factor for susceptibility to CRC. Additionally, we have identified a significant correlation between male patients over 50 years old and those with an advanced TNM stage (III + IV). These results are consistent with those reported by Sharma et al., 2021 in patients with CRC [24], as well as breast and gallbladder cancer [39]. On the other hand, no association has been observed for the rs2229080 variant with esophageal and gastric cancer [19]. However, in two studies, the C allele has been reported as a protective factor against breast cancer [9, 39].
In relation to the DCC rs714 variant, no significant association was detected in the present study with any demographic and clinicopathological variables. However, in a few reports a positive association has been observed. For instance, Malik et al. found an association with esophageal and gastric cancer [17], and Rai et al. reported an association with gallbladder cancer [40].
Finally, the multivariable analysis showed, for the first time, that tobacco and alcohol consumption are a risk factor for CRC in carriers of the G/T or T/T genotypes of the rs34214448 NME1 variant, and G/C or C/C genotypes of the rs2229080 DCC variant. Potentially modifiable lifestyle factors, such as tobacco and alcohol consumption, have been associated with CRC risk in studies conducted in Western populations [41].
Further studies with larger sample sizes, functional genomics and analysis in other populations are needed to validate the genetic effects of NME1 and DCC polymorphisms in CRC. A limitation of this study was the absence of Body Mass Index (BMI) and follow-up data in these patients. In the future, more studies concerning to the association between other SNPs in the NME1 and DCC genes and the risk of CRC are required.
Conclusions
In conclusion, this study represents the first to identify the NME1 rs34214448 and DCC rs2229080 variants as potential markers for CRC risk. Additionally, these polymorphic variants were found to be associated with age, sex, TNM stages, and tumor localization.
Availability of data and materials
The datasets used during the present study are available from the corresponding author upon request.
Abbreviations
- CRC:
-
Colorectal cancer
- PCR–RFLP:
-
Polymerase chain reaction-restriction fragment length polymorphism
- OR:
-
Odds ratio
- DNA:
-
Deoxyribonucleic acid
- LOH:
-
Loss of heterozygosity
- IMSS:
-
Mexican Social Security Institute
- TNM:
-
Tumor-Nodule-Metastasis
- HWE:
-
Hardy–Weinberg Equilibrium
- CI:
-
Confidence intervals
- RNA:
-
Ribonucleic acid
References
Ferlay J EM, Lam F, Laversanne M, Colombet M, Mery L, Piñeros M, Znaor A, Soerjomataram I, Bray F. Global Cancer Observatory: Cancer Today. Lyon, France: International Agency for Research on Cancer. 2024. https://gco.iarc.who.int/today. Accessed 22 Feb 2024
Balmain A, Gray J, Ponder B. The genetics and genomics of cancer. Nat Genet. 2003;33(Suppl):238–44. https://doi.org/10.1038/ng1107.
Ouatas T, Salerno M, Palmieri D, Steeg PS. Basic and translational advances in cancer metastasis: Nm23. J Bioenerg Biomembr. 2003;35(1):73–9. https://doi.org/10.1023/a:1023497924277.
Takayama T, Miyanishi K, Hayashi T, Sato Y, Niitsu Y. Colorectal cancer: genetics of development and metastasis. J Gastroenterol. 2006;41(3):185–92. https://doi.org/10.1007/s00535-006-1801-6.
Han W, Shi CT, Cao FY, Cao F, Chen MB, Lu RZ, Wang HB, Yu M, He DW, Wang QH, Wang JF, Xu XX, Ding HZ. Prognostic Value of NME1 (NM23-H1) in patients with digestive system neoplasms: a systematic review and meta-analysis. PLoS ONE. 2016;11(8): e0160547. https://doi.org/10.1371/journal.pone.0160547.
Jensen SL, Wood DP Jr, Banks ER, Veron M, Lascu I, McRoberts JW, Rangnekar VM. Increased levels of nm23 H1/nucleoside diphosphate kinase A mRNA associated with adenocarcinoma of the prostate. World J Urol. 1996;14(Suppl 1):S21-25. https://doi.org/10.1007/BF00182060.
Khan MH, Yasuda M, Higashino F, Haque S, Kohgo T, Nakamura M, Shindoh M. nm23-H1 suppresses invasion of oral squamous cell carcinoma-derived cell lines without modifying matrix metalloproteinase-2 and matrix metalloproteinase-9 expression. Am J Pathol. 2001;158(5):1785–91. https://doi.org/10.1016/S0002-9440(10)64134-X.
Banerjee S, Jha HC, Robertson ES. Regulation of the metastasis suppressor Nm23-H1 by tumor viruses. Naunyn Schmiedebergs Arch Pharmacol. 2015;388(2):207–24. https://doi.org/10.1007/s00210-014-1043-8.
Bakshi D, Nagpal A, Sharma V, Sharma I, Shah R, Sharma B, Bhat A, Verma S, Bhat GR, Abrol D, Sharma R, Vaishnavi S, Kumar R. MassARRAY-based single nucleotide polymorphism analysis in breast cancer of north Indian population. BMC Cancer. 2020;20(1):861. https://doi.org/10.1186/s12885-020-07361-8.
Saito M, Yamaguchi A, Goi T, Tsuchiyama T, Nakagawara G, Urano T, Shiku H, Furukawa K. Expression of DCC protein in colorectal tumors and its relationship to tumor progression and metastasis. Oncology. 1999;56(2):134–41. https://doi.org/10.1159/000011954.
Luo L, Shen GQ, Stiffler KA, Wang QK, Pretlow TG, Pretlow TP. Loss of heterozygosity in human aberrant crypt foci (ACF), a putative precursor of colon cancer. Carcinogenesis. 2006;27(6):1153–9. https://doi.org/10.1093/carcin/bgi354.
Akkiprik M, Ataizi-Celikel C, Dusunceli F, Sonmez O, Gulluoglu BM, Sav A, Ozer A. Clinical significance of p53, K-ras and DCC gene alterations in the stage I-II colorectal cancers. J Gastrointestin Liver Dis. 2007;16(1):11–7.
Toma M, Cimponeriu D, Apostol P, Stavarachi M, Cojocaru M, Belusica L, Craciun AM, Radu I, Gavrila L. Lack of association between ACE ID polymorphism and colorectal cancer in Romanian patients. Chirurgia (Bucur). 2009;104(5):553–6.
Feng CY, Wang PH, Tsai HT, Tee YT, Ko JL, Chen SC, Lin CY, Han CP, Yang JS, Liu YF, Lin LY, Yang SF. Polymorphisms of Human Nonmetastatic Clone 23 Type 1 Gene and Neoplastic Lesions of Uterine Cervix. Reprod Sci. 2010;17(10):886–93. https://doi.org/10.1177/1933719110373661.
Li AL, Zhou X, Wang ZN, Song YX, Gao P, Miao Y, Zhu JL, Xu HM. Associations of non-metastatic cells 1 gene polymorphisms with lymph node metastasis risk of gastric cancer in Northern Chinese population. Tumour Biol. 2012;33(6):2159–66. https://doi.org/10.1007/s13277-012-0476-2.
Li Y, Kang S, Qin JJ, Wang N, Zhou RM, Sun HY. nm23 gene polymorphisms are associated with survival of patients with epithelial ovarian cancer but not with susceptibility to disease. Gynecol Oncol. 2012;126(3):455–9. https://doi.org/10.1016/j.ygyno.2012.06.004.
Malik MA, Gupta A, Zargar SA, Mittal B. Role of genetic variants of deleted in colorectal carcinoma (DCC) polymorphisms and esophageal and gastric cancers risk in Kashmir Valley and meta-analysis. Tumour Biol. 2013;34(5):3049–57. https://doi.org/10.1007/s13277-013-0870-4.
Stremitzer S, Zhang W, Yang D, Ning Y, Stintzing S, Sunakawa Y, Sebio A, Yamauchi S, Matsusaka S, Parekh A, Barzi A, El-Khoueiry R, Stift J, Wrba F, Gruenberger T, Lenz HJ. Variations in genes involved in dormancy associated with outcome in patients with resected colorectal liver metastases. Ann Oncol. 2015;26(8):1728–33. https://doi.org/10.1093/annonc/mdv224.
Liu X, Wang X, Fu SW, Wang M, Kang H, Guan H, Zhang S, Ma X, Lin S, Liu K, Feng Y, Dai C, Dai Z. Genetic association of deleted in colorectal carcinoma variants with breast cancer risk: A case-control study. Oncotarget. 2016;7(22):32765–73. https://doi.org/10.18632/oncotarget.9024.
Zhu KW, Chen P, Zhang DY, Yan H, Liu H, Cen LN, Liu YL, Cao S, Zhou G, Zeng H, Chen SP, Zhao XL, Chen XP. Association of genetic polymorphisms in genes involved in Ara-C and dNTP metabolism pathway with chemosensitivity and prognosis of adult acute myeloid leukemia (AML). J Transl Med. 2018;16(1):90. https://doi.org/10.1186/s12967-018-1463-1.
Antar S, Mokhtar N, Abd Elghaffar MA, Seleem AK. Association of polymorphisms in metastasis suppressor genes NME1 and KISS1 with breast cancer development and metastasis. J Egypt Natl Canc Inst. 2020;32(1):24. https://doi.org/10.1186/s43046-020-00037-1.
Malik MA, Malik SA, Haq MG, Bangri SA, Ahmad SZ, Shah OJ, Shah ZA. Genetic Susceptibility of DCC Gene in Gallbladder Cancer in Kashmir and Meta-Analysis. Nutr Cancer. 2022;74(3):947–55. https://doi.org/10.1080/01635581.2021.1949728.
Rubio SA, Martinez SE, Corona JS, Ruiz AP, Rincon AE, Lagunas IA, Camacho JG, Moguel MC. EcoRI polymorphism of the metastasis-suppressor gene NME1 in Mexican patients with breast cancer. Breast Cancer Res Treat. 2006;96(2):159–61. https://doi.org/10.1007/s10549-005-9072-0.
Sharma B, Angurana S, Bhat A, Verma S, Bakshi D, Bhat GR, Jamwal RS, Amin A, Qadri RA, Shah R, Kumar R. Genetic analysis of colorectal carcinoma using high throughput single nucleotide polymorphism genotyping technique within the population of Jammu and Kashmir. Mol Biol Rep. 2021;48(8):5889–95. https://doi.org/10.1007/s11033-021-06583-8.
Miller SA, Dykes DD, Polesky HF. A simple salting out procedure for extracting DNA from human nucleated cells. Nucleic Acids Res. 1988;16(3):1215. https://doi.org/10.1093/nar/16.3.1215.
Huang XI, Zhao W, Li Y, Kang S. Association between nm23 gene polymorphisms and the risk of endometriosis. Biomed Rep. 2015;3(6):874–8. https://doi.org/10.3892/br.2015.511.
Siegel R, Desantis C. Jemal A (2014) Colorectal cancer statistics. CA Cancer J Clin. 2014;64(2):104–17. https://doi.org/10.3322/caac.21220.
Radanova M, Levkova M, Mihaylova G, Manev R, Maneva M, Hadgiev R, Conev N, Donev I. Single Nucleotide Polymorphisms in microRNA Genes and Colorectal Cancer Risk and Prognosis. Biomedicines. 2022;10(1). https://doi.org/10.3390/biomedicines10010156
Tsong WH, Koh WP, Yuan JM, Wang R, Sun CL, Yu MC. Cigarettes and alcohol in relation to colorectal cancer: the Singapore Chinese Health Study. Br J Cancer. 2007;96(5):821–7. https://doi.org/10.1038/sj.bjc.6603623.
Minami Y, Kanemura S, Kusaka J, Kinouchi M, Suzuki S, Nishino Y, Miura K. Associations of cigarette smoking, alcohol drinking and body mass index with survival after colorectal cancer diagnosis by anatomic subsite: a prospective patient cohort study in Japan. Jpn J Clin Oncol. 2022;52(12):1375–88. https://doi.org/10.1093/jjco/hyac140.
Yang LP, Wang ZX, Zhang R, Zhou N, Wang AM, Liang W, Wang ZQ, Luo HY, Wang F, Liu JW, Liu F, Zhang XC, Liu YP, Jin Y. Association between cigarette smoking and colorectal cancer sidedness: A multi-center big-data platform-based analysis. J Transl Med. 2021;19(1):150. https://doi.org/10.1186/s12967-021-02815-4.
Huang YM, Wei PL, Ho CH, Yeh CC. Cigarette Smoking Associated with Colorectal Cancer Survival: A Nationwide, Population-Based Cohort Study. J Clin Med. 2022;11(4).https://doi.org/10.3390/jcm11040913
Botteri E, Borroni E, Sloan EK, Bagnardi V, Bosetti C, Peveri G, Santucci C, Specchia C, van den Brandt P, Gallus S, Lugo A. Smoking and colorectal cancer risk, overall and by molecular subtypes: a meta-analysis. Am J Gastroenterol. 2020;115(12):1940–9. https://doi.org/10.14309/ajg.0000000000000803.
Antar S, Mokhtar N, Abd Elghaffar MA, Seleem AK. Association of polymorphisms in metastasis suppressor genes NME1 and KISS1 with breast cancer development and metastasis. J Egypt Natl Cancer Institute. 2020;32(1). https://doi.org/10.1186/s43046-020-00037-1
Shi XQ, Jin HF, Peng ML, Li BJ, She MC, Zhu T, Wen S, Qin DC. Association between NMEI polymorphisms and cancer susceptibility: A meta-analysis based on 1644 cases and 2038 controls. Pathol Res Pract. 2018;214(4):467–74. https://doi.org/10.1016/j.prp.2018.02.020.
Qu S, Long J, Cai Q, Shu XO, Cai H, Gao YT, Zheng W. Genetic polymorphisms of metastasis suppressor gene NME1 and breast cancer survival. Clin Cancer Res. 2008;14(15):4787–93. https://doi.org/10.1158/1078-0432.CCR-08-0083.
Wang PH, Yi YC, Tsai HT, Tee YT, Ko JL, Han CP, Liu YF, Lin LY, Yang SF. Significant association of genetic polymorphism of human nonmetastatic clone 23 type 1 gene with an increased risk of endometrial cancer. Gynecol Oncol. 2010;119(1):70–5. https://doi.org/10.1016/j.ygyno.2010.06.013.
Braunagel D, Schaich M, Kramer M, Dransfeld CL, Ehninger G, Mahlknecht U. The T_T genotype within the NME1 promoter single nucleotide polymorphism -835 C/T is associated with an increased risk of cytarabine induced neurotoxicity in patients with acute myeloid leukemia. Leuk Lymphoma. 2012;53(5):952–7. https://doi.org/10.3109/10428194.2011.635862.
Rai R, Sharma KL, Tiwari S, Misra S, Kumar A, Mittal B (2013) DCC (deleted in colorectal carcinoma) gene variants confer increased susceptibility to gallbladder cancer (Ref. No.: Gene-D-12–01446). Gene 518 (2):303–309. https://doi.org/10.1016/j.gene.2013.01.019
Minami R, Aoyama N, Honsako Y, Kasuga M, Fujimori T, Maeda S. Codon 201Arg/Gly polymorphism of DCC (deleted in colorectal carcinoma) gene in flat- and polypoid-type colorectal tumors. Dig Dis Sci. 1997;42(12):2446–52. https://doi.org/10.1023/a:1018839907159.
Cho S, Shin A. Population Attributable Fraction of Established Modifiable Risk Factors on Colorectal Cancer in Korea. Cancer Res Treat. 2021;53(2):480–6. https://doi.org/10.4143/crt.2019.742.
Acknowledgements
This study was supported by Grants from “Fondo de Investigación en Salud. Instituto Mexicano del Seguro Social” (FIS/IMSS/PROT/G18/1822 and (FIS/IMSS/PROT/PRIO/19/118).
Funding
This research was supported by Grants from “Fondo de Investigación en Salud. Instituto Mexicano del Seguro Social” (FIS/IMSS/PROT/G18/1822 and (FIS/IMSS/PROT/PRIO/19/118).
Author information
Authors and Affiliations
Contributions
MARR, PBN and MPGA designed the study; RMMG, AMSS, CJTJ, TDPR, AAAW, MEMC and IMR collected the samples and clinicopathological data; RMMG, AMSS and MARR experiments conducted and the data analysis; RMMG, AMSS, CJTV, PBN, MPGA, MHOG, IMR, TDPR, AAAW, MEMC and MARR have contributed to the writing of the manuscript; and all authors share and approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval for this study was obtained from the Scientific Research Committee of the Mexican Social Security Institute (IMSS) and was approved with the register number: R-2018–1305-001. Informed written consent to participate in the study was provided by all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Márquez-González, R.M., Saucedo-Sariñana, A.M., de Jesús Tovar-Jacome, C. et al. NME1 and DCC variants are associated with susceptibility and tumor characteristics in Mexican patients with colorectal cancer. J Egypt Natl Canc Inst 36, 10 (2024). https://doi.org/10.1186/s43046-024-00213-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43046-024-00213-7