Abstract
Introduction
Brain metastases (BM) are associated with dismal prognosis as they cause significant morbidity and affect the quality of life of patients. Management of BM depends on the following factors: age, patient performance, size and the number of lesions, location of the tumor, comorbidities, primary tumor type, and extracranial disease burden. In the present study, the pattern of occurrence, clinical characteristics, treatment outcome of brain metastases, and factors, tumor characteristics, and treatment that may impact BM patients’ overall survival were analyzed.
Methods
Retrospective analysis of medical records of 116 patients with histologically proven primary site solid tumors with brain metastases was done in the present study. Clinicoradiological and pathological parameters were documented. The relationship between variables and outcome was assessed by univariate analysis using the Cox proportional regression model to reach a significance of p < 0.05, to determine independent predictors of overall survival.
Results
One hundred sixteen patients of BM from various solid malignancies were included. Age ranged from 18 to 81 years (median 53.5). One hundred four patients received WBRT with a dose range of 8–40Gy/1–15fr, 7 received SRS with a dose of 18–24Gy depending on the size of the metastatic lesion, and 2 received SRT 27–33Gy/3fr. At the time of final analysis, 47 patients with BM had expired, 60 were lost to follow-up, and 9 were alive. Median survival was 8.25 (0.5–32.5 months) months. Female gender (χ2 = 8.423; p = 0.015), RPA I (χ2 = 9.353; p = 0.05), and metachronous BM (χ2 = 3.793; p = 0.03) were associated with better survival. Patients with age 41–50 years, adenocarcinoma lung histology, and supratentorial location survived more than 2 years but did not show any statistical significance.
Conclusion
Brain metastases portend a very dismal prognosis. Certain clinicoradiological and pathologic factors have been identified to affect survival. More prospective multicentric trials, with a larger sample size, need to be conducted to assess the benefit of radiation in patients with limited life expectancy and identify prognostic and predictive factors for survival.
Similar content being viewed by others
Introduction
Brain metastases (BM) are the most common intracranial malignancy and ten times more common than primary brain tumors [1]. Lung primary is most commonly associated with the occurrence of brain metastases (40–50%), followed by breast (15–30%), melanoma (5–20%), colorectal cancer (CRC) (3–8%), and renal cell cancer (2–4%) [2]. Small cell lung cancer and adenocarcinoma are the common histologies in lung cancer associated with BM. Brain metastases are associated with dismal prognosis as they cause significant morbidity and affect the quality of life of patients [3]. Management of BM depends on the following factors: age, patient performance, size and the number of lesions, location of tumor, comorbidities, primary tumor type, and extracranial disease burden. Commonly used treatment modalities include surgery, whole brain radiotherapy (WBRT), stereotactic surgery (SRS) and radiotherapy, chemotherapy, and targeted therapies [4]. Quality of life of patients and the long-term toxicity and management complications should also be carefully balanced when deciding on the treatment of BM patients. WBRT is associated with an increment in intracranial tumor control rates but with long-term neurocognitive decrement, and without improvement in overall survival, SRS is usually considered in patients with a limited number of BM [5, 6].
The literature is sparse on the factors that may affect survival in patients with brain metastases. We conducted a single-center retrospective study to assess the pattern of occurrence, clinical characteristics, and management outcome of brain metastases and also identified clinical factors, tumor characteristics, and treatment that may impact BM patients’ overall survival.
Methods
Patient selection
We retrospectively analyzed medical records of a total of 116 patients of solid tumors with brain metastases who received treatment between Jan 2018 and March 2021. Patients with a histologically proven primary site (solid tumors) with brain metastases were included. Patients who had leptomeningeal metastases and hematological malignancies were excluded. Approval was taken from the Institutional Ethics committee. Diagnosis of brain metastases was made on the basis of the following criteria: imaging evidence of intracranial metastases or pathological confirmation of a metastatic brain tumor.
Study variables
Parameters documented were age, gender, primary site, stage, primary tumor type, date of diagnosis of brain metastases, synchronous/metachronous, and clinical presentation of BM; the number of lesions; location, number of extracranial metastases, RPA-I:KPS ≥70%, age <65 years, controlled primary site, and no extracranial metastases; RPA-II: all others; RPA-III:KPS < 70; surgery for metastases: yes/no; radiotherapy technique, dose, time after brain metastases (in months); and status of the patient at the time of analysis.
Outcome
The primary outcome assessed was overall survival defined as the time interval between BM diagnosis and death from any cause. The secondary outcome assessed was clinical factors, tumor characteristics, and treatment that may impact the overall survival of BM patients.
Statistical analysis
The method of analysis of all subjects was intention-to-treat analysis. Relationships between categorical variables were analyzed using Fisher’s exact test, while continuous data was analyzed using the Mann–Whitney U test. The relationship between variables and outcome was assessed by univariate analysis using the Cox proportional regression model to reach a significance of p < 0.05, to determine independent predictors of overall survival. Overall survival and median survival were calculated. Patients who were lost to follow-up were excluded from the survival analysis.
Results
Patient characteristics
In the present study, 116 patients of BM from various solid malignancies were included during the study period. Age ranged from 18 to 81 years (median 53.5). The most common age group was 41–50 years with 38 patients. Male to female ratio was 1.57. Lung cancer was the most common primary malignancy 80 (68.9%) with 35% being adenocarcinoma histology followed by breast cancer 23 (19.8%) patients. Thirty-one (26.7%) patients had bone metastases. The most common presenting symptom was headache in 64 patients, and 7 had an incidental diagnosis of brain metastases, in whom brain MRI was done as part of staging workup for advanced malignancy. Out of seven patients with asymptomatic BM, six were of lung cancer (SCLC and NSCLC) and one breast cancer. According to RPA classification, 51, 15, and 50 patients were of I, II, and III respectively. Multiple lobes of the brain were involved in 51.7% of patients. The time to diagnosis of BM was more than 6 months (metachronous) from primary malignancy in 73 patients whereas 43 patients had synchronous BM. The median follow-up time was 6 months (Table 1).
Treatment and outcome
Patients with synchronous BM were treated with radiation therapy followed by systemic chemotherapy depending on the performance status of the patient. None of the patients had undergone surgery prior to radiation. One hundred four patients received WBRT with a dose range of 8–40Gy/1–15fr, 7 received SRS with a dose of 18–24Gy depending on the size of the metastatic lesion, and 2 received SRT 27–33Gy/3fr. At the time of the final analysis, 47 patients with BM had expired, 60 were lost to follow-up, and 9 were alive (Table 2).
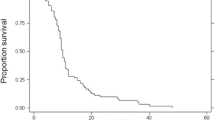
A large number of patients being lost to follow-up might be due to the COVID-19 situation prevailing for the last 2 years. The cause of death included disease progression and aspiration pneumonia. Twenty-two patients survived for less than 6 months whereas 16 for more than 1 year. Median survival was 8.25 (0.5–32.5 months) months (Fig. 1).
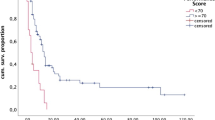
Overall median survival was high in age more than 50 years (32 months), in male (28 months) adenocarcinoma histology in lung cancer (32 months), and in KPS scores more than 70 (32 months) (Fig. 2a–d).
Factors affecting survival
Correlation of variables was done with survival data, and female gender (χ2 = 8.423; p = 0.015), RPA I (χ2 = 9.353; p = 0.05), and metachronous BM (χ2 = 3.793; p = 0.03) were associated with better survival. Patients with age 41–50 years (4), adenocarcinoma histology (4), multiple brain metastases (7), and supratentorial location (4) survived more than 2 years and did not show any statistical significance (Table 3).
Discussion
Brain metastases are the most common intracranial neoplasms and occur in 15–40% of patients with systemic cancer [7]. Incidence is on the rise in the last 20 years because of the upsurge in primary malignancies, e.g., lung and breast cancer, and newer therapeutic modalities increasing survival and imaging modalities which can identify brain metastases [8]. The more common age of BM occurrence is the 5th to 7th decade. Similarly, in the present study, the median age was 53 years with 57.7% of patients being more than 50 years of age. BM are common in the lung (36–64%), breast (15–25%), and melanoma (5–20%) followed by less common colorectum, genitourinary malignancies [9, 10]. In the present study also, lung cancer was the most common primary malignancy in 68.9% of patients with 35% being adenocarcinoma histology followed by breast cancer in 19.8% of patients. BM are primarily diagnosed as metachronous, and less common synchronous (30%), and in few patients, BM may be the presenting symptom in occult cancer (10%). In the present study, 62.9% of patients had metachronous BM presentation [11].
The common symptoms of BM include headache, vomiting, seizures, and weakness which are due to mass effect, edema, and raised intracranial pressure. In this study, 55.3% of patients presented with headache followed by seizures and weakness whereas 6% did not have any symptoms pertaining to BM.
The decision regarding treatment is usually done on the basis of the recursive partition analysis (RPA) prognostic scale which was developed by Gaspar et al. in 1977 [12]. This is based on four prognostic factors: performance according to the Karnofsky Performance Scale (KPS), control of the primary disease, presence or absence of extracranial disease, and age greater or less than 65 years. Patients are divided into three classes I, II, and III with an estimated survival of 7.1, 4.2, and 2.3 months respectively. Patients with RPA I and II are considered for surgery or radiation of BM whereas class III is usually considered for supportive care. In this study, 43.9% of patients were of RPA class I and 43.1% were class III. Also, at the time of analysis, 7 patients in class I and 2 patients in class III were alive, suggesting other factors might also be associated with increased survival in some patients. Though the prognostic scale suggests survival, also, there is disease-specific graded prognostic assessment (DS-GPA) in which other prognostic factors specific to each malignancy are considered, e.g., molecular subtype in breast cancer and the number of metastases in the lung, renal carcinoma, and melanoma [13, 14].
Management strategies for BM include surgery, whole brain radiotherapy (WBRT), stereotactic surgery (SRS), and stereotactic radiotherapy (SRT) [15]. Dose for WBRT varies from 30Gy in 2 weeks to 20Gy in 1 week without any difference in symptom control and overall survival in the two fractionations [16]. 89.6% of patients in this study received WBRT, with the most common fractionation being 20Gy in 5 fractions because 74.2% of patients had multiple metastases. There was no immediate toxicity due to this dose fractionation but a longer neurological assessment is required to identify any effect on neurocognitive function. Only 6% and 1.8% of patients received SRS and SRT respectively.
Patients with good performance status, a limited number of brain lesions, and controlled extracranial primary should be considered for SRS and have shown 80–90% local control with symptom improvement and median survival of 6–12 months [17]. The median survival in the present study was 8.25 months. Ekici et al. in their study of BM had a median survival of 6.7 months. They also identified patients with KPS ≥ 70, with single BM, with extracranial primary controlled, and without leptomeningeal metastases [18].
Similarly, in the present study, patients with RPA I class survived more than II and III, but there was no correlation in patients with number of brain lesions, extracranial primary status, or disease burden elsewhere and survival. Lock et al. assessed whether patients with shorter expected survival would benefit from WBRT and concluded that poor performance status and the extent of metastatic burden could be a predictor of early death in patients with BM [19]. Similarly, in the present study, patients with synchronous BM, RPA-II, and male gender had poor survival, but there was no difference on OS depending on the WBRT dose. Rastogi et al. identified that female gender, performance status, breast primary, metachronous BM, solitary lesion, and controlled primary were associated with better survival in BM [20]. In the present study, results regarding factors affecting survival in BM also showed a similar trend as mentioned in previous studies but some did not show any statistical significance.
The limitations of the present study being disease-specific graded prognostic assessment for each disease site could have revealed more factors affecting survival. A large number of patients were lost to follow-up due to the COVID-19 situation at the time of analysis, which might have affected our results. But more prospective multicentric trials, with a larger sample size, need to be conducted to assess the benefit of radiation in patients with limited life expectancy and identify prognostic and predictive factors for survival.
Conclusion
Brain metastases portend a very dismal prognosis. WBRT remains the cornerstone of the management of multiple brain metastases, whereas for solitary lesion, surgical excision followed by SRS or SRT is the preferred treatment modality. The performance status of the patient with extracranial disease burden plays an important role in decision-making. In the present study, female gender, RPA I class, and metachronous brain metastases were identified as factors affecting the overall survival of BM patients. Also, patients with age 41–50 years, adenocarcinoma histology, and supratentorial location of tumors survived longer though the results were not statistically significant.
Availability of data and materials
The data that support the findings of this study are available on request from the corresponding author.
Abbreviations
- BM:
-
Brain metastases
- CRC:
-
Colorectal cancer
- WBRT:
-
Whole brain radiotherapy
- RPA:
-
Recursive partitioning analysis
- SRS:
-
Stereotactic surgery
- SRT:
-
Stereotactic radiotherapy
- KPS:
-
Karnofsky Performance Status
- SCLC:
-
Small cell lung cancer
- NSCLC:
-
Nonsmall cell lung cancer
- DS-GPA:
-
Disease-specific graded prognostic assessment DS-GPA
References
Nayak L, Lee EQ, Wen PY. Epidemiology of brain metastases. Curr Oncol Rep. 2012;14(1):48–54.
Achrol AS, Rennert RC, Anders C, et al. Brain metastases. Nat Rev Dis Primers. 2019;5(1):5-018-0055-y.
Quigley MR, Fukui O, Chew B, Bhatia S, Karlovits S. The shifting landscape of metastatic breast cancer to the CNS. Neurosurg Rev. 2013;36(3):377e82.
Kocher M, Soffietti R, Abacioglu U, Villà S, Fauchon F, Baumert BG, et al. Adjuvant whole-brain radiotherapy versus observation after radiosurgery or surgical resection of one to three cerebral metastases: results of the EORTC 22952-26001 study. J Clin Oncol. 2011;29(2):134–41.
Brown PD, Jaeckle K, Ballman KV, et al. Effect of radiosurgery alone vs radiosurgery with whole brain radiation therapy on cognitive function in patients with 1 to 3 brain metastases a randomized clinical trial. JAMA J Am Med Assoc. 2016;316(4):401e9.
Mainwaring W, Bowers J, Pham N, Pezzi T, Shukla M, Bonnen M, Ludwig M. Stereotactic Radiosurgery Versus Whole Brain Radiation Therapy: A Propensity Score Analysis and Predictors of Care for Patients With Brain Metastases From Breast Cancer. Clin Breast Cancer. 2019;19(2):e343-e351.
Delattre JY, Krol G, Thaler HT, et al. Distribution of brain metastases. Arch Neurol. 1988;45:741–4.
Schouten LJ, Rutten J, Huveneers HA, Twijnstra A. Incidence of brain metastases in a cohort of patients with carcinoma of the breast, colon, kidney, and lung and melanoma. Cancer. 2002;94:2698–705.
Taillibert S, Le Rhun É. Epidemiology of brain metastases. Cancer Radiother. 2015;19(1):3–9.
Gavrilovic IT, Posner JB. Brain metastases: epidemiology and pathophysiology. J Neuro-Oncol. 2005;75:5–14.
Kralik SF, Kamer AP, Ho CY. Diagnostic imaging of intracranial metastasis. Curr Probl Cancer. 2015;39(2):99–112.
Gaspar L, Scott C, Rotman M, Asbell S, Phillips T, et al. Recursive partitioning analysis (RPA) of prognostic factors in three radiation therapy oncology group (RTOG) brain metastases trials. Int J Radiat Oncol Biol Phys. 1997;37:745–51.
Villà S, Weber DC, Moretones C, Mañes A, Combescure C, et al. Validation of the new graded prognostic assessment scale for brain metastases: a multicenter prospective study. Radiat Oncol. 2011;6:23.
Sperduto PW, Kased N, Roberge D, Xu Z, Shanley R, et al. Summary report on the graded prognostic assessment: an accurate and facile diagnosis-specific tool to estimate survival for patients with brain metastases. J Clin Oncol. 2012;30:419–25.
Tsao MN, Rades D, Wirth A, Lo SS, Danielson BL, et al. Radiotherapeutic and surgical management for newly diagnosed brain metastases: an American Society for Radiation Oncology evidence based guideline. Prac Radiat Oncol. 2012;2:210–25.
Borgelt B, Gelber R, Kramer S, Brady LW, Chang CH, et al. The palliation of brain metastases: final results of the first two studies by the radiation therapy oncology group. Int J Radiat Oncol Biol Phys. 1980;6:1–9.
Lippitz B, Lindquist C, Paddick I, et al. Stereotactic radiosurgery in the treatment of brain metastases: the current evidence. Cancer Treat Rev. 2014;40(1):48–59.
Ekici K, Temelli O, Dikilitas M, Halil Dursun I, Bozdag Kaplan N, Kekilli E. Survival and prognostic factors in patients with brain metastasis: single center experience. J Buon. 2016;21(4):958–63.
Lock M, Chow E, Pond GR, Do V, Danjoux C, Dinniwell R, et al. Prognostic factors in brain metastases: can we determine patients who do not benefit from whole-brain radiotherapy? Clin Oncol (R Coll Radiol). 2004;16(5):332–8.
Rastogi K, Bhaskar S, Gupta S, Jain S, Singh D, Kumar P. Palliation of brain metastases: analysis of prognostic factors affecting overall survival. Indian J Palliat Care. 2018;24(3):308–12.
Acknowledgements
None.
Financial support and sponsorship
Nil.
Funding
None.
Author information
Authors and Affiliations
Contributions
SG—conceptualization of the study; SS—data collection; AC—data collection; SN—literature review; RA—data collection; KK—data analysis; DJ—compilation of data; RA—patient data review and editing the manuscript; AG—editing the manuscript; MG—literature review and editing the manuscript. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All India Institute of Medical Sciences, Rishikesh IEC has approved the study on 16/07/2021. IEC approval letter no: AIIMS/IEC/21/401. We obtain patient consent about the possible use of their data in the future studies and research.
Consent for publication
We obtain patient consent about the possible use of their data in the future studies, research, and publication.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gupta, S., Singh, S., Chophy, A. et al. Analysis of prognostic factors in patients with brain metastases affecting survival. J Egypt Natl Canc Inst 34, 45 (2022). https://doi.org/10.1186/s43046-022-00146-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43046-022-00146-z