Abstract
Background
Thyroid cancer is one of the common cancers that, depending on the need for treatment, patients are treated with radioactive iodine after thyroidectomy surgery. The purpose of this study is to investigate the effect of iodine therapy on the ovarian reserve of women at reproductive ages.
Methods
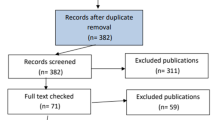
In this prospective study, 60 patients with thyroid cancer aged 18 to 35 who were undergoing iodine therapy for the first time in 2018–2019 were included in the study. Patients with underlying diseases and any ovarian disorders and patients who needed repeated iodine treatment were excluded from the study. Anti-Müllerian hormone (AMH) level of patients was evaluated 4 times before, 3, 6, and 12 months after iodine therapy. The significance level of the P-value study was considered less than 0.05.
Results
The average age of the patients was 29.53 ± 4.53 years. With aging, AMH level decreases significantly. No significant correlation was observed between smoking, menarche age, and abnormal uterine bleeding with AMH level. The average AMH before, 3, 6, and 12 months after iodine therapy was 2.25 ± 0.55 ng/ml, 1.15 ± 0.35 ng/ml, 1.58 ± 0.47 ng/ml, and 1.94 ± 0.58 ng/ml, which has a significant decrease respectively 49.05%, 29.55%, and 13.58% compared to the amount before iodine therapy (P-value < 0.001).
Conclusion
Considering the effect of iodine therapy on the reduction of AMH levels, it is recommended that women of reproductive age group should be evaluated prior to iodine therapy to determine their ovarian reserve level so that if their AMH level is not suitable, they may need to consult with a fertility preservation specialist.
Similar content being viewed by others
Background
Anti-Müllerian hormone (AMH) is a measure of ovarian reserve and is secreted from granulosa cells in the early stages of follicle formation to large antral follicle [1]. The level of the hormone could not be detected from the birth of a female infant to the age of her puberty. The level of the hormone increases and reaches its highest level at the end of her puberty. The ovarian follicular reserve declines with aging, and at the point of menopause, its level is no longer detectable [2]. A practical advantage of this technique is that it can be measured independently of the menstrual cycle and gonadotropin levels [3]. Measuring the serum level of AMH is used as an index to evaluate the ovarian reserve in pre-IVF and polycystic ovary syndrome examination [4]. The normal serum level of AMH is around 1 to 3.5 ng/ml [4].
Thyroid cancer is the most common malignancy of the endocrine system, which is three times more common in women than in men [5]. According to the guidelines of the American Thyroid Association in 2017, since pregnancy within 6 months after iodine treatment is associated with an increased chance of complications such as anomalies and miscarriage, it is not recommended to become pregnant during this period [6, 7].
Based on our knowledge, four prospective studies [8,9,10,11] and one retrospective study [12] have examined the changes in AMH levels at different time points after iodine therapy in cancer patients. In three primary studies, evidence of a decrease in AMH levels after iodine therapy has been reported [8,9,10]. Since the studies are limited and there is still a debate in this field, therefore the present study was conducted with the primary aim of investigating the effect of iodine therapy on ovarian reserve by measuring the blood level of anti-Müllerian hormone.
Methods
Study protocol
This prospective cohort study was scheduled in the Nuclear Medicine Department of the University-Affiliated Center (Imam Khomeini Hospital). The study protocol was approved by the Islamic Azad University, Tehran Medical Sciences Branch Ethics Committee, and a written informed consent was obtained from each patient who participate in this study. The 60 women at the age of 18–35 years old with differentiated thyroid carcinoma diagnoses who were admitted to the Nuclear Medicine Department for iodine therapy from December 2018 to December 2019 were included and followed up 1 year after the administration of RAI. The exclusion criteria were as follows: AMH level less than 1 ng/ml; existing other malignancies; advanced renal, hepatic, or cardiac disease; previous history of radiation exposure to the pelvis; and previous pelvic surgery (with the exception of cesarean section).
The high-dose (100 mCi) radioactive iodine (RAI) treatment was carried out for all patients. The preparation for RAI therapy was performed with thyroid hormone withdrawal. Each woman underwent a baseline serum AMH measurement before radioiodine therapy. A detailed general and reproductive health questionnaire included questions regarding menstruation, pregnancies, comorbidities, and smoking which were provided and asked from each patients during the first visit. Each woman was then requested to return to the endocrinology clinic at Imam Khomeini Hospital for AMH measurements at 3, 6, and 12 months after the RAI therapy. All of AMH measurements were performed in the laboratory of Imam Khomeini Hospital.
AMH level measurements
Participants provided fasting blood samples from a peripheral vein during the follicular phase (days 3–5). Serums were separated and stored at − 80 °C until analysis in order to synchronize time and a specialist who perform the AMH assays. Therefore, all the AMH measurements were carried out at end of sampling by using an AMH Gen II enzyme-linked immunosorbent assay (Beckman Coulter, Brea, CA, USA). The laboratory specialist performed the analysis procedure on the basis of the manufacturer’s instruction. AMH measurement tests for patients were without complications and free of charge.
Statistical analysis
The sample size of 60 subjects was calculated based on the Yaish et al. study that reported the 1.35 ± 1 ng/ml reduction in AMH level after RAI therapy by using the quantitative attribute estimation formula in a population with an acceptable error of 0.25 from the standard deviation (d = 0.25) and confidence interval 95%. Frequency table was used to describe qualitative variables, and mean and standard deviation were used to present quantitative variables. The Student t-test and correlation statistical tests were applied to analyze the data.
Results
The statistical analysis showed that the mean age of the patients was 29.53 ± 4.53 years (19 to 35 years), and the body mass index (BMI) of the patients before starting iodine therapy ranged from 21 to 37 kg/m2 with a mean of 27.65 ± 3.89. The range of menarche age of the patients was from 8 to 14 years with a mean of 10.38 ± 1.49 years. Out of 60 patients, 18.3% had AUB. Forty-one (68.3%) patients had no history of pregnancy. The mean of AMH levels before iodine therapy was 2.25 ± 0.55 ng/ml in the range of 1.3–3.8 ng/ml. The mean of AMH decreased to 1.15 ± 0.35 ng/ml 3 months after iodine treatment. After 6 months of iodine therapy, it increased again to 1.58 ± 0.47 ng/ml, and 12 months after iodine therapy, it reached 1.94 ± 0.58 ng/ml.
As observed in the diagram, the level of AMH decreased sharply after 3 months of iodine therapy, and then it increased with the passage of time; however, it did not reach the initial level. The mean level of AMH decreased by 1.1 ng/ml after 3 months of iodine therapy, 0.67 ng/ml 6 months after iodine therapy, and 0.31 ng/ml 12 months after iodine therapy compared to before iodine therapy. A significant correlation was observed between the values of AMH reduction in 3, 6, and 12 months after iodine therapy compared to the initial level (all P-values < 0.001). In other words, the amount of AMH decreased by 49.05%, 29.55%, and 13.58%, respectively, in 3, 6, and 12 months after iodine therapy compared to the initial levels before iodine therapy (Fig. 1).
A significant reverse relationship between age and AMH level was observed (P < 0.001, Table 1). A statistically significant inverse correlation was observed between the patient’s BMI and the AMH level 3 months after the iodine treatment (P-value = 0.026), while there was no statistically significant relationship between AMH levels at baseline, 6 months, and 12 months after iodine therapy and BMI before starting iodine therapy (Table 1). Four patients (6.7%) were smokers, and the mean level of AMH before iodine therapy in smokers was 2.58, which was 2.22 in the non-smoker group. This higher AMH level is due to the higher prevalence of this variable in younger people. Statistically, no significant relationship between smoking and AMH level was observed at the time points of the measurements (P = 0.22, P = 0.09, P = 0.24, and P = 0.27, respectively). There was no statistically significant relationship between the AMH level and menarche age of the patients (Table 1). Eleven patients had AUB (18.3%), and the mean of baseline AMH levels and then 3, 6, and 12 months after iodine treatment in these patients were 2.27, 1.19, 1.63, and 1.96, respectively. No statistically significant relationship between AMH hormone level and AUB was observed (P = 0.88, P = 0.66, P = 0.73, and P = 0.91, respectively). The number of previous pregnancies had a significant relationship with the initial AMH level (P-value = 0.048), but its relationship was not significant in 3, 6, and 12 months after iodine therapy (P = 0.09, P = 0.06, and P = 0.13, respectively).
Discussion
In present study, AMH decreased by 49.05%, 29.55%, and 13.58%, respectively, in 3, 6, and 12 months after iodine therapy compared to baseline levels before iodine therapy. Similar to chemotherapy and chemotherapy, iodine therapy is also associated with a decrease in ovarian reserve, so patients should be referred for fertility preservation counseling before iodine therapy. In the majority of the previous studies, the level of AMH decreased in first month after iodine treatment and then increased. Due to the difference between the kits used in different studies and different units of AMH, the changes are not comparable in terms of quantity; however, the effect of iodine therapy on the ratio of reduction or rising of AMH after iodine therapy can be compared.
As it has already been approved, AMH levels decrease with age. In Yaish et al. study [8], the amount of AMH reduction in women over 35 years old compared to women under 35 years old was significant (63.7 ± 18.5 pmol/l vs. 29.2 ± 33.1 pmol/l), which indicates the effect of age on AMH changes. In Giusti et al. study [12], the patients who underwent thyroidectomy along with iodine therapy were compared to the patients who underwent only thyroidectomy, and they reported that the mean level of AMH in the iodine therapy group was 10.7 pmol/l versus 17.5 pmol/l in the control group (only thyroidectomy). The fertility rate was nonsignificantly 62% in the iodine-treated group and 61% in the control group, and the abortion rate was 18% and 26%, respectively. In the present study, we did not include patients older than 35 years to be able to examine the effect of iodine therapy more precisely.
Elsewhere, Wu et al., in a retrospective study, evaluated 25,333 women who underwent iodine therapy for thyroid cancer between in terms of fertility rate and mean time to live birth after iodine therapy. The results showed that iodine therapy had no effect on women’s fertility [13].
In contrast to the present study, Mittica and colleagues in a cross-sectional prospective study have evaluated the changes of AMH level in three groups of thyroid surgery alone, thyroid surgery along with iodine therapy and the control group, after 2 years, and they found no significant changes in the level of AMH between the two groups with and without RAI therapy [11]. Also, the two groups did not differ significantly in terms of the age of menopause and the incidence of abnormal uterine bleeding [11].
In agreement to our findings, Yaish et al. [8] demonstrated that the hormone level decreased dramatically from 3.25 to 1.9 ng/ml in the first 3 months. After 1 year, 82% of patients had AMH levels lower than their pre-iodine therapy level, and serum AMH was still 32% lower than prior to iodine therapy. Furthermore, Evranos et al. reported that the AMH level is strongly reduced 6 months after RAI treatment compared to before, and no significant difference was found between the time of AMH measurement and its reduction rate [9]. Van Velsen and co-workers after longitudinal study of 65 patients with DTC who treated with total thyroidectomy and a single RAI therapy concluded that AMH concentrations significantly decreased during the first year after initial therapy, and then they remained fixed. In patients receiving multiple RAI therapies, a further reduction was observed [14]. Age at baseline significantly impressed AMH change over time. These findings recommend a less aggressive RAI therapy in low-risk patients as is advocated in the current American Thyroid Association guidelines, especially in women older than 35 years with the desire to have a child [14].
With the expansion of cancer treatments, preserving fertility has become very important for patients of reproductive age. Studies on the effect of GnRH-a (triptorelin) and GnRH-ant (cetrorelix) on AMH changes show that a high dose of GnRH-ant causes more AMH expression, but GnRH agonist had no significant effect [15]. In Leonard et al. study, it was shown that goserelin prevents premature ovarian failure in women with breast cancer undergoing chemotherapy, but it does not make a significant difference in their AMH levels [16]. The meta-analysis study shows the positive effects of GnRH agonist on the prevention of premature ovarian failure and amenorrhea, as well as higher pregnancy rates in this group of patients [17].
The strengths of the current study are reasonable sample size and its prospective design in women less than 35 years old. It is worth noting that the limitation of our study is not having a control group (patients without chemotherapy), so we could not examine the independent effect of RAI therapy on AMH level change. Due to financial and timing shortages, we could not refer patients for ultrasound examination to determine the antral follicles count (AFC); therefore, it is suggested that in future studies, the changes of other ovarian reserve tests such as the AFC and follicle-stimulating hormone level be investigated over a year and compared with an age-matched control group.
Conclusion
Considering the effect of iodine therapy on the reduction of AMH levels, it is recommended that women of reproductive age group should be evaluated prior to iodine therapy to determine their ovarian reserve level so that if their AMH level is not suitable, they may need to consult with a fertility preservation specialist.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding authors on reasonable request.
Abbreviations
- AMH:
-
Anti-Müllerian hormone
- RAI:
-
Radioactive iodine
- AUB:
-
Abnormal uterine bleeding
- GnRH:
-
Gonadotropin-releasing hormone
References
Kwee J, Schats R, McDonnell J, Themmen A, de Jong F, Lambalk C (2008) Evaluation of anti-Müllerian hormone as a test for the prediction of ovarian reserve. Fertil Steril 90(3):737–743
Dólleman M, Verschuren WM, Eijkemans MJ, Broekmans FJ, Van Der Schouw YT (2015) Added value of anti-Müllerian hormone in prediction of menopause: results from a large prospective cohort study. Hum Reprod 30(8):1974–1981
La Marca A, Stabile G, Artenisio AC, Volpe A (2006) Serum anti-Mullerian hormone throughout the human menstrual cycle. Hum Reprod 21(12):3103–3107
Aghssa MM, Tarafdari AM, Tehraninejad ES, Ezzati M, Bagheri M, Panahi Z et al (2015) Optimal cutoff value of basal anti-mullerian hormone in iranian infertile women for prediction of ovarian hyper-stimulation syndrome and poor response to stimulation. Reprod Health 12(1):1–8
Furuya-Kanamori L, Bell KJ, Clark J, Glasziou P. Prevalence of differentiated thyroid cancer in autopsy studies over six decades: a meta-analysis. J Clin Oncol. 2016.
Alexander EK, Pearce EN, Brent GA, Brown RS, Chen H, Dosiou C et al (2017) 2017 Guidelines of the American Thyroid Association for the diagnosis and management of thyroid disease during pregnancy and the postpartum. Thyroid 27(3):315–389
Blackburn BE, Ganz PA, Rowe K, Snyder J, Wan Y, Deshmukh V et al (2018) Reproductive and gynecological complication risks among thyroid cancer survivors. J Cancer Surviv 12(5):702–711
Yaish I, Azem F, Gutfeld O, Silman Z, Serebro M, Sharon O et al (2018) A single radioactive iodine treatment has a deleterious effect on ovarian reserve in women with thyroid cancer: results of a prospective pilot study. Thyroid 28(4):522–527
Evranos B, Faki S, Polat SB, Bestepe N, Ersoy R, Cakir B (2018) Effects of radioactive iodine therapy on ovarian reserve: a prospective pilot study. Thyroid 28(12):1702–1707
Lin R, Miao W. The effect of radioiodine therapy on ovarian function in patients with differentiated thyroid carcinoma. Soc Nuclear Med; 2019.
Mittica M, Dotto A, Comina M, Teliti M, Monti E, Giusti M (2020) Cross-sectional and prospective study on anti-Müllerian hormone changes in a cohort of pre-menopausal women with a history of differentiated thyroid cancer. Thyroid Res 13(1):1–9
Giusti M, Mittica M, Comite P, Campana C, Gay S, Mussap M (2018) Anti-Müllerian hormone in pre-menopausal females after ablative radioiodine treatment for differentiated thyroid cancer. Endocrine 60(3):516–523
Wu JX, Young S, Ro K, Li N, Leung AM, Chiu HK et al (2015) Reproductive outcomes and nononcologic complications after radioactive iodine ablation for well-differentiated thyroid cancer. Thyroid 25(1):133–138
van Velsen EF, Visser WE, van den Berg SA, Kam BL, van Ginhoven TM, Massolt ET et al (2020) Longitudinal analysis of the effect of radioiodine therapy on ovarian reserve in females with differentiated thyroid cancer. Thyroid 30(4):580–587
Dong M, Huang L, Wang W, Du M, He Z, Mo Y et al (2011) Regulation of AMH and SCF expression in human granulosa cells by GnRH agonist and antagonist. Pharmazie 66(6):436–439
Leonard R, Adamson D, Bertelli G, Mansi J, Yellowlees A, Dunlop J et al (2017) GnRH agonist for protection against ovarian toxicity during chemotherapy for early breast cancer: the Anglo Celtic Group OPTION trial. Ann Oncol 28(8):1811–1816
Senra JC, Roque M, Talim MC, Reis FM, Tavares RL (2018) Gonadotropin-releasing hormone agonists for ovarian protection during cancer chemotherapy: systematic review and meta-analysis. Ultrasound Obstet Gynecol 51(1):77–86
Acknowledgements
We extend thanks to all the women who participated in this study.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
AH and ZL designed the research. AH and ZL contributed in patient’s selection, data collection, analysis, interpretation of data, and manuscript writing/editing.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the 1964 Helsinki Declaration and its later amendments (ethics approval number: IR.IAU.TMU.REC.1399.188). The eligible patients signed written informed consent prior to participation in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hosseini, A., Lavasani, Z. The effect of radioactive iodine therapy on anti-Müllerian hormone changes in women with thyroid cancer at reproductive age: a prospective study. Middle East Fertil Soc J 28, 24 (2023). https://doi.org/10.1186/s43043-023-00147-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43043-023-00147-5